COVID-19 and Myocarditis: Challenges in Diagnosis and Care
Covid 19 and myocarditis – current challenges: Myocardial damage vs acute myocarditis
Prof. dr. Sci. Ivan Malčić, MD, PhD1
OPEN ACCESS
PUBLISHED:30 December 2024
CITATION: MALČIĆ, Prof. dr. Sci. Ivan. Covid 19 and myocarditis – current challenges: Myocardial damage vs acute myocarditis. Medical Research Archives, [S.l.], v. 12, n. 12, dec. 2024. Available at: <https://esmed.org/MRA/mra/article/view/5971>. Date accessed: 02 nov. 2025. doi: https://doi.org/10.18103/mra.v12i12.5971.
COPYRIGHT: © 2025 European Society of Medicine. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
DOI: https://doi.org/10.18103/mra.v12i12.5971
ISSN 2375-1924
ABSTRACT
Background: Coronavirus infection disease 2019 (COVID-19) is a disease caused by Severe Acute Respiratory Syndrome coronavirus 2 (SARS-CoV-2), which has rapidly spread worldwide in December 2019. Besides the symptoms of acute respiratory distress and multiorgan failure, the cardiac involvement with acute myocardial injury is also a possible clinical scenario(1) Despite the initial opinion that high troponin levels increase mortality in patients, it is clear today that abnormal troponin are not necessarily a sign of acute myocarditis. The aim of this presentation is to show the diagnostic process for the occurrence of myocarditis in Covid-19 infection compared to the diagnostic process for myocarditis with other viruses called cardiotropic viruses.
The presentation refers mainly to the desire for paediatric cardiologists to learn about the fundamental difference in the approach to a child with SARS-CoV-2 compared to myocarditis of another etiolgy. From daily practice, it seems that with Covid-19 infection, more attention is paid to possible damage to the myocardium (due to elevated troponin levels), and too little attention is paid to other symptoms. This primarily refers to coagulation disorders that can develop diffuse intravascular coagulopathy as circulus vitiosus with tragic consequences.
This presentation is the experience from the perspective of paediatric cardiologists and has no basis for statistical analysis. It is aimed at the need for scientific research into the causes and consequences of various changes in the heart musculature caused by Covod-19 infection (most often in the context of multisystem inflammatory syndrome) in relation to extensive changes in the heart musculature in the case of infection with cardiotropic viruses.(2,3)
Keywords
COVID-19, myocarditis, cardiovascular involvement, children, adolescents
Introduction
COVID-19 is rare in paediatric patients, with incidence of less than 1% in children and adolescents below the age of 10. The main serious complication in children affected by the disease is multisystemic inflammatory syndrome (MIS-C). This syndrome had a cardiovascular involvement in 80–100% of cases in adults, with mortalities occurring in 67% of patients. The aim of this presentation is to highlight the cardiovascular involvement in children and adolescents with COVID-19 since this has the morbidity and mortality potential in this age group.
The heart cannot be viewed as an isolated organ damaged by the corona virus, without knowing that it is SARS and MSI.¹²³⁴⁵
PATHOGENESIS OF CARDIOVASCULAR INJURY CAUSED BY SARS-CoV-2
This viral infection causes damage to the heart in several ways. The primary mechanism of heart damage is cardiotoxicity due to the entry of viruses into the heart tissues, consequent hypoxia, and side effects of drugs administered in therapy. It has been proven that the direct viral invasion of the COVID-19 virus is caused by the binding of the virus to the ACE2 receptors on the surface of the heart.
This is proven by a post-mortem study where spherical virus particles are found in the heart tissue on electron microscopy, and it is also confirmed in the heart of deceased SARS patients by reverse transcriptase-polymerase chain reaction (RT-PCR).⁵⁶ Therefore, it is believed that severe acute SARS-CoV-2 infection is associated with changes in the ACE2 receptor and the way the virus enters the intracellular medium.
After being infected with this virus, excessive release of cytokines or T-cell dysregulation occurs, resulting in microvascular damage and endothelial dysfunction. The increased level of cytokines and the release of inflammatory mediators reduce heart contractility, cause peripheral vasodilation, and thus cause hemodynamic instability. General symptoms after cardiovascular damage belong to the group of MIS symptoms.⁶ The findings of cardiac biomarkers and inflammatory markers are correlated with the severity of damage and activation of Th1 lymphocytes.
