Clinical Outcomes of Pancreatic Head Malignancies in Tanzania
Clinical Profile and Outcome of Pancreatic Head Malignancies Among Patients at a Tertiary Referral Hospital A Seven-year Retrospective Review
Kennedy Misso, MD¹˒², Comfort M. Takang, MD, MPH³, Kondo Chilonga¹˒², Mujaheed Suleman¹, Yotham Gwanika, MSc ¹, Pius Aloyce¹˒², Glory Makupa¹˒², Augustine Musyoka¹˒², Arkadiusz Z. Dudek, MD, PhD ⁴, Randy Hurley, MD ⁵, Furaha Serventi, MD ¹˒²
- Kilimanjaro Christian Medical Centre (KCMC), Moshi, Tanzania
- KCMC University (KCMCU), Moshi, Tanzania
- University of Minnesota Department of Haematology, Oncology, and Transplant, Minneapolis, Minnesota, USA
- Division of Medical Oncology, Department of Medicine, Mayo Clinic, Rochester, Minnesota, USA
- Regions Hospital, HealthPartners System, St Paul, Minnesota, USA
OPEN ACCESS
PUBLISHED: 31 October 2025
CITATION:MISSO, Kennedy et al. Clinical Profile and Outcome of Pancreatic Head Malignancies Among Patients at a Tertiary Referral Hospital – A Seven-year Retrospective Review. Medical Research Archives, [S.l.], v. 13, n. 10, oct. 2025. Available at: <https://esmed.org/MRA/mra/article/view/6916>.
COPYRIGHT: © 2025 European Society of Medicine. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
DOI : https://doi.org/10.18103/mra.v13i10.6916.
ISSN 2375-1924
Abstract
Background: Malignancies of the head of the pancreas pose a significant global challenge due to their late presentation and the disease’s aggressive nature. Modifiable risk factors, such as obesity, cigarette smoking, and alcohol consumption, are expected to increase, leading to a higher incidence of pancreatic cancer. Although the incidence of pancreatic cancer in Africa is expected to increase, data on pancreatic head malignancies in the region are abysmal. This study aimed to assess the current status of pancreatic cancer diagnosis and treatment options in Northern Tanzania.
Methods: We conducted a retrospective hospital-based study from January 2016 to December 2023 at a tertiary hospital in northern Tanzania. We aimed to investigate clinical presentation, management outcomes, and survival analysis. We retrieved data on patients diagnosed with pancreatic head tumours from the cancer registry. Data on demographics, clinical features, diagnostics, treatment, and outcomes were extracted from the cancer registry and hospital records. Descriptive statistics are presented as means with standard deviations (SD) or medians with interquartile ranges (IQR) for continuous variables, and frequencies with percentages for categorical variables. The chi-square (χ²) test assessed the association between categorical variables, while the grouped sample t-test or one-way ANOVA evaluated continuous outcomes at a 95% confidence interval. Significance was set at P < 0.05. Survival was analysed using the Kaplan Meier method and log-rank tests, with Cox regression used to identify independent predictors of mortality. Ethical approval was obtained from the institutional review board, with consent waived due to the study’s retrospective nature.
Results: A total of 132 patients were included in this study, with a mean age of 61 years and a slight male predominance of 56.1%. Despite the low rate of chemotherapy administration (15.9%), treatment was associated with improved 30-day overall survival (OS 77.7% for recipients vs. 60.4% for non-recipients). Chronic pancreatitis was significantly associated with increased mortality (HR 5.92, p=0.019).
Conclusion: Our study reveals a high rate of late-stage presentations, limited diagnostic and treatment options, and markedly poor survival outcomes for patients with tumours of the head of the pancreas in northern Tanzania. The findings underscore the necessity for enhanced diagnostic and treatment strategies for pancreaticobiliary malignancies, given the significant mortality risks linked to certain factors and the limited use of invasive treatments. Further research is essential to develop more cost-effective interventions and enhance patient outcomes.
Keywords
Pancreatic cancer, head malignancies, Tanzania, survival analysis, treatment outcomes
Introduction
Malignancies of the pancreas are aggressive cancers that are often diagnosed late, resulting in a poor prognosis. Modifiable risk factors like obesity, alcohol consumption, and smoking contribute to an increase in global pancreatic cancer rates. By 2025, pancreatic cancer is projected to become the third leading cause of cancer-related deaths in Europe, with an expected increase in incidence in Africa from 2018 to 2040. It is usually diagnosed at advanced stages and has aggressive characteristics, leading to a dismal prognosis. Worldwide, pancreatic cancer leads to nearly as many deaths as diagnosed cases, with 466,003 deaths (94%) compared to 495,773 diagnosed cases.
