Community Health Workers’ COVID-19 Knowledge in Haiti, Malawi, and Rwanda
Community health workers’ knowledge, attitudes, and perceptions of risk for COVID-19: A cross-sectional survey in Haiti, Malawi and Rwanda
Kobel Duflo1, Stephanie Armbruster2, Erick Baganzizi3, Stefanie A. Joseph4, Nadege Belizaire5, Maurice Junior Chévalier5, Peterson Abhis Fauré5, Jimmy Jean Baptiste,5 Emmanuel Donsémbé5, Frank Gondwe6, Benson Chawinga6, Tamunine Musfah7, Jean Claude Muganga4, Dale A. Barnhart2,4, Betty Hedt-Gauthier8, Fabien Munyaneza6, Mary clisbee5,
- Partners in Health and Zanmi Lasante (ZL), Mirebalais, Haiti
- Department of Biostatistics, Harvard T.H. Chan School of Public Health, Boston, MA, USA
- Partners In Health, Inshuti Mu Buzima (IMB), Kigali, Rwanda
- Partners In Health, Boston, MA, USA
- Partners in Health and Zanmi Lasante (ZL), Mirebalais, Haiti
- Partners In Health, Abwenzi Pa za Umoyo (APZU), Neno, Malawi
- Partners In Health, Inshuti Mu Buzima (IMB), Kigali, Rwanda
- Department of Biostatistics, Harvard T.H. Chan School of Public Health, Boston, MA, USA; Department of Global Health and Social Medicine, Harvard Medical School, Boston, MA, USA
OPEN ACCESS
PUBLISHED: 31 December 2024
CITATION: DUBIQUE, Kobel et al. Community health workers’ knowledge, attitudes, and perceptions of risk for COVID-19: A cross-sectional survey in Haiti, Malawi and Rwanda. Medical Research Archives, [S.l.], v. 12, n. 12, dec. 2024. Available at: <https://esmed.org/MRA/mra/article/view/6012>.
COPYRIGHT: © 2025 European Society of Medicine. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ISSN 2375-1924
DOI: https://doi.org/10.18103/mra.v12i12.6012
ABSTRACT
Community health workers (CHWs) are critical to the response to COVID-19 in low- and middle-income countries (LMICs). This study aimed to assess the knowledge, perceptions, and attitudes of CHWs regarding COVID-19 and its vaccine in Haiti, Malawi, and Rwanda. A cross-sectional survey was conducted from June 2023 to October 2023, involving 525 eligible CHWs. We quantified the COVID-19 related knowledge among CHWs based on the success rate, indicating the proportion of correct affirmations or rejections of 10 statements surrounding COVID-19 and the COVID-19 vaccine. The success rates were captured across countries in a bar plot. We aimed to prioritize country-wise research collaboration. The results revealed that CHWs in Malawi had the highest knowledge, while those in Haiti had the lowest. Most CHWs acknowledged the threat posed by COVID-19, and the majority expressed willingness to receive the vaccine. However, barriers such as misinformation and lack of access to vaccines were reported. Our findings underscore the need for targeted interventions to enhance CHWs’ knowledge and address barriers to vaccination.
Keywords: Community health workers, COVID-19, knowledge, attitudes, perceptions, vaccine
1. Introduction
COVID-19 was one of the deadliest pandemics of the 21st century, with an estimated death toll ranging from 5 to 17 million people¹. The COVID-19 mortality rate has varied across time, areas, and among countries due to socioeconomic and political disparities², with low- and middle-income countries (LMICs) having a higher mortality rate and shorter length of time from infection to death compared to high-income countries during the second and third waves³. Further, rural communities experienced a higher COVID-19 mortality rate compared to urban communities because of longstanding healthcare disparities that contributed to delays in accessing healthcare⁴.
Vaccines for COVID-19 have proven to be one of the best health strategies to stop the spread of the virus and reduce mortality⁵. However, LMICs have not achieved the full benefits of COVID-19 vaccines. One issue is in-country access to vaccines, with more than 10 billion COVID-19 vaccines largely distributed in high-income countries⁶⁻⁷. Specific socioeconomic and political conditions in low-income countries further contribute to disparities in both vaccine administration and acceptance⁸. A second issue is an individual’s willingness to be vaccinated, which requires an awareness of COVID-19 risk and the benefits of the vaccines.
Community health workers (CHWs), who are often individuals elected by their communities to serve as a link between the homes and health facilities, are an important part of the health sectors in many LMICs⁹⁻¹¹. While CHWs cannot increase vaccine availability on a national level, these individuals are an important and trusted source of health-related information who could help educate community members on COVID-19 risks and the vaccine¹²⁻¹³.
Partners In Health (PIH) is a non-profit organization that works closely with governments in 11 countries, including Haiti, Malawi, and Rwanda, to provide quality healthcare and accompaniment with a preferential option for the poorest communities¹⁴. The organization champions care delivery in low-income countries using a community-based approach and the accompaniment model that engage community health workers in the provision of medicines, in social support, in education, and in the linkage of care between communities and health facilities¹⁵⁻¹⁶. When the COVID-19 pandemic devastated the world, PIH used its past experiences in combating infectious disease outbreaks and responding to disasters to launch a comprehensive effort to support COVID-19 response across country sites around the world¹⁷. The Global Coronavirus Response plan by Partners In Health addressed several key areas, including testing, provision of care, support for local government responses, mobilization of community health workers, and research development and capacity building¹⁷.
The study focused on Haiti, Malawi, and Rwanda for several key reasons. An invitation to participate in leveraging CHWs to combat misinformation was extended to all sites in PIH’s cross-site COVID-19 research network, which includes Haiti, Malawi and Rwanda. The three countries self-selected to participate due to their established CHW programs, interest in scientific research, and capacity to engage in the study. Their diverse geographic locations, spanning different continents, offered valuable insights into how local contexts, cultures, and experiences shape the response to the COVID-19 pandemic. Finally, at the inception of the study, country partners had identified both significant vaccine hesitancy and high levels of trust in CHWs, rendering Haiti, Malawi and Rwanda ideal candidate countries to explore the role of CHWs in addressing vaccine-related challenges¹⁸⁻²⁰.
In this paper, we describe the COVID-19 knowledge, attitude, and vaccination perceptions among CHWs in the rural areas of three different LMICs – Haiti, Malawi, and Rwanda. This study informs overall community awareness and activities related to COVID-19, using CHWs as a litmus for their communities, as well as potential areas to target for future CHW interventions. By exploring across
By exploring across three different countries, we gain a better understanding of the variability in COVID-19 knowledge, attitude, and vaccination perceptions that can support future CHW-driven initiatives and promote successful cross-site research collaboration.
2. Methods
STUDY SETTING:
This is a cross-sectional study of CHWs in the rural areas of Haiti, Malawi, and Rwanda that assessed the knowledge, perception, and attitude towards COVID-19 and its vaccine. CHWs were selected from the catchment areas of PIH, namely Zanmi Lasante in Haiti, Abwenzi Pa Za Umoyo in Malawi, and Inshuti Mu Buzima in Rwanda. In all three countries, these PIH organizations support health care delivery in underserved rural areas. Health systems in these areas rely on CHWs to connect communities to health facilities. In the Central Plateau and Lower Artibonite regions of Haiti, the CHW program, supported by PIH, operates in areas that either focus on specific diseases or provide general health care support. Overall, PIH supports approximately 2,500 Haitian CHWs in total, serving a population of roughly 3.3 million people²¹.