It is interesting that the latest reports on myocarditis caused by the COVID-19 virus speak of a sudden positive change in the use of immunomodulatory drugs (intravenous corticosteroids and immunoglobulins), but only in some patients. This remark corresponds to a much earlier experience in the history of knowledge about myocarditis, from the early 80s of the 20th century.
According to this experience, about 50% of patients with severe cardiomyopathy in the acute course of myocarditis caused by other cardiotropic viruses (e.g., coxsackie) suddenly improve with the use of corticosteroids, and in 50% the condition worsens. **The answer should be sought precisely in the findings of the virus in heart cells using the RT-PCR method.**⁷⁸
It is also plausible that SARS-CoV-2 infection increases the risk of thromboembolic and ischemic events. Although the mechanism of coagulopathy is unclear, it is likely to be multifactorial. Previous studies have shown that infections with other coronaviruses also elevated other components of the fibrinolysis pathway and regulated the genes associated with the induction of a procoagulant factor.
Patients with previous congenital heart disease are most prone to coagulation changes. Disseminated intravascular coagulation also causes myocardial injury and has been characterized in post-mortem biopsies of patients with SARS.⁸
SPECTRUM OF CLINICAL SYMPTOMS (COVID-19 MYOCARDITIS AND CARDIOVASCULAR SYSTEM)
For the clinical diagnosis of myocarditis, ECG, ECHO, MR, and cardiac enzymes should be performed, considering that troponin is defined as a marker of cardiac damage in children and adolescents.
Myocarditis and pericarditis are found in 40% and 25% of patients, and combined with the findings of myocardial dysfunction, they suggest pan-carditis, which has an increased risk and a worse outcome than in the case of COVID-19 infection.
Simultaneous arrhythmias due to hypoxia, neurohormonal and humoral stress, and metabolic changes are possible. Some drugs given without sufficient experience, such as hydroxychloroquine, can worsen arrhythmias
Inflammatory cytokines cause peripheral vasodilation and consequent hemodynamic instability.
More than 25% of patients develop venous thrombosis, especially those who have increased D-dimers, inflammatory markers, decreased fibrinogen, and acute respiratory syndrome.
Coronary thrombosis and an increased risk of coronary ischemia can also develop.
After this description, it is clear that in case of infection with the COVID-19 virus, the heart should not be considered as a myocarditis isolated from symptoms in other organs, especially in the case of severe coagulation disorders.
Imaging Findings
Diagnostic Methods
TTE is the most common diagnostic method for detecting cardiovascular changes in children and adolescents with COVID-19.
In most reports, changes are found in the left ventricle (LV) with reduced ejection fraction (EF), including mitral regurgitation, pericardial effusion, and hypokinesia of the inferior septal and inferior walls.
Treatment can achieve complete normalization in a very short time. However, there are also extreme coronary aneurysms (14.5%) and patients with cardiac shock.
That’s why TTE serves as an initial test to evaluate EF, coronary aneurysm, and pericardial effusion.
MRI reads functional and morphological changes, and with gadolinium staining, can find areas of necrosis or fibrosis in the myocardium in 50% of children with COVID-19 myocarditis.
CT helps to rule out intracardiac thrombus and endocarditis, and diagnose pulmonary thromboembolism.
Myocardial Biopsy and Histology
In one large study that includes as many as 353 publications, only 38 patients were found in whom the diagnosis of myocarditis was proven or suspected according to the valid WHO/ISFC criteria, which includes the so-called Dallas criteria.
Endomyocardial biopsies (EMB) were performed only in 8 patients.
In only one case was the finding of SARS-CoV-2 in the cardiomyocyte clearly described based on the Dallas criteria, but it was not stated whether an RT-PCR test was performed.
Histology demonstrates myocardial inflammation with a predominance of macrophages, and myocyte necrosis was instead limited.
The case presented clinically as acute myocarditis with cardiogenic shock, and EMB results suggest viral mediation of inflammation without significant direct myocyte destruction.
Histological evidence of SARS-CoV-2 was also found in 5 of 104 EMBs with suspected myocarditis or heart failure; however, only 2 met the Dallas criteria for myocarditis.
Autopsy histologic data were also available in 4 patients and included accumulation of inflammatory cells in the endothelium, inflammatory infiltrates, and signs of ferroptosis (regulated cell death due to iron accumulation).