It is currently the seventh most common cause of cancer-related deaths among both men and women, and the five-year survival rate for this type of cancer is less than 10%. Over the past decade, an upward trend in pancreatic cancer cases has been observed worldwide. Global Cancer Observatory (GLOBOCAN) estimates that pancreatic cancer will be the leading cause of cancer death by 2025, as more progress is made on other malignancies, such as breast and lung cancer. Pancreatic cancer seems to be lagging in more effective ways of early diagnosis and effective treatment that carry less morbidity.
Between 2020 and 2040, Africa is expected to see the most significant surge in cancer incidences and deaths, outpacing all other global regions. In Tanzania, in 2020, 510 new cases of pancreatic malignancies were diagnosed annually, resulting in 494 deaths. Our objective was to establish a foundational understanding of pancreatic head cancers in northern Tanzania. We aimed to investigate the clinical presentation, management provided, and outcomes of pancreatic head malignancies at a tertiary hospital.
Methodology
This retrospective cohort study was conducted at Kilimanjaro Christian Medical Centre (KCMC), a tertiary referral hospital in northern Tanzania, spanning the period from January 1, 2016, to December 31, 2023. KCMC serves as a zonal tertiary referral hospital with a catchment population of 15 million. The study period (2016-2023) was chosen to ensure data completeness and reflect the era when cancer registry systems and electronic medical records had significant improvement.
All patients aged 18 years and above with histologically or radiologically confirmed malignancies of the pancreatic head, and complete demographic, clinical, and outcome data, were included. Those with tumours of the pancreatic body or tail, secondary pancreatic involvement from other primaries, or incomplete essential records were excluded. Patients were identified through the KCMC Cancer Registry and hospital medical records, and data were abstracted using a standardised form before being entered into a secure REDCap database.
Variables collected included demographics (age, sex, residence, insurance status), clinical features (presenting symptoms, comorbidities, Eastern Cooperative Oncology Group (ECOG) performance status, alcohol use, chronic pancreatitis), diagnostic modalities such as histopathology, computed tomography (CT), and magnetic resonance imaging (MRI), treatment modalities (surgical resection, biliary bypass, chemotherapy, palliative surgery, or best supportive care), and outcomes (survival status, date of death, or last follow-up).
Diagnosis was confirmed by histology, where available, or by imaging (contrast-enhanced CT or MRI) demonstrating a pancreatic head mass with malignant features. Patients lost to follow-up were censored at the date of last contact. As this was a retrospective cohort study, the sample size was determined by the number of eligible cases during the study period. All patients meeting the inclusion criteria were included to maximise statistical power.
Data analysis was performed using Stata version 18 (Stata Corp LLC, College Station, TX, USA). Descriptive statistics are presented as means with standard deviations (SD) or medians with interquartile ranges (IQR) for continuous variables, and frequencies with percentages for categorical variables. Comparative analyses were conducted using chi-square tests for categorical variables and independent t-tests or one-way ANOVA for continuous variables. Survival outcomes were assessed using Kaplan Meier curves, with log-rank tests for group comparisons, and Cox proportional hazards regression was applied to identify independent predictors of mortality, reporting hazard ratios (HR) with 95% confidence intervals (CI). Statistical significance was set at p < 0.05. Ethical approval was obtained from the Kilimanjaro Christian Medical University College Research Ethics Committee (CRERC), and patient confidentiality was maintained by de-identifying all records before analysis, with the requirement for informed consent waived due to the retrospective design.
Results
THE CLINICODEMOGRAPHIC CHARACTERISTICS
The mean age of patients at diagnosis was 61.01 years, with a standard deviation of 14.20 years. The majority, 77.27%, were over 30 years old, and 56.1% were male. 28.8% of patients had unknown ECOG scores, while others were categorised as ECOG PS 1 (32.6%). Chronic pancreatitis was present in 3.8% of patients, and the vast majority (96.2%) had no history of this condition.