In Neno district, the PIH-supported area in Malawi, PIH implements a household model for CHW care, where a CHW provides support to all members of a household irrespective of their health status. The PIH community health department in Malawi has trained 629 CHWs to serve over 19,000 households, with the goal of ensuring faster access to health care, higher retention, and treatment adherence, as well as greater prevention and economic development²²˒²³.
In the Kirehe and Southern Kayonza districts of Rwanda, the CHWs supported by PIH are integrated into the national system, which was established in 2007²⁴. Each CHW has designated responsibilities, focusing either on the treatment of childhood diseases, malnutrition, providing care during pregnancy, and facilitating delivery at health care centers²⁵. In these two districts, PIH supports over 1,200 CHWs, serving approximately 48,000 households²⁶.
STUDY DESIGN AND DATA COLLECTION:
This study, conducted from June 2023 to October 2023, included 525 eligible CHWs (175 CHWs per country). Participants were eligible for the survey if they were over 18 years old and actively working in the country’s target catchment area (Haiti: 289 eligible CHWs, Malawi: 1232 eligible CHWs, Rwanda: 3499 eligible CHWs). In each country, 205 eligible CHWs (175 + 30 backup) were randomly sampled from the group of eligible CHWs, and the first 175 CHWs who agreed to participate were recruited.
The CHW survey was conducted in the local language – Haitian Creole in Haiti, Chichewa in Malawi, and Kinyarwanda in Rwanda. The survey was administered by trained enumerators, who directly entered the data into REDCap using tablets. The CHW survey lasted 30 to 90 minutes and comprised of questions about COVID-19 infection and vaccine history, reasons for or against receiving the COVID-19 vaccine, awareness of the COVID-19 virus and vaccine, and the perceived danger of a COVID-19 infection and overall attitude towards the pandemic. The survey also collected personal demographic information from each CHW.
DATA ANALYSIS:
The data were exported from REDCap, cleaned, and analyzed using STATA v15.1. Figures were generated in R v4.3.2. We summarized categorical variables by percentages and counts or medians and interquartile range (IQR), and continuous variables by means and standard deviations. Using the method of Wang et al.²⁵, we visualized the perceptions of CHWs about COVID-19 about risk, worry, severity, and control in a boxplot, stratified by country, with each country team being able to modify their priority disease comparison list. On each plot, we display the median responses for other reference diseases assessed in the survey, namely (1) infectious diseases: cholera, tuberculosis, HIV/AIDS, malaria, typhoid (Haiti only), Ebola (Rwanda only); (2) non-communicable diseases: diabetes, cardiovascular diseases, asthma, malnutrition, hypertension (Rwanda and Haiti only); (3) mental health diseases. anxiety, depression, suicidal ideation (Haiti only).
We tested for a global difference in answer distribution for COVID-19 responses with a Kruskal-Wallis test and pairwise differences between countries with a Mann-Whitney U-test.
We quantified the COVID-19 related knowledge among CHWs based on the success rate, indicating the proportion of correct affirmations or rejections of 10 statements surrounding COVID-19 and the COVID-19 vaccine. Such knowledge assessment was used in previous research²⁶˒²⁷. The statements referred to common COVID-19 related misconceptions and stigma. The success rates were compared across countries in a bar plot. We tested for pairwise country-wise differences in knowledge in a Chi-squared test.
We captured attitudes towards COVID-19 using a 3-level agreement Likert scale – (1) Strongly Disagree, (2) Neutral, (3) Strongly Agree – to 18 statements surrounding worry about health, beliefs in effectiveness of public health measures, development and controllability of the pandemic, as well as trust in governmental public health management²⁷. Pairwise country-wise differences were visualized in a Likert plot and tested for by an unpooled t-test based on the mean attitude towards COVID-19 across statements.
Depending on their vaccination status, the CHWs were prompted to indicate the reasons for or against receiving a COVID-19 vaccination. All CHWs were asked about their intention and reasons to receive vaccine boosters. The answers were attributed to a predefined category (multiple answers possible) or indicated in an “Other” category, following standard procedure¹⁹˒²⁸. The answer frequencies were analyzed in a bar plot.
ETHICS:
The study received ethical approval from the Harvard Internal Review Board (IRB# 11-1339), the Malawi National Committee on Research in the Social Sciences and Humanities (IRB# 11/22/694), the Haiti Zanmi Lasante Institutional Review Board (IRB# 11082022), and the Rwanda National Research Ethics Committee (IRB# 00001497). All CHWs provided informed consent prior to study participation. Participants received a baseline compensation of $5 to $10, as well as additional country- and time-specific compensation and reimbursement for travel.
3. Results
DEMOGRAPHIC CHARACTERISTICS:
This study included 525 CHWs, divided equally across countries (Table 1). Nearly two-thirds were female in Malawi (n=117, 66.9%) and Rwanda (n=115, 65.7%), but only one-third were female in Haiti (n=66, 37.7%). The mean age was 44.7 years (standard deviation (s.d.) ± 10.2 years). The majority of CHWs (n=457, 90.7%) had at least one child who was ≤18 years old. The median number of children ≤18 years old across countries was 2 (IQR: 1–3); for those children ≤18 years old, the mean age was 8.5 years (s.d. ± 6.8 years).
Table 1: Demographics among community health workers in Rwanda, Malawi and Haiti
| Rwanda | Malawi | Haiti | Total |
|---|---|---|---|
| n | % | n | % |
| Number of community health workers involved in survey | 175 | 33.33 | 175 |
| Sex | |||
| Female | 115 | 65.70 | 117 |
| Children | |||
| Have children | 174 | 99.40 | 170 |
| Rwanda | Malawi | Haiti | Total | |
|---|---|---|---|---|
| n | % | n | % | n |
| Yes, and at least one child ≤18 years | 160 | 92.50 | 153 | 91.10 |
| Yes, but all children are >18 years | 13 | 7.40 | 15 | 8.60 |
| Rwanda | Malawi | Haiti | Total | |
|---|---|---|---|---|
| mean / median | STD / IQR | mean / median | STD / IQR | mean / median |
| Age (years), mean (STD) | 42.9 | 9.9 | 42.5 | 10.5 |
| Children | ||||
| Number of children ≤18 years, median (IQR) | 2 | (1.0–3.0) | 2 | (2.0–3.0) |
| Age of child if <18 years old (in years), mean (STD) | 7.9 | 7.2 | 8.7 | 6.5 |
PERCEPTIONS OF HEALTH RISK–WORRY–SEVERITY–CONTROL OF COVID-19:
The perception of COVID-19 controllability among CHWs varied significantly across countries (p<0.001) (Figure 1A). The highest belief in COVID-19 controllability was registered in Rwanda (median=5 indicating “Strongly agree”, IQR: 3–5; Malawi: median=4 indicating “Agree”, IQR: 3–5; Haiti: median=4 indicating “Agree”, IQR: 3–5). The median controllability value for COVID-19 aligned with the median across all reference diseases (noted by the red stars in Figure 1A), indicating similar perceptions of controllability for COVID-19 and the reference diseases.