WHO/ISFC – Dallas Criteria (1986)
Pathohistological Criteria (Four Forms)
-
Active: Myocyte degeneration, necrosis, and cellular infiltration
-
Borderline: Cellular infiltration without damage to the heart muscle
-
Persistent: Inflammatory infiltration even after repeated biopsy
-
Resolution: Reduction or disappearance of inflammation with connective tissue transformation on control biopsies
The criteria have relatively low sensitivity and specificity despite their wide application.
New Knowledge
-
Virus may be present in the heart despite scant cellular infiltration.
-
The Dallas criteria may cause incorrect determination of the severity of infection depending on the circumstances of the final outcome.
-
For final diagnostic accuracy, a reasonable schedule of biopsies between traditional histological imaging and immune-histological and virological diagnostics — molecular genetics is suitable.
In the following pictures, we show great differences in the histological findings in a child who experienced cardiogenic shock during a COVID-19 infection, without a visible inflammatory process, myocyte necrosis, or inflammatory infiltrates (Fig. 1).
On the contrary, a child who had acute myocarditis caused by a cardiotropic virus (Coxsackie) has a completely different picture, in which eosinophils, lymphocytes, and plasma cells dominate, and the muscles are edematous (Fig. 2).⁸,¹¹
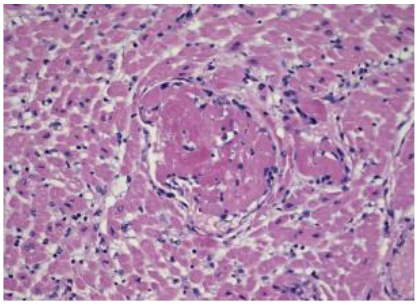
Fig. 1.
Microscopic study of the heart from a deceased patient with COVID-19 and cardiogenic shock in Bergamo, Italy.
Numerous microthrombi of the left ventricle are shown without evidence of an inflammatory infiltrate;
the detection on tissue by molecular technique for SARS-CoV-2 was negative.
Collectively, the diagnosis of COVID-19-related myocarditis was excluded in view of the thorough histological evaluation that proved **absence of myocyte necrosis and inflammatory infiltrate.**⁸
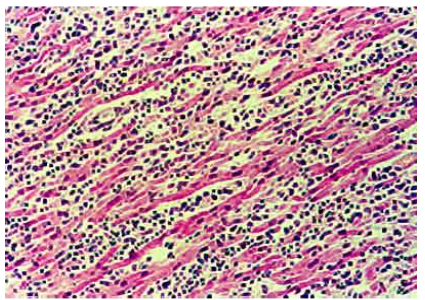
Fig. 2.
Acute myocarditis – light microscopy (Dallas criteria); shows massive interstitial infiltrates of lymphocytes, plasma cells, and eosinophils.
Muscle fibers are partially edematous and hypereosinophilic.
*HE, enlargement 100x.*¹¹
MYOCARDIAL DAMAGE vs ACUTE MYOCARDITIS
Elevated troponin basically marks myocarditis, but it is not possible to determine if the elevated troponin level is caused by inflammation or non-inflammatory etiological factors.
In the absence of myocardial ischemia, a significant increase in troponin can be an indication for observation of acute myocarditis only in the appropriate clinical context.
Under normal circumstances, there is a series of diagnostic procedures for suspected myocarditis according to the latest literature. However, the mentioned imaging methods also leave doubts if the etiological factors are not certain.
This means that a definitive diagnosis with a high degree of sensitivity cannot be made when myocarditis is suspected (Fig. 3).⁷,⁹,¹¹
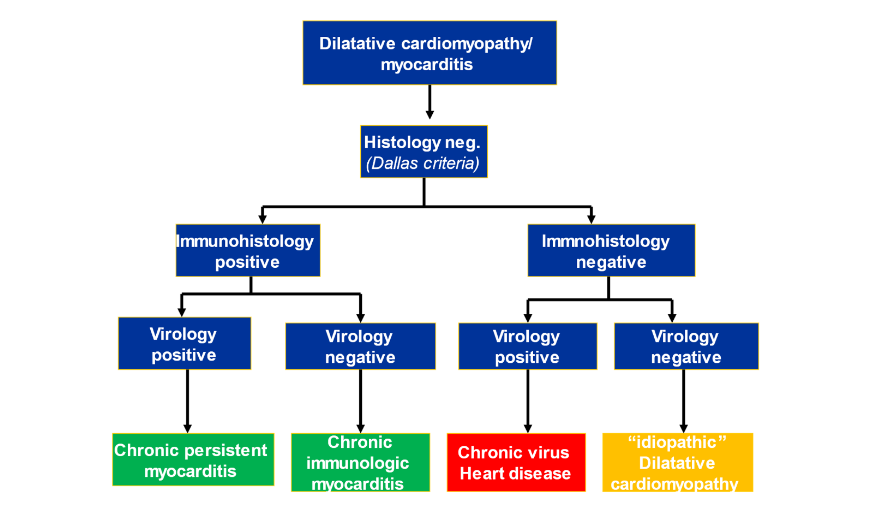
Fig. 3. Flow-diagram for diagnosis of cardiomyopathy and myocarditis.