| Variable | Frequency (n) | Percentage (%) | |
|---|---|---|---|
| Age Category | ≤30 | 30 | 22.7 |
| >30 | 102 | 77.3 | |
| Gender | Female | 58 | 43.9 |
| Male | 74 | 56.1 | |
| Alcohol Use | No | 77 | 58.3 |
| Yes | 55 | 41.7 | |
| Performance Status (ECOG) | ECOG PS 0 | 1 | 0.8 |
| ECOG PS 1 | 43 | 32.6 | |
| ECOG PS 2 | 31 | 23.5 | |
| ECOG PS 3 | 18 | 13.6 | |
| ECOG PS 5 | 1 | 0.8 | |
| Undocumented ECOG PS | 38 | 28.8 | |
| Chronic Pancreatitis | No | 127 | 96.2 |
| Yes | 5 | 3.8 |
TREATMENT RECEIVED
Table 2 summarises the treatment modalities received by patients with pancreatic head malignancies. The majority of patients (84.1%) did not receive chemotherapy, while only 15.9% underwent systemic treatment. Biliary bypass was performed in 41.7% of patients, reflecting its role as the most common intervention in this cohort.
| Variable | Frequency (n) | Percentage (%) | |
|---|---|---|---|
| Biliary Bypass | No | 77 | 58.3 |
| Yes | 55 | 41.7 | |
| Chemotherapy | No | 111 | 84.1 |
| Yes | 21 | 15.9 |
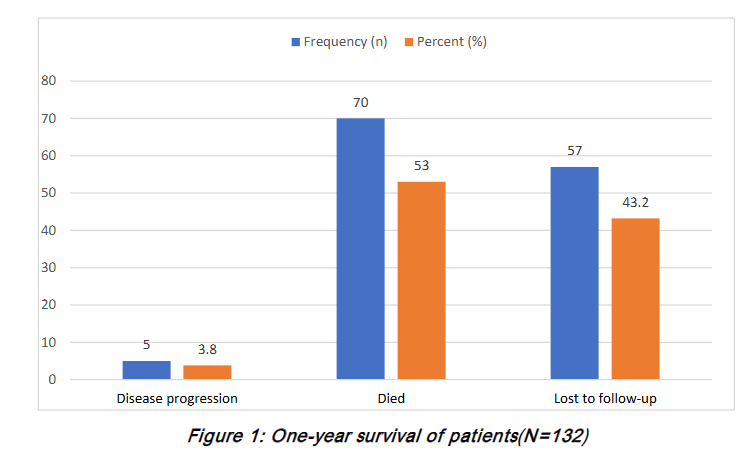
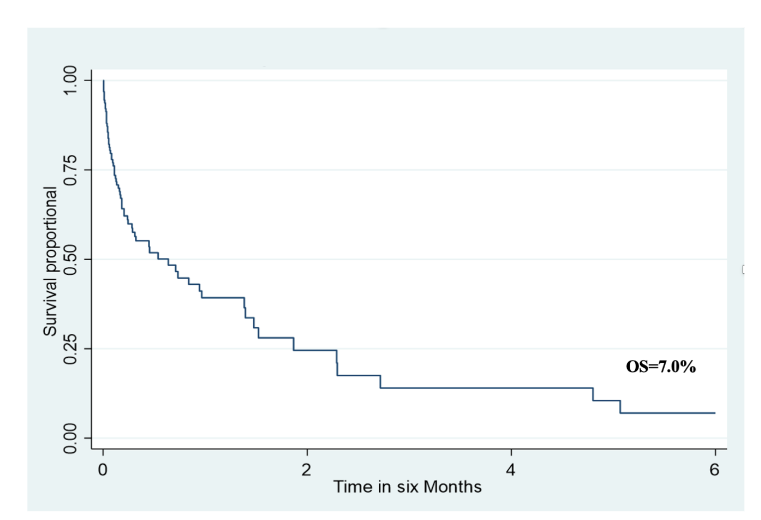
The Median Survival in this study was 33 days (IQR 30-80). Figure 1 displays the one-year survival of patients after diagnosis. The low frequency of disease recorded is likely related to a lack of imaging follow-up, as most patients did not receive any treatment or subsequent scans after initial diagnosis. The six-month overall survival in this study was 7.0%.