Perceived risk of a COVID-19 infection varied significantly by country (p<0.001) (Rwanda: median=1 indicating “Much lower than average”, IQR: 1–2; Malawi: median=3 indicating “Average”, IQR: 2–4; Haiti: median=2 indicating “Lower than average”, IQR: 1–5) (Figure 1B). In Rwanda, CHWs perceived the median risk of contracting a reference disease as “Lower than average” for COVID-19. In Malawi and Haiti, the median risk perception for the reference diseases aligned with the perception of COVID-19 risk.
The perception of the severity of a COVID-19 infection differed significantly between Rwanda and Malawi versus Haiti (p<0.01) (Rwanda / Malawi: median=5 indicating “Strongly Agree”, IQR: 4–5; Haiti: median=4 indicating “Agree”, IQR: 4–5) (Figure 1C). In Malawi, CHWs considered COVID-19 a more serious disease than the reference diseases (median=4 indicating “Agree”, IQR: 4–5) (Figure 1C). The perception of severity for COVID-19 and the reference diseases aligned for Rwanda and Haiti.
The CHWs worried little about contracting COVID-19 (for all countries: median=1 indicating “Not at all”, Rwanda: IQR: 1; Haiti / Malawi: IQR: 1–2) (Figure 1D). The perceptions of worry varied significantly across countries (p<0.05 for Haiti and Malawi, p<0.001 otherwise). Participants did not worry more or less about contracting COVID-19 than the reference diseases.
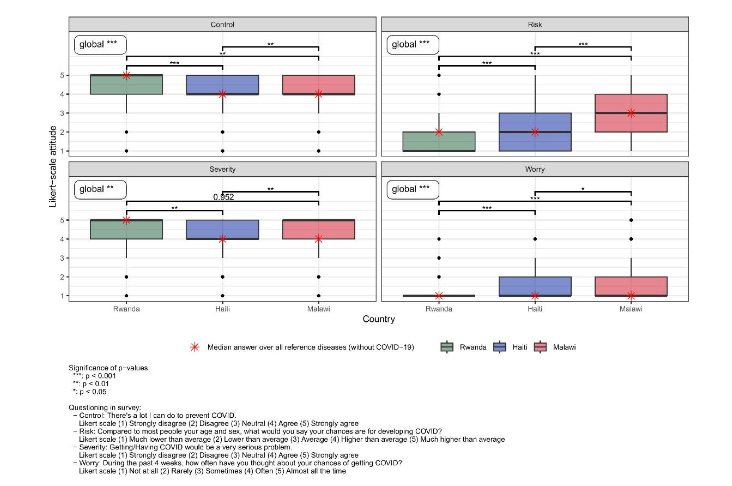
Figure 1: Danger perception towards COVID-19; questioning surrounding perception of risk, worry, severity and control among community health workers in Rwanda, Malawi and Haiti
KNOWLEDGE ABOUT COVID-19 AND COVID-19 VACCINE AMONG COMMUNITY HEALTH WORKERS:
In Rwanda and Haiti, CHWs were very knowledgeable, while they were less so in Malawi (COVID-19 knowledge: Malawi–Haiti / Malawi–Rwanda p<0.001; Rwanda–Haiti: p=0.429; COVID-19 vaccine knowledge: Rwanda–Malawi / Rwanda–Haiti / Malawi–Haiti: p<0.001).
In Rwanda and Haiti, CHWs showed more knowledge on the effectiveness of preventive measures (facemasks, avoiding crowded places, immediate isolation of contact person) than CHWs in Malawi (facemasks: Haiti: n=151, 86.3%; Malawi: n=1, 0.6%; Rwanda: n=168, 96.0%) (avoid crowded places: Haiti: n=163, 93.1%; Malawi: n=5, 2.9%; Rwanda: n=157, 89.7%) (immediate isolation of contact person: Haiti: n=156, 89.1%; Malawi: n=9, 5.1%; Rwanda: n=164, 93.7%) (Figure 2A).
Popular COVID-19 myths seemed widely disseminated in Malawi; 42 (24.0%) CHWs believed that a virus transmission cannot happen without a fever; only 64 (36.4%) CHWs correctly rejected the statement that contracting the COVID-19 disease was safer than receiving the vaccine; 3 (1.7%) CHWs correctly rejected the belief that the COVID-19 vaccine can cause infertility; and only 10 (5.7%) correctly rejected that a vaccination can lead to an infection with COVID-19 (Figure 2A, 2B).
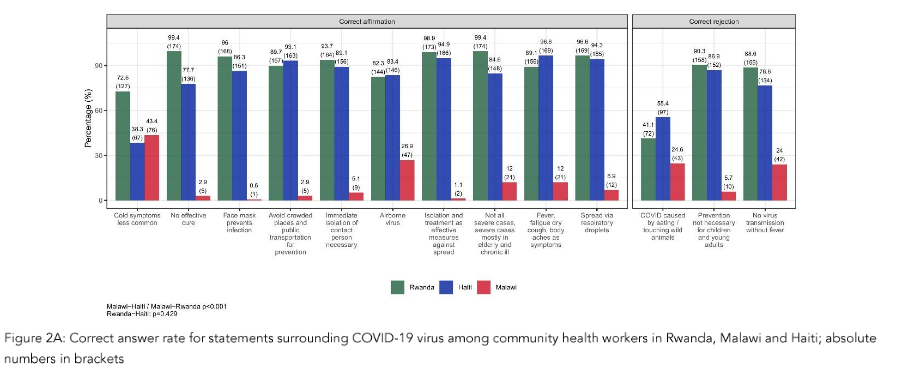
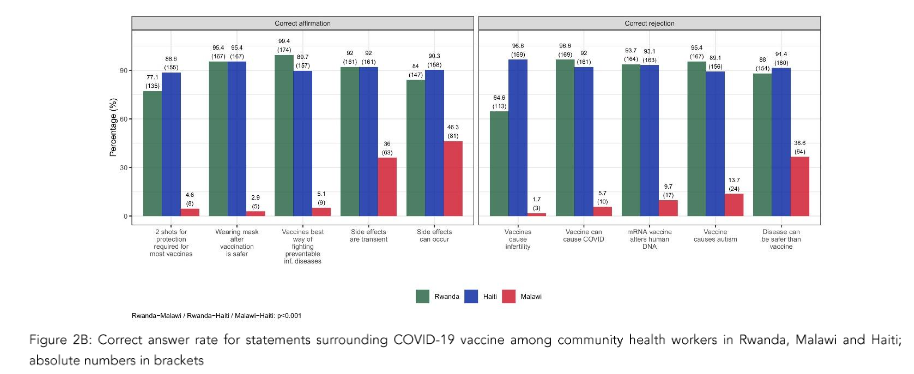
Figure 2B: Correct answer rate for statements surrounding COVID-19 vaccine among community health workers in Rwanda, Malawi and Haiti; absolute numbers in brackets
ATTITUDES ABOUT COVID-19 AMONG COMMUNITY HEALTH WORKERS IN HAITI, MALAWI, AND RWANDA:
The mean attitude across countries differed significantly across countries (Rwanda–Malawi: p<0.001; Rwanda–Haiti: p<0.001; Malawi–Haiti: p=0.0013). Most CHWs acknowledged the threat COVID-19 posed to the public (Haiti: n=168, 96.0%; Malawi: n=159, 90.9%; Rwanda: n=173, 98.9%) and agreed on the efficacy of social distancing to control COVID-19 (Haiti: n=162, 93.6%; Malawi: n=170, 97.7%; Rwanda: n=160, 94.7%) (Figure 3).