FACTORS ASSOCIATED WITH MORTALITY AMONG PATIENTS
Table 3 shows that chronic pancreatitis and exposure to surgery had a significant association with increased mortality. Other factors, such as age, gender, health insurance, alcohol use, performance status, and chemotherapy, did not show significant associations with mortality.
| Variable | Crude HR (95% CI) | p-value | Adjusted HR (95% CI) | p-value | |||
|---|---|---|---|---|---|---|---|
| Age at diagnosis | ≤30 ref | >30 | 0.80 (0.46 – 1.41) | 0.442 | 1.30 (0.65 – 2.60) | 0.456 | |
| Gender | Female ref | Male | 0.89 (0.55 – 1.43) | 0.635 | 0.77 (0.43 – 1.38) | 0.379 | |
| Health Insurance | No | 1.06 (0.67 – 1.70) | 0.795 | 1.07 (0.61 – 1.88) | 0.803 | Yes ref | |
| Alcohol Use | No ref | Yes | 0.91(0.56 – 1.48) | 0.695 | 0.85 (0.48 – 1.50) | 0.566 | |
| Performance Status | ECOG PS 0 ref | ECOG PS 1 | 1.28 (0.17 – 9.48) | 0.808 | 4.53 (0.20 – 102.31) | 0.342 | |
| ECOG PS 2 | 1.06 (0.14 – 8.17) | 0.956 | 4.50 (0.20 – 103.10) | 0.346 | |||
| ECOG PS 3 | 1.23 (0.16 – 9.52) | 0.842 | 5.04 (0.22 – 117.01) | 0.313 | |||
| ECOG PS 4 | 3.25 (0.20 – 53.35) | 0.409 | 38.32 (0.79 – 1864.71) | 0.066 | |||
| Unknown ECOG PS | 1.66 (0.21 – 12.85) | 0.628 | 15.79 (0.70 – 353.73) | 0.082 | |||
| Chronic Pancreatitis | No ref | Yes | 1.25 (0.39 – 4.00) | 0.708 | 5.92 (1.35 – 26.00) | 0.019 | |
| Chemotherapy | No ref | Yes | 0.87 (0.51-1.46) | 0.595 | 0.68 (0.34 – 1.35) | 0.273 |
Discussion
The mean age of the patients was 61.01 years, with 77.27% being over 30 years of age a slight male predominance, with males comprising 56.1% of the patients. A history of ever using alcohol was reported in 41.7%. These findings are similar to those of other epidemiological studies, which report a median age of presentation in the sixth and seventh decades of life, with a rare diagnosis before the age of 55 years. GLOBOCAN statistics report pancreatic cancer to be more common in males, with the incidence in Eastern Europe of 9.9/100,000 population.
Globally, pancreatic cancer shows a consistent male predominance, with men experiencing both higher incidence and mortality compared to women. Men accounted for ~53% of new cases worldwide (246,840 vs. 219,163 in women), with an age-standardised incidence rate (ASR) of 5.5 per 100,000 in men versus 4.0 per 100,000 in women. In Western countries, this disparity is more pronounced: in the United States, SEER data report ASRs of 9.8 in men and 7.5 in women, while in Europe, countries such as France and Germany show male rates exceeding 10 per 100,000 compared to 7-8 in women.
Our study reports a six-month overall survival rate of 7%, with a median survival of 33 days (interquartile range, 30-80 days). These outcomes reflect inferior survival, most likely due to the advanced stage at presentation, which severely limits the feasibility of both surgical and systemic interventions. Similar challenges have been documented in neighbouring regions. At Kenyatta National Hospital, Moraa and Degu’s five-year retrospective study reported that most patients presented with advanced disease, and few underwent potentially curative resection. Although their mean and median survival times (48.7±9.7 and 39±23.9 months, respectively) were longer, these estimates were influenced by small sample size, follow-up limitations, and methodological differences.
In contrast, extensive international population-based analyses demonstrate improved survival when patients are diagnosed earlier and have access to surgery. Huang et al. reported three-year survival rates of 23 to 39 per cent among resected stage I-II patients younger than 60 years, 16% to 31% in those aged 60 to 69, and 17 to 30 percent in those aged 70 years or older. In advanced age groups, perioperative survival exceeded 94%, indicating that with sufficient infrastructure and perioperative care, surgery provides substantial benefit across age groups. In comparison, survival in unresected or advanced-stage disease rarely exceeds 11%, even in modern chemotherapy, highlighting the critical importance of timely resection.
Our findings are consistent with reports from across Africa and beyond, where most patients present at an advanced stage. In Ethiopia, Dinagde and Abubeker found that nearly 81.8% of patients underwent only palliative procedures, underscoring the limited role of curative resection in the region. A Moroccan single-centre retrospective cohort likewise showed that only 19.8% were resectable at diagnosis, reflecting the global challenge of late presentation. In contrast, U.S. Surveillance, Epidemiology, and End Results (SEER) data show a 5-year relative survival of approximately 12% and steadily improving outcomes with multimodal therapy, though still among the lowest of all major cancers. Taken together, these comparisons reinforce that the Tanzanian experience is part of a broader sub-Saharan African pattern of delayed diagnosis, low resection rates, and reliance on palliative surgery, while also highlighting the widening survival gap with high-income countries.
Within our patient group, the most common surgery was a double bypass, a cholecystectomy combined with gastrojejunostomy and Braun’s anastomosis carried out via Kocher or midline incisions. Such surgical procedures continue to play a vital role in palliation, particularly in contexts where advanced disease is prevalent and minimally invasive techniques are not widely accessible. Progress in endoscopic and interventional radiology has led to substantial gains in both diagnostic precision and palliative care. Techniques like endoscopic ultrasound (EUS) now offer detailed imaging and enable fine-needle aspiration, supporting earlier identification of lesions missed by standard imaging and providing tissue samples for histological analysis to inform treatment strategies. Procedures such as Endoscopic Retrograde Cholangiopancreatography (ERCP) and Percutaneous Transhepatic Biliary Drainage (PTBD) have become first-line interventions for biliary decompression, thereby lessening the dependence on open operations and permitting a more timely commencement of systemic therapies.
Published literature supports this paradigm shift. Inamdar et al. used a large national cohort to demonstrate that ERCP is associated with lower complication rates, shorter hospital stays, and reduced costs compared to PTBD. However, both methods are effective in relieving obstruction. In resource-limited settings, surgical bypass remains essential, as the absence of ERCP and Interventional radiology makes surgery the only option in palliating biliary obstruction. Although invasive and limited by the patient’s physical and performance status, surgery offers an advantage in relieving gastric obstruction in some cases where the tumour is bulky. Mutombo et al. found that double or triple bypass procedures continue to provide effective palliation of both biliary and gastric outlet obstruction, improving oral intake and quality of life despite limited survival gains.
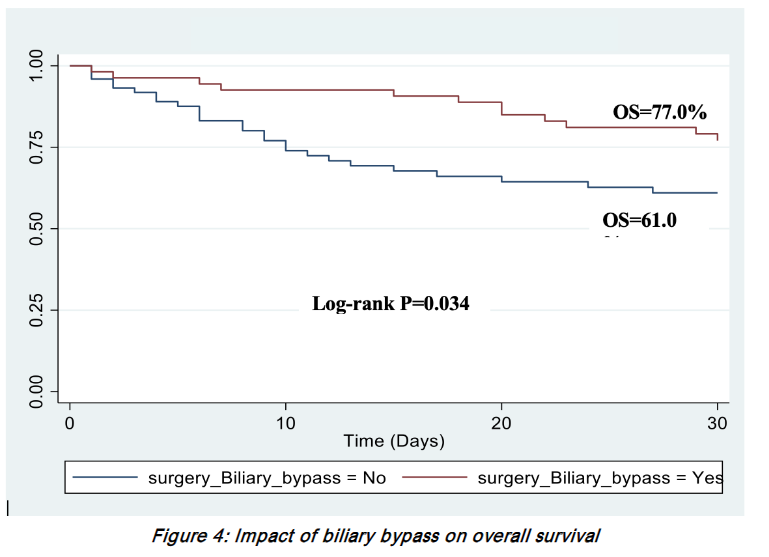
Survival analysis in our cohort demonstrated that patients who underwent surgical biliary bypass had statistically significant survival advantages compared to those who did not undergo surgery. This likely reflects the importance of enterobiliary drainage in optimising patients for chemotherapy, as relief of jaundice is often required before systemic treatment can be initiated. Taken together, these results underscore the need for context-sensitive treatment strategies. In high-resource settings, minimally invasive approaches such as EUS, ERCP, and PTBD should be prioritised due to their safety profile and ability to facilitate systemic therapy. In contrast, in resource-limited environments, surgical bypass particularly double bypass anastomosis remains a vital option for comprehensive palliation.