Participants were confident in the abilities of their country to overcome the COVID-19 virus (Haiti: n=149, 85.1%; Malawi: n=133, 76.4%; Rwanda: n=171, 97.7%).
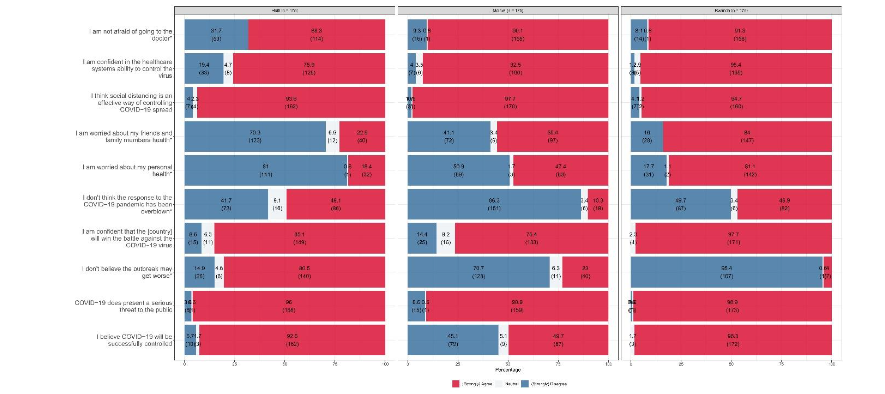
Figure 3: Attitude of community health workers towards the COVID-19 pandemic and its management in Rwanda, Malawi and Haiti; absolute numbers in brackets
In Haiti and Malawi, CHWs expressed little concern for their health as well as for the health of their families and friends (personal health: Haiti: n=141, 81.0%; Malawi: n=89, 50.9%; Rwanda: n=31, 17.7%); (friends and family members’ health: Haiti: n=123, 70.3%; Malawi: n=72, 41.1%; Rwanda: n=28, 16.0%). Haitian CHWs expressed fear and doubt about their physicians and healthcare system (unafraid of visiting doctor: n=53, 31.7%; no belief in the healthcare system’s ability to control the virus: n=33, 19.4%), yet did not believe the outbreak to worsen (n=140, 80.5%). Rwandan and Malawian CHWs were more pessimistic in terms of the future development of the pandemic. (“Strongly agree”/“Agree” outbreak will not get worse: Malawi: n=40, 23.0%; Rwanda: n=7, 4.9%).
HISTORY OF COVID-19 VACCINATIONS AMONG COMMUNITY HEALTH WORKERS:
Most CHWs could not recall a previous infection with COVID-19 (Haiti: n=167, 95.4%; Malawi: n=166, 94.9%; Rwanda: n=172, 98.3%) (Table 2). Many CHWs in Haiti and Rwanda confirmed having received the COVID-19 vaccine (Haiti: n=170, 97.1%; Rwanda: n=175, 100%); however, 58 (33.1%) Malawian CHWs did not receive a COVID-19 vaccine. Rwanda had the highest vaccination rate with two doses of the COVID-19 vaccine (n=134, 76.6%) and the highest COVID-19 booster rate (n=133, 99.3%). Booster was unavailable in Haiti. Most CHWs across countries would agree to be vaccinated if an approved third and fourth dose of vaccine to prevent COVID-19 was available today at no cost (Haiti: n=163, 93.7%; Malawi: n=155, 88.6%; Rwanda: n=174, 99.4%).
Table 2: Vaccine history and vaccination intention among community health workers in Rwanda, Malawi and Haiti
| Rwanda | Malawi | Haiti | Total | |
|---|---|---|---|---|
| Previous COVID-19 infection | ||||
| To your knowledge, do you have or have you had COVID-19? | ||||
| N = | 175 | 175 | 175 | 525 |
| No | 172 (98.3%) | 166 (94.9%) | 167 (95.4%) | 505 (96.2%) |
| Yes | 3 (1.7%) | 5 (2.9%) | 8 (4.6%) | 16 (3.1%) |
| Not sure/It depends | 0 | 4 (2.3%) | 0 | 4 (0.8%) |
| COVID-19 vaccination history | ||||
| Have you received a COVID-19 vaccine? | ||||
| No | 0 | 58 (33.1%) | 5 (2.9%) | 63 (12%) |
| Yes | 175 (100%) | 117 (66.9%) | 170 (97.1%) | 462 (88%) |
| How many doses of COVID-19 vaccine have you received? | ||||
| N = | 175 | 117 | 170 | 462 |
| One dose | 25 (14.3%) | 40 (34.2%) | 91 (53.5%) | 156 (33.8%) |
| Two doses | 134 (76.6%) | 77 (65.8%) | 79 (46.5%) | 290 (62.8%) |
| Don’t know | 16 (9.1%) | 0 | 0 | 16 (3.5%) |
| Have you received a booster dose? | ||||
| N = | 134 | 77 | 79 | 290 |
| No | 1 (0.7%) | 41 (53.2%) | 79 (100%) | 121 (41.7%) |
| Yes | 133 (99.3%) | 36 (46.8%) | 0 | 169 (58.3%) |
| Intention to vaccinate | ||||
| If an approved third and fourth dose of vaccine to prevent COVID-19 was available to you today at no cost, would you agree to be vaccinated? | ||||
| N = | 175 | 175 | 174 | 524 |
| No | 0 | 15 (8.6%) | 8 (4.6%) | 23 (4.4%) |
| Yes | 174 (99.4%) | 155 (88.6%) | 163 (93.7%) | 492 (93.9%) |
| Not sure/It depends | 1 (0.6%) | 5 (2.9%) | 3 (1.7%) | 9 (1.7%) |
REASONS AGAINST PAST VACCINATION AND FOR OR AGAINST THE INTENTION TO VACCINATE:
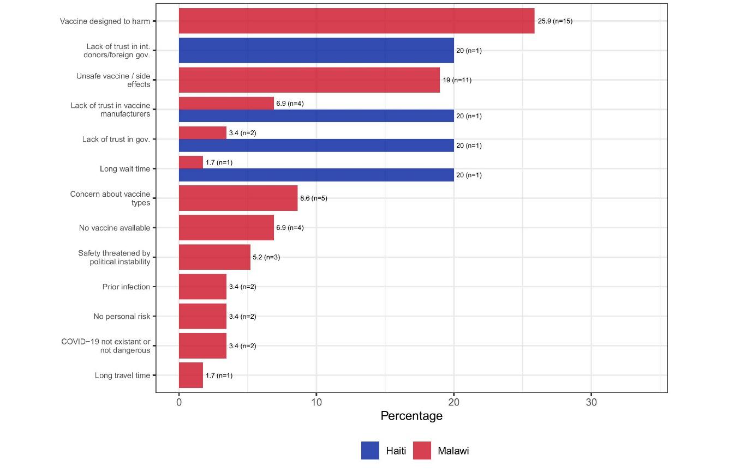
In Haiti, CHWs lacked trust, resulting in refusing vaccination in the past (lack of trust in international donors/foreign governments: n=1, 20%; in local government: n=1, 20%; in vaccine manufacturers: n=1, 20%). In Malawi, CHWs expressed safety concerns as the main reason for refusing vaccination in the past (harmfulness of vaccine: n=15, 25.9%; unsafe vaccine/side effects: n=11, 19.0%; lack of trust in vaccine manufacturers: n=4, 6.9%; concern about vaccine types: n=5, 8.6%) (Figure 4A). All CHWs in Rwanda were vaccinated.