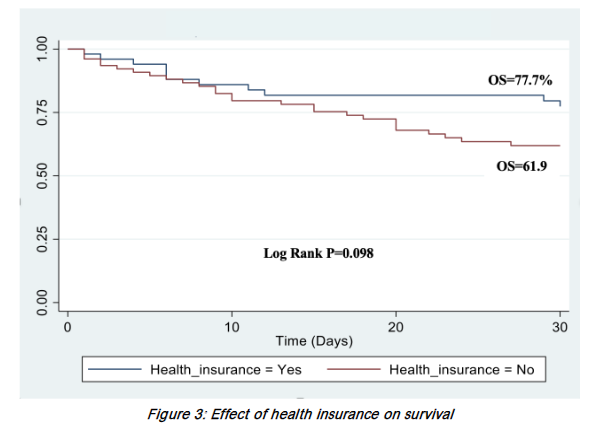
Age, gender, and health insurance status had no statistically significant effect on one-month survival rates. Overall survival (OS) for insured patients was 77.7% compared to 61.9% for non-insured patients, although the difference was not statistically significant. This suggests that having health insurance did not affect general health-seeking behaviour in this study, although the study was not powered to detect significant differences. On the contrary, a prospective study conducted in Massachusetts, United States, found that improved healthcare coverage led to increased pancreatic cancer resections and better outcomes from cytoreductive therapy. A systematic review in low- and middle-income countries reported inconsistent findings on the positive association between healthcare coverage and access to care. These findings suggest that while insurance may facilitate initial access to care, its effect on complex cancer outcomes like pancreatic malignancies is limited unless paired with diagnostic and treatment infrastructure.
Chronic pancreatitis was statistically significantly associated with a mortality-adjusted HR of 5.92. Although our analysis demonstrated that chronic pancreatitis was statistically significantly associated with a mortality-adjusted HR of 5.92 (P = 0.019), this finding must be interpreted with caution. The number of patients with a prior history of pancreatitis in our cohort was too small, which limits the precision of the estimate and raises the possibility of overestimation of risk. Furthermore, as highlighted in literature, there is a recognised risk of misclassification at the first clinical presentation, where an initial episode of pancreatic cancer may be misdiagnosed as acute or chronic pancreatitis due to overlapping clinical and radiological features.
In a prospective multicenter cohort of 2015 patients across six European countries, the cumulative incidence of chronic pancreatitis increased to 1.8% and 4% at 10- and 20 years post-diagnosis, respectively. The risk was independent of sex, country of origin, and gender. A systematic review and meta-analysis involving 13 studies found an increased association between chronic pancreatitis and pancreatic cancer. They recommended a close follow-up in the first two years to minimise the risk of overlooking malignancy. In the International Pancreatic Cancer Consortium (PanC4), a large case-control study involving 5048 cases and 10,947 controls. Chronic pancreatitis had an odds ratio of 2.71 (95% CI: 1.96-3.74) in follow-up of more than two years. It mostly affected patients <65 years. Our findings highlight the need for improved diagnostic protocols and awareness of chronic pancreatitis as a potential precursor or confounding factor in pancreatic cancer care across sub-Saharan Africa.
Despite these advances, only 15.9% of patients in this study received chemotherapy, underscoring the challenges of advanced disease presentation and systemic barriers to care. Many patients were ineligible for systemic therapy due to poor postoperative recovery, while others declined treatment because of financial limitations. Although the adjusted hazard ratio for chemotherapy was 0.68 (P = 0.273), it did not reach statistical significance. The observed trend suggests a potential survival benefit consistent with the global evidence. Pancreatic cancer remains among the most lethal malignancies, with limited therapeutic options and poor overall survival despite recent advances in systemic therapy. Lai et al. reported that regimens such as FOLFIRINOX and gemcitabine-based combinations can improve outcomes, but their use is frequently limited by toxicity and patient performance status. Additionally, cachexia and malnutrition, which are highly prevalent in pancreatic cancer, have been shown to significantly reduce chemotherapy tolerance and efficacy significantly.
Expanding access to chemotherapy calls for integrated surgical and oncological services, improvements in supportive care, nutritional interventions, and financial safeguards. Such initiatives are vital to guarantee effective palliation and enable access to systemic therapy, both of which are central to enhancing survival rates in pancreatic cancer.
Conclusion
The findings in this study highlight the need for improved diagnostic and treatment strategies for pancreaticobiliary malignancies, considering the significant mortality risks associated with certain factors and the limited use of invasive treatments. Further research is necessary to develop more cost-effective interventions and improve patient outcomes.
Acknowledgements of research support for the study:
Foundation for Cancer Care in Tanzania (FCCT), Minneapolis, Minnesota, USA, for research funding support.
List of where and when the study has been presented in part elsewhere:
Not applicable.