Figure 4A: Reasons against vaccination among community health workers in Haiti (n=5) and Malawi (n=58); no community health workers in Rwanda reported being unvaccinated; absolute numbers in brackets
Reasons for expressing no intention to get vaccinated in Haiti included vaccine availability (n=2, 18.2%), unsafe vaccine (n=1, 9.1%), and the belief that COVID-19 did not exist or did not constitute a danger for community members (n=1, 9.1%) (Figure 4B). In Malawi, safety concerns were the primary reason to refuse additional vaccination (unsafe vaccine: n=5, 25.0%; concerns about vaccine types: n=2, 10.0%; vaccine designed to harm: n=2, 10.0%). In Rwanda, one CHW considered themselves not at risk for COVID-19
Figure 4B: Reasons against intention to vaccinate among community health workers in Rwanda (n=1), Haiti (n=11) and Malawi (n=20); absolute numbers in brackets
Community health workers’ perceptions of COVID-19 in Haiti, Malawi, and Rwanda
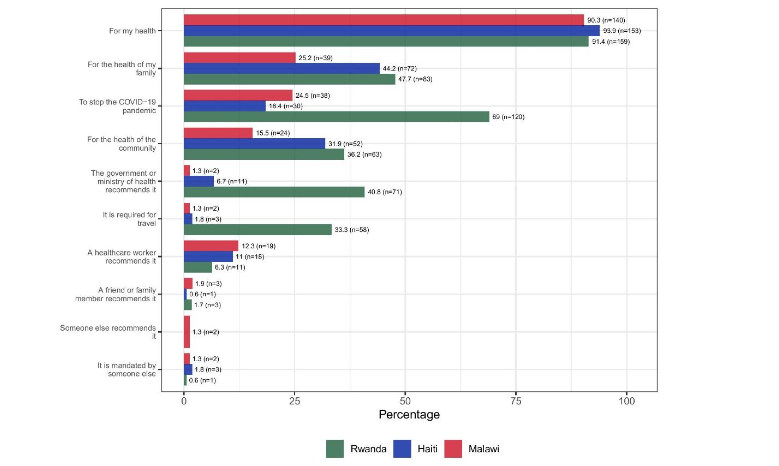
Personal health, the health of family, and their communities were the main reason for expressing intentions to vaccinate across countries (personal health: Haiti: n=153, 93.9%; Malawi: n=140, 90.3%; Rwanda: n=159, 91.4%; family health: Haiti: n=72, 44.2%; Malawi: n=39, 25.2%; Rwanda: n=83, 47.7%; community health: Haiti: n=52, 31.9%; Malawi: n=24, 15.5%; Rwanda: n=63, 36.2%).
Another reason included CHWs’ desire to stop the COVID-19 pandemic (Haiti: n=30, 18.4%; Malawi: n=38, 24.5%; Rwanda: n=120, 69.0%). In Rwanda, recommendations by the government and the Ministry of Health as well as travel requirements incentivized vaccination (recommendation: Rwanda: n=71, 40.8%; Haiti: n=11, 6.8%; Malawi: n=2, 1.3%; travel: Rwanda: n=58, 33.3%; Haiti: n=3, 1.8%; Malawi: n=2, 1.3%).
Recommendations by a health care worker strongly motivated Haitian and Malawian CHWs (Haiti: n=18, 11.0%; Malawi: n=19, 12.3%; Rwanda: n=11, 6.3%).
Figure 4C: Reasons for intention to vaccinate among community health workers in Rwanda (n=174), Malawi (n=155) and Haiti (n=163); absolute numbers in brackets
Discussion
The study investigated differences in CHW’s risk perception, knowledge, and attitude towards COVID-19 and COVID-19 vaccination efforts across three LMICs: Rwanda, Malawi, and Haiti. Overall, CHWs considered COVID-19 a serious public health threat and expressed their support for adherence to public health interventions; yet, they did not perceive the virus as an immediate threat to their personal health. They voiced doubt about the intensity and effectiveness of national pandemic responses. Knowledge around COVID-19 as well as vaccination rates depended on national settings.
Rwandan CHWs exhibited a strong sense of control over COVID-19, with little worry about contracting the disease. Early in the pandemic, the Rwandan government (including the Rwandan Ministry of Health, the Biomedical Center, and the Surveillance Response Division) implemented a comprehensive Coronavirus National Preparedness and Response Plan, whose key aims were to contain the spread of the virus and combat misinformation²⁹. It implemented innovative strategies using drones, robots, and social media for the rapid dissemination of public health information, COVID-19 response supplies, and transparent risk communication, fostering trust in its communities³⁰. Most Rwandans received at least two doses of the COVID-19 vaccine, contributing to the high confidence in their country’s healthcare system³¹.
In Haiti and Malawi, weaker health infrastructure and misinformation may have negatively affected the risk perceptions of COVID-19¹⁹˒³²–³⁴. Participants in Malawi considered COVID-19 a more uncontrollable, severe disease and expressed a pessimistic outlook on future pandemic developments. Yet, many CHWs in Malawi considered the response to the pandemic overblown and perceived the risk of a personal COVID-19 infection as low. Their perceptions might have been negatively affected by the limited training opportunities for CHWs in remote regions, the focus on theoretical training without practice modules, and by the non-availability of equipment for knowledge application³⁵.
Overall, the lack of knowledge about COVID-19 in Malawi also likely contributed to the perception of the virus as being of little concern, compared to CHWs in Haiti and Rwanda who demonstrated accurate knowledge about COVID-19 and the vaccine. To date, there have been no studies comparing the vaccine among CHWs in Haiti, Malawi, and Rwanda. Previous research has shown that knowledge of COVID-19 and its vaccine differs across countries³⁶˒³⁷. Our findings align with those of a community-based survey on Knowledge, Attitudes, and Practices (KAP) related to COVID-19 among adults in Malawi, which revealed limited knowledge of the virus³⁸. A qualitative study involving Bangladesh, India, Kenya, Malawi, and Nigeria indicated inadequate training opportunities and lack of necessary equipment were the main causes of the CHWs’ lack of knowledge³⁵. In Malawi, particularly in the Neno district, low knowledge levels about COVID-19 and vaccines might be attributed to remote location and context, gaps in the levels of education, opportunities for ongoing dialogue during the design and implementation of the community sensitization activities, and limited access to information³⁹˒⁴⁰. Conversely, CHWs from Haiti demonstrated a strong awareness of the infectious nature of the virus and expressed concerns about contracting COVID-19.
The differences in knowledge might have contributed to differences in CHWs’ attitude towards COVID-19. Our results revealed that a majority of CHWs in Haiti displayed apprehension towards seeking medical assistance. Amid the COVID-19 pandemic, numerous Haitians refrained from seeking healthcare services⁴¹. Additionally, adverse political conditions and large-scale lockdowns significantly hampered the overall accessibility of the healthcare system. Haitian CHWs harbored some skepticism regarding the healthcare system’s capability to manage the virus. This lack of trust in the healthcare system and COVID-19-related information was compounded by the fact that Haiti faced tremendous challenges in stopping the pandemic due to inadequate biosecurity, testing infrastructure, and resources, along with the spread of misinformation and stigma surrounding COVID-19⁴¹. In addition, adverse political conditions, violence, and large-scale lockdowns significantly impacted the overall healthcare response in Haiti. The COVID-19 pandemic concurred with extreme political instability and gang violence in Haiti, calling for any results to be set into perspective.
Rwandan CHWs’ optimism towards the pandemic development and an effective governmental response to contain the pandemic aligns with previous studies which revealed a strong belief in virus control and national public health capabilities among citizens⁴³–⁴⁶. The Rwandan government implemented its comprehensive Coronavirus National Preparedness and Response Plan early in the pandemic. It employed innovative strategies for quick dissemination of public health information and transparent risk communication, fostering trust in its communities³⁰.
In our study, Malawian CHWs questioned the controllability of the virus, yet they did not expect the pandemic to worsen. Many CHWs considered the response to the pandemic overblown, most prominently in Malawi. When COVID-19 arrived in Malawi, public health policies restricted social gatherings⁴⁷. Nevertheless, political rallies were
held, openly violating the public health guidance⁴⁷. This caused severe mistrust in the government and undermined the relevance of the COVID-19 prevention measures⁴⁷. The Malawian High Court overruled the country’s lockdown after nationwide protests against lockdown policies⁴⁷. The opposition to movement restrictions in Malawi might have resulted from its direct consequences on livelihoods⁴⁸. As our results showed, a substantial proportion of CHWs in Haiti, Malawi, and Rwanda supported adherence to social distancing measures as an effective intervention to mitigate the spread of COVID-19. At the time of the initial COVID-19 outbreak, stringent restrictions were observed to forestall the virus propagation. These findings align with those originating from a comprehensive review of studies conducted across multiple countries, revealing communities’ favorable dispositions towards adopting public health directives aimed at containing the COVID-19 virus³⁶. Furthermore, an epidemiological study from Rwanda⁴⁹ unveiled that a notable majority of respondents voiced concerns regarding crowded locales and readily complied with mandates pertaining to facial covering⁴⁴˒⁴⁸. Adherence to these guidelines exhibited a strong correlation with the practical abstinence from high-risk behaviors conducive to COVID-19 transmission.
Vaccination coverage among CHWs, and the number of vaccine and booster doses, varied according to the availability of COVID-19 vaccines in Rwanda, Malawi, and Haiti. The COVID-19 vaccination rate among CHWs in Rwanda are highest compared to Haiti and Malawi. Most Rwandans received at least two doses of COVID-19 vaccine³¹. The vaccination success was attributed to the high confidence of Rwandans in their country’s healthcare system³¹. From the beginning of the global vaccination efforts onwards, Rwanda received an ample supply of COVID-19 vaccines. As the pandemic progressed, the government strove to achieve herd immunity by administering several COVID-19 booster doses³¹.
As our data showed, Rwanda had the highest proportion of CHWs who were boosted with additional doses of the COVID-19 vaccine. In Haiti, vaccine supply depended on US donations⁵⁰, and many vaccination campaigns failed due to a lack of vaccine supply. Haiti only administered a first and second dose of the vaccine to officials, health care professionals, and people living with comorbidities. No data was available on the percentage of Haitians vaccinated with at least one booster dose of a COVID-19 vaccine⁵¹. In March 2021, the Malawian government received a shipment of 360,000 doses of AstraZeneca to administer the first dose to healthcare workers, officials, the elderly, and people with comorbidities⁵². Vaccine hesitancy limited the success of the national COVID-19 vaccine campaign⁵²˒⁵³. Key drivers of vaccine hesitancy in Malawi were mistrust in the safety of the COVID-19 vaccine, complacency due to a lack of knowledge, and misinformation, which continuously affected vaccination efforts⁵⁴.
Previous literature additionally emphasized education levels, socio-economic status, exposure to vaccine-related misinformation and trust in public health authorities as pivotal factors influencing vaccine hesitancy⁵⁵–⁵⁹. When COVID-19 spread, PIH started a global COVID-19 response, and PIH’s Strategy for Achieving Equity in COVID-19 Vaccination at all the country sites increased the willingness for vaccination⁶⁰. Healthcare workers, including CHWs, were identified as the most trusted source of vaccine information⁶¹. Our results, which show that most CHWs in Rwanda, Haiti, and Malawi would be willing to receive additional COVID-19 vaccine doses, provide reasons for optimism.
Several limitations should be considered when interpreting these results. First, the survey relied on self-reported information without requesting any documentation or proof of vaccination to verify given answers. Given that national economic context, public policy, cultural factors and societal dynamics strongly influenced knowledge, attitude, risk perceptions and vaccination willingness, our
findings are limited in their comparability and generalizability to other LMICs. In addition, PIH pursued a global COVID-19 response and developed a strategy for achieving equity in COVID-19 vaccination across all country sites. Such coordinated action contributed to an overall willingness for vaccination among PIH staff, including CHWs⁶⁰. This further might restrict generalizability. Lastly, the results of this study were focused on adult CHWs only. Nevertheless, insights from our analyses provide guidance and impetus to leverage CHWs as trusted sources of information and as enforcers of public health interventions.
Conclusion
Risk perception, knowledge of COVID-19 and the COVID-19 vaccine, as well as the attitude towards the pandemic among CHWs, differed across Rwanda, Malawi, and Haiti. Overall, CHWs consider COVID-19 a serious disease, yet they do perceive it as a non-immediate health threat. National narratives, public health communication, and training opportunities influence the knowledge of COVID-19 and its vaccine among CHWs. Vaccine availability determined the vaccine history of CHWs. Lack of trust was a frequent reason for vaccine hesitancy. Targeted interventions and transparent, trustworthy communication are essential to ensure that CHWs are well informed, have a cautious attitude toward COVID-19, and possess the skills needed to promote public health compliance within communities.
Conflict of Interest:
The authors have no conflicts of interest to declare.
Funding Statement:
This research was made possible by the Social Science Research Council’s Mercury Project with funding from The Rockefeller Foundation, Robert Wood Johnson Foundation, Craig Newmark Philanthropies, and the Alfred P. Sloan Foundation.
Acknowledgements:
Special thanks to Ximena Tovar, Kathryn Hanly, and Caitlin Roman for their leadership and support during the project implementation. We acknowledge the contribution of our study participants, staff, and executive leadership from the three participating countries.