Disclaimers:
None
References:
- Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71(3):209-249. doi:10.3322/caac.21660
- Ferlay J, Partensky C, Bray F. More deaths from pancreatic cancer than breast cancer in the EU by 2017. Acta Oncol (Madr). 2016;55(9-10):1158-1160. doi:10.1080/0284186X.2016.1197419
- Hu JX, Lin YY, Zhao CF, et al. Pancreatic cancer: A review of epidemiology, trend, and risk factors. World J Gastroenterol. 2021;27(27):4298. doi:10.3748/WJG.V27.I27.4298
- Rawla P, Sunkara T, Gaduputi V. Epidemiology of Pancreatic Cancer: Global Trends, Etiology and Risk Factors. World J Oncol. 2019;10(1):10-27. doi:10.14740/wjon1166
- Klein AP. Pancreatic cancer epidemiology: understanding the role of lifestyle and inherited risk factors. Nat Rev Gastroenterol Hepatol. 2021;18(7):493-502. doi:10.1038/s41575-021-00457-x
- Gaddam S, Abboud Y, Oh J, et al. Incidence of Pancreatic Cancer by Age and Sex in the US, 2000-2018. JAMA – Journal of the American Medical Association. American Medical Association. 2021;326(20):2075-2077. doi:10.1001/jama.2021.18859
- Saad AM, Turk T, Al-Husseini MJ, Abdel-Rahman O. Trends in pancreatic adenocarcinoma incidence and mortality in the United States in the last four decades; a SEER-based study. BMC Cancer. 2018;18(1). doi:10.1186/S12885-018-4610-4
- Moraa F, Degu A. Survival Outcomes Among Pancreatic Cancer Patients at Kenyatta National Hospital. J Gastrointest Cancer. 2022;53(4):958-964. doi:10.1007/S12029-021-00723-W
- Ilic I, Ilic M. International patterns in incidence and mortality trends of pancreatic cancer in the last three decades: A joinpoint regression analysis. World J Gastroenterol. 2022;28(32):4698-4715. doi:10.3748/WJG.V28.I32.4698
- Huang L, Jansen L, Balavarca Y, et al. Stratified survival of resected and overall pancreatic cancer patients in Europe and the USA in the early twenty-first century: A large, international population-based study. BMC Med. 2018;16(1):1-15. doi:10.1186/S12916-018-1120-9/TABLES/4
- Lillemoe KD, Rikkers LF. Pancreaticoduodenectomy: The golden era. Ann Surg. 2006;244(1):16-17. doi:10.1097/01.sla.0000226042.37420.f9
- Cameron JL, He J. Two thousand consecutive pancreaticoduodenectomies. J Am Coll Surg. 2015;220(4):530-536. doi:10.1016/j.jamcollsurg.2014.12.031
- Dinagde TA, Abubeker Z. Surgical management of pancreatic cancer in Tikur Anbessa Specialized Hospital, Addis Ababa, Ethiopia: a 5 years retrospective descriptive study. BMC Surg. 2024;24(1). doi:10.1186/S12893-024-02503-2
- Amri F, Koulali H, Jabi R, et al. Pancreatic cancer: experience from an emerging country in North Africa. J Cancer Res Clin Oncol. 2023;149(15):14297. doi:10.1007/S00432-023-05245-5
- Siegel RL, Miller KD, Wagle NS, Jemal A. Cancer statistics, 2023. CA Cancer J Clin. 2023;73(1):17-48. doi:10.3322/CAAC.21763
- Mutombo FL, Tsandiraki JK, Mchihiyo T, et al. Palliative biliodigestive bypass for unresectable pancreatic malignancy at Kilimanjaro Christian medical centre: a retrospective cross-sectional study. BMC Gastroenterol. 2025;25(1):103. doi:10.1186/s12876-025-03683-8
- Cipolletta L, Rotondano G, Marmo R, Bianco MA, Italian Evidence-Based Gastroenterology & Hepatology Club. Endoscopic palliation of malignant obstructive jaundice: an evidence-based review. Dig Liver Dis. 2007;39(4):375-388. doi:10.1016/j.dld.2006.12.016
- Iruarrizaga E, Azkona E, Martinez M, et al. Percutaneous transhepatic biliary drainage (PTBD) and endoscopic retrograde cholangiopancreatography (ERCP) for malignant obstructive jaundice (OJ) in advanced digestive cancers. Journal of Clinical Oncology. 2011;29(4_suppl):348-348. doi:10.1200/jco.2011.29.4_suppl.348