Target journal:
Challenges and Opportunities in COVID-19, Special issue from the European Society of Medicine
References
1. Prabhu M, Gergen J. History’s Seven Deadliest Plagues. VaccinesWork. November 15, 2021. Accessed August 15, 2024. https://www.gavi.org/vaccineswork/historys-seven-deadliest-plagues
2. Sorci G, Faivre B, Morand S. Explaining among-country variation in COVID-19 case fatality rate. Sci Rep. 2020;10(1):18909. doi:10.1038/s41598-020-75848-2
3. Yao L, Aleya L, Howard SC, et al. Variations of COVID-19 mortality are affected by economic disparities across countries. Sci Total Environ. 2022;832:154770. doi:10.1016/j.scitotenv.2022.154770
4. Grome HN, Raman R, Katz BD, et al. Disparities in COVID-19 Mortality Rates: Implications for Rural Health Policy and Preparedness. J Public Health Manag Pract. 2022;28(5):478-485. doi:10.1097/PH H.0000000000001507
5. Moghadas SM, Vilches TN, Zhang K, et al. The Impact of Vaccination on Coronavirus Disease 2019 (COVID-19) Outbreaks in the United States. Clin Infect Dis. 2021;73(12):2257-2264. doi:10.10 93/cid/ciab079
6. Our World in Data. Total COVID-19 vaccine doses administered. Our World in Data. Accessed August 15, 2024. https://ourworldindata.org/grapher/cumulative-covid-vaccinations?tab=map
7. Ahlberg BM, Bradby H. Ethnic, racial and regional inequalities in access to COVID-19 vaccine, testing and hospitalization: Implications for eradication of the pandemic. Front Sociol. 2022;7:809090. doi:10.3389/fsoc.2022.809090
8. Bayati M, Noroozi R, Ghanbari-Jahromi M, Jalali FS. Inequality in the distribution of Covid-19 vaccine: a systematic review. Int J Equity Health. 2022;21(1):122. doi:10.1186/s12939-022-01729-x
9. World Health Organization. WHO Guideline on Health Policy and System Support to Optimize Community Health Worker Programmes.; 2018.
10. Ahmed S, Chase LE, Wagnild J, et al. Community health workers and health equity in low- and middle-income countries: systematic review and recommendations for policy and practice. Int J Equity Health. 2022;21(1):49. doi:10.1186/s12939-021-01615-y
11. Mukherjee J, Farmer P. An Introduction to Global Health Delivery: Practice, Equity, Human Rights. 2nd ed. Oxford University PressNew York; 2021. doi:10.1093/oso/9780197607251.001.0001
12. Ballard M, Johnson A, Mwanza I, et al. Community Health Workers in Pandemics: Evidence and Investment Implications. Glob Health Sci Pract. 2022;10(2):e2100648. doi:10.97 45/GHSP-D-21-00648
13. Oliver J, Ferdinand A, Kaufman J, Allard N, Danchin M, Gibney KB. Community health workers’ dissemination of COVID-19 information and services in the early pandemic response: a systematic review. BMC Health Serv Res. 2024;24 (1):711. doi:10.1186/s12913-024-11165-y
14. Countries. Partners In Health. Accessed November 14, 2024. https://www.pih.org/countries
15. Mukherjee JS, Barry D, Weatherford RD, Desai IK, Farmer PE. Community-Based ART Programs: Sustaining Adherence and Follow-up. Curr HIV/AIDS Rep. 2016;13(6):359-366. doi:10.1007/ s11904-016-0335-7
16. 5 Unique Elements Driving Partners In Health’s Work. Partners In Health. June 8, 2021. Accessed November 14, 2024. https://www.pih.org/article/5-unique-elements-driving-partners-healths-work
17. Global Coronavirus Response. Partners In Health. March 13, 2020. Accessed November 14, 2024. https://www.pih.org/article/global-coronavirus-response
18. Chery MJ, Dubique K, Higgins JM, et al. COVID-19 vaccine acceptance in three rural communes in Haiti: A cross-sectional study. Hum Vaccines Immunother. 2023;19(1):2204048. doi:10. 1080/21645515.2023.2204048
19. Aron MB, Connolly E, Vrkljan K, et al. Attitudes toward COVID-19 Vaccines among Patients with Complex Non-Communicable Disease and Their Caregivers in Rural Malawi. Vaccines. 2022;10(5) :792. doi:10.3390/vaccines10050792
20. Niyigena A, Girukubonye I, Barnhart DA, et al. Rwanda’s community health workers at the front line: a mixed-method study on perceived needs and challenges for community-based healthcare delivery during COVID-19 pandemic. BMJ Open. 2022;12(4):e055119. doi:10.1136/bmjopen-2021-055119
21. Partners In Health. Haiti. Partners In Health. Accessed May 1, 2024. https://www.pih.org/country/haiti
22. Partners In Health. Malawi. Partners In Health. Accessed May 5, 2024. https://www.pih.org/country/malawi
23. Admon AJ, Bazile J, Makungwa H, et al. Assessing and improving data quality from community health workers: a successful intervention in Neno, Malawi. Public Health Action. 2013;3(1):56-59. doi:10.5588/pha.12.0071
24. Condo J, Mugeni C, Naughton B, et al. Rwanda’s evolving community health worker system: a qualitative assessment of client and provider perspectives. Hum Resour Health. 2014; 12(1):71. doi:10.1186/1478-4491-12-71
25. Wang C, O’Neill SM, Rothrock N, et al. Comparison of risk perceptions and beliefs across common chronic diseases. Prev Med. 2009;48 (2):197-202. doi:10.1016/j.ypmed.2008.11.008
26. Lee SK, Sun J, Jang S, Connelly S. Misinformation of COVID-19 vaccines and vaccine hesitancy. Sci Rep. 2022;12(1):13681. doi:10.1038/ s41598-022-17430-6
27. Bakdash T, Marsh C. Knowledge, Attitudes, and Beliefs Regarding the COVID-19 Pandemic Among Women in Kansas. J Community Health. 2021;46(6):1148-1154. doi:10.1007/s10900-021-00994-1
28. Joseph SA, Jerome JG, Boima F, et al. Attitudes toward COVID-19 Vaccination: Staff and Patient Perspectives at Six Health Facilities in Sierra Leone. Vaccines. 2023;11(8):1385. doi:10.3390/ vaccines11081385
29. Musanabaganwa C, Cubaka V, Mpabuka E, et al. One hundred thirty-three observed COVID-19 deaths in 10 months: unpacking lower than predicted mortality in Rwanda. BMJ Glob Health. 2021;6(2):e004547. doi:10.1136/bmjgh-2020-004547
30. Karim N, Jing L, Lee JA, et al. Lessons Learned from Rwanda: Innovative Strategies for Prevention and Containment of COVID-19. Ann Glob Health. 2021;87(1):23. doi:10.5334/aogh.3172
31. Uwizeyimana T, Manirambona E, Saidu Musa S, Uwiringiyimana E, Bazimya D, Mathewos K. Achieving COVID‐19 herd immunity in Rwanda, Africa. Public Health Chall. 2023;2(1):e75. doi:10. 1002/puh2.75
32. Louis-Jean J, Cenat K, Sanon D, Stvil R. Coronavirus (COVID-19) in Haiti: A Call for Action. J Community Health. 2020;45(3):437-439. doi:10. 1007/s10900-020-00825-9
33. Chilumpha M, Chatha G, Umar E, et al. ‘We stay silent and keep it in our hearts’: a qualitative study of failure of complaints mechanisms in Malawi’s health system. Health Policy Plan. 2023;38(Supple ment_2):ii14-ii24. doi:10.1093/heapol/czad043
34. United Nations. Overcoming COVID myths and fears in Malawi. United Nations News: Global perspective Human stories. May 2, 2021. Accessed August 16, 2024.https://news.un.org/en/story/2021/05/1090972
35. Olaniran A, Banke-Thomas A, Bar-Zeev S, Madaj B. Not knowing enough, not having enough, not feeling wanted: Challenges of community health workers providing maternal and newborn services in Africa and Asia. Tappis H, ed. PLOS ONE. 2022;17(9):e0274110. doi:10.1371/journal. pone.0274110
36. Wake AD. The Acceptance Rate Toward COVID-19 Vaccine in Africa: A Systematic Review and Meta-analysis. Glob Pediatr Health. 2021;8:23 33794X2110487. doi:10.1177/2333794X211048738
37. Feldman M, Lacey Krylova V, Farrow P, et al. Community health worker knowledge, attitudes and practices towards COVID-19: Learnings from an online cross-sectional survey using a digital health platform, UpSCALE, in Mozambique. Di Gennaro F, ed. PLOS ONE. 2021;16(2):e0244924. doi:10.1371/journal.pone.0244924
38. Li Y, Liu G, Egolet RO, Yang R, Huang Y, Zheng Z. Knowledge, Attitudes, and Practices Related to COVID-19 Among Malawi Adults: A Community-Based Survey. Int J Environ Res Public Health. 2021;18(8):4090. doi:10.3390/ijerph18084090
39. Kainja J, Makhumula C, Twabi HS, Gunde AM, Ndasauka Y. Cultural determinants of COVID-19 vaccines misinformation in Malawi. Humanit Soc Sci Commun. 2024;11(1):1193. doi:10.1057/s415 99-024-03743-6
40. Magagula A. Level of knowledge about COVID-19 and vaccines among CHWs in Malawi. Published online July 25, 2024.
41. Faure JA, Wang CW, Chen CHS, Chan CC. Assessment of the Functional Capacity and Preparedness of the Haitian Healthcare System to Fight against the COVID-19 Pandemic: A Narrative Review. Healthcare. 2022;10(8):1428. doi:10.3390/ healthcare10081428
42. Miller J. Sustaining Health Care as Crisis in Haiti Escalates. Harvard Medical School. March 21, 2024. Accessed October 26, 2024. https://hms.harvard.edu/news/sustaining-health-care-crisis-haiti-escalates
43. Al-Hanawi MK, Angawi K, Alshareef N, et al. Knowledge, Attitude and Practice Toward COVID-19 Among the Public in the Kingdom of Saudi Arabia: A Cross-Sectional Study. Front Public Health. 2020;8:217. doi:10.3389/fpubh.2020.00217
44. Zhong BL, Luo W, Li HM, et al. Knowledge, attitudes, and practices towards COVID-19 among Chinese residents during the rapid rise period of the COVID-19 outbreak: a quick online cross-sectional survey. Int J Biol Sci. 2020;16(10):1745-1752. doi:10.7150/ijbs.45221
45. Yoseph A, Tamiso A, Ejeso A. Knowledge, attitudes, and practices related to COVID-19 pandemic among adult population in Sidama Regional State, Southern Ethiopia: A community based cross-sectional study. Erbil N, ed. PLOS ONE. 2021;16(1):e0246283. doi:10.1371/journal. pone.0246283
46. Azlan AA, Hamzah MR, Sern TJ, Ayub SH, Mohamad E. Public knowledge, attitudes and practices towards COVID-19: A cross-sectional study in Malaysia. Tu WJ, ed. PLOS ONE. 2020;15 (5):e0233668. doi:10.1371/journal.pone.0233668
47. Kaungav SB. How have Malawi’s courts affected the country’s epidemic response? The London School of Economics and Political Science (LSE). November 13, 2020. https://blogs.lse.ac.uk/africaatlse/2020/11/13/how-have-malawis-courts-law-affected-epidemic-response/
48. Mzumara GW, Chawani M, Sakala M, et al. The health policy response to COVID-19 in Malawi. BMJ Glob Health. 2021;6(5):e006035. doi:10.1136 /bmjgh-2021-006035
49. Moradzadeh R, Nazari J, Shamsi M, Amini S. Knowledge, Attitudes, and Practices Toward Coronavirus Disease 2019 in the Central Area of Iran: A Population-Based Study. Front Public Health. 2020;8:599007. doi:10.3389/fpubh.2020.599007
50. Pan American Health Organization (PAHO). Haiti receives 500,000 vaccines donated by the United States through COVAX. PAHO: Pan American Health Organization. Accessed July 8, 2024. https://www.paho.org/en/stories/haiti-receives-500000-vaccines-donated-united-states-through-covax
51. World Health Organization. WHO COVID-19 dashboard. World Health Organization Data. Accessed October 26, 2024. https://data.who.int/dashboards/covid19/vaccines
52. Nkambule E, Mbakaya BC. COVID-19 vaccination hesitancy among Malawians: a scoping review. Syst Rev. 2024;13(1):77. doi:10.1186/s1364 3-024-02499-z
53. Sethy G, Chisema MN, Sharma L, et al. ‘Vaccinate my village’ strategy in Malawi: an effort to boost COVID-19 vaccination. Expert Rev Vaccines. 2023;22(1):180-185. doi:10.1080/14760 584.2023.2171398
54. Bwanali AN, Lubanga AF, Mphepo M, Munthali L, Chumbi GD, Kangoma M. Vaccine hesitancy in Malawi: a threat to already-made health gains. Ann Med Surg. 2023;85(10):5291-5293. doi:10.1097/ MS9.0000000000001198
55. Goel K, Sen A, Goel P, et al. Assessment of COVID-19 Vaccination Intention Among Community Health Workers: a Web-based Cross-sectional Survey During the First Wave of the Pandemic in India. Published online July 8, 2021. doi:10.21203 /rs.3.rs-675407/v1
56. Avahoundje EM, Dossou JP, Vigan A, et al. Factors associated with COVID-19 vaccine intention in Benin in 2021: A cross-sectional study. Vaccine X. 2022;12:100237. doi:10.1016/j.jvacx. 2022.100237
57. Eyal K, Njozela L, Köhler T, et al. Correlates of COVID-19 vaccination intentions and opinions about mandates among four groups of adults in South Africa with distinct vaccine intentions: evidence from a large national survey. BMC Public Health. 2023;23(1):1767. doi:10.1186/s12889-023-16584-w
58. Nomura S, Eguchi A, Yoneoka D, et al. Reasons for being unsure or unwilling regarding intention to take COVID-19 vaccine among Japanese people: A large cross-sectional national survey. Lancet Reg Health – West Pac. 2021;14:100223. doi:10.1016/j. lanwpc.2021.100223
59. Sánchez-González L, Major CG, Rodriguez DM, et al. COVID-19 Vaccination Intention in a Community Cohort in Ponce, Puerto Rico. Am J Trop Med Hyg. 2022;107(2):268-277. doi:10.4269/ ajtmh.22-0132
60. PIH’s Strategy for Achieving Equity in COVID-19 Vaccination. Partners In Health. Accessed November 14, 2024. https://www.pih.org/learning-collaborative/pihs-strategy-achieving-equity-covid-19-vaccination
61. Warren AM, Bennett MM, Da Graca B, et al. Intentions to receive COVID-19 vaccines in the united states: Sociodemographic factors and personal experiences with COVID-19. Health Psychol. 2023;42(8):531-540. doi:10.1037/hea0001225