- Chang KJ, Wiersema MJ. Endoscopic ultrasound-guided fine-needle aspiration biopsy and interventional endoscopic ultrasonography. Emerging technologies. Gastrointest Endosc Clin N Am. 1997;7(2):221-235. Accessed September 23, 2025. http://www.ncbi.nlm.nih.gov/pubmed/9101263
- Inamdar S, Slattery E, Bhalla R, Sejpal D V., Trindade AJ. Comparison of Adverse Events for Endoscopic vs Percutaneous Biliary Drainage in the Treatment of Malignant Biliary Tract Obstruction in an Inpatient National Cohort. JAMA Oncol. 2016;2(1):112-117. doi:10.1001/JAMAONCOL.2015.3670
- Fakas S, Elias M, Lim D, Meytes V. Comparison of gastrojejunostomy techniques and anastomotic complications: a systematic literature review. Surg Endosc. 2021;35(12):6489-6496. doi:10.1007/S00464-020-08142-X
- Loehrer AP, Chang DC, Hutter MM, et al. Health Insurance Expansion and Treatment of Pancreatic Cancer: Does Increased Access Lead to Improved Care? J Am Coll Surg. 2015;221(6):1015-1022. doi:10.1016/j.jamcollsurg.2015.09.010
- Erlangga D, Suhrcke M, Ali S, Bloor K. The impact of public health insurance on health care utilisation, financial protection and health status in low- and middle-income countries: A systematic review. Buttigieg SC, ed. PLoS One. 2019;14(8):e0219731. doi:10.1371/journal.pone.0219731
- Kirkegård J, Mortensen FV, Cronin-Fenton D. Chronic Pancreatitis and Pancreatic Cancer Risk: A Systematic Review and Meta-analysis. American Journal of Gastroenterology.Nature Publishing Group. 2017;112(9):1366-1372. doi:10.1038/ajg.2017.218
- Lowenfels AB, Maisonneuve P, Cavallini G, et al. Pancreatitis and the risk of pancreatic cancer. International Pancreatitis Study Group. N Engl J Med. 1993;328(20):1433-1437. doi:10.1056/NEJM199305203282001
- Duell EJ, Lucenteforte E, Olson SH, et al. Pancreatitis and pancreatic cancer risk: a pooled analysis in the International Pancreatic Cancer Case-Control Consortium (PanC4). Annals of Oncology. 2012;23(11):2964. doi:10.1093/ANNONC/MDS140
- Rahib L, Smith BD, Aizenberg R, Rosenzweig AB, Fleshman JM, Matrisian LM. Projecting cancer incidence and deaths to 2030: the unexpected burden of thyroid, liver, and pancreas cancers in the United States. Cancer Res. 2014;74(11):2913-2921. doi:10.1158/0008-5472.CAN-14-0155
- Park W, Chaw Reilly EM. Pancreatic Cancer: A Review. JAMA. 2021;326(9):851-862. doi:10.1001/JAMA.2021.13027
- Ghosn M, Ibrahim T, Assi T, El Rassy E, Kourie HR, Kattan J. Dilemma of first line regimens in metastatic pancreatic adenocarcinoma. World J Gastroenterol. 2016;22(46):10124. doi:10.3748/WJG.V22.I46.10124
- Hajatdoost L, Sedaghat K, Walker EJ, Thomas J, Kosari S. Chemotherapy in pancreatic cancer: A systematic review. Medicina (Lithuania).MDPI AG. 2018;54(3). doi:10.3390/medicina54030048
- Funamizu N, Sakamoto A, Utsunomiya T, et al. Geriatric nutritional risk index as a potential prognostic marker for patients with resectable pancreatic cancer: a single-center, retrospective cohort study. Sci Rep. 2022;12(1):13644. doi:10.1038/s41598-022-18077-z
- Furuse J, Osugi F, Machii K, Niibe K, Endo T. Effect of cancer cachexia on first-line chemotherapy in patients with advanced pancreatic cancer: a claims database study in Japan. Int J Clin Oncol. 2024;29(4):456-463. doi:10.1007/S10147-024-02467-6
- Neoptolemos JP, Stocken DD, Bassi C, et al. Adjuvant chemotherapy with fluorouracil plus folinic acid vs gemcitabine following pancreatic cancer resection: a randomized controlled trial. JAMA. 2010;304(10):1073-1081. doi:10.1001/JAMA.2010.1275