Conclusions
MIS-C or SARS-CoV-2 infection with myocardial involvement has a worse prognosis, but isolated myocarditis does not necessarily indicate a poor prognosis.However, given the paucity of published data, the inhomogeneity of cases, and the neglect of the basic criteria for the diagnosis of viral myocarditis in paediatric cardiology, no firm conclusion can be made about the importance of myocarditis in COVID-19 virus infection.There is also limited knowledge about the use of immunosuppressants without a myocardial biopsy and RT-PCR test of the biopsy itself. Colchicine is also under question, and the positive action in myocarditis remains only an assumption.Even though in many cases it is not possible to prove a causal relationship between SARS-CoV-2 infection and myocarditis, the latest histological data speak of a direct viral infection of cardiomyocytes.This evidence of myocarditis with and without direct myocyte damage suggests that different pathophysiological mechanisms are responsible — either COVID-mediated development of myocarditis or a therapeutic approach as the cause.It seems that myocardial biopsy in cases of suspected COVID-19 myocarditis should become the subject of large-scale studies.The current views on the diagnosis of myocarditis, as well as the guidelines for proper treatment, remain unsatisfactory.It is already logical to assume that patients who do not have a virus in the heart muscle, but only an inflammatory process stimulated by the virus, could benefit significantly from treatment with immunosuppressants, according to the views of paediatric cardiologists in cases of myocarditis caused by other **cardiotropic viruses.**⁵⁶¹¹
Conflict of Interest:
None
Acknowledgements:
None
References
1. Maques do Vele Kapucho AC, Silva Resende PL, Mascarenhas DA, Rodrigues da Silva CLM, Sawamura KSS et al. Cardiac manifestations in pediatric Covid-19. Clinics 2021;76:e3001
2. Pereira MFB, Litvinov N, Farhat SCL, Eisencraft AP, Gibelli MABC, Carvalho et al. Clinical spectrum with high mortality in pediatric patie with COVID-19and multisystem inflamatory sindrome. Clinics (Sao Paulo). 2020;75:e2209
3. Safadi MAP, Silva CAAD. The challenging and unpredictable spectrum of COVID-19 in children and adolescents. Rev Paul Pediatr. 2020; 39:e202 0192.
4. Feldstein LR, Rose EB, Horwitz SM, Collins JP, Newhams MM, Son MBF,et al. Multisystem Inflammatory Syndrome in U.S. Children and Adolescents. N Engl J Med. 2020;383(4):334-46.
5. Fremed MA, Lytrivi ID, Liberman L, Anderson BR, Barry OM, Choudhury TA, et al. Cardiac workup and monitoring in hospitalised children with COVID- 19. Cardiol Young. 2020;30(7):907-10.
6. Dolhnikoff M, Ferreira Ferranti J, de Almeida Monteiro RA, Duarte-Neto AN, Soares Gomes-Gouvêa M, Viu Degaspare N, et al. SARS-CoV-2 in cardiac tissue of a child with COVID-19-related multisystem inflammatory syndrome. Lancet Child Adolesc Health. 2020;4(10):790-4
7. Sandoval Y, Januzzi JL Jr, Jaffe AS. Cardiac Troponin for Assessment of Myocardial Injury in COVID-19: JACC Review Topic of the Week. J Am Coll Cardiol. 2020;76(10):1244-58.
8. Castiello T, Georgiopoulos G, Finocchiaro G, Claudia M, Andrea Gianatti A, Delialiss D et al. COVID 19 and myocarditis: a systematic review and overview of current challenges. Heart Failure Reviews (2022) 27:251–261.
9. Henderson LA, Canna SW, Friedman KG, Gorelik M, Lapidus SK,Bassiri H, et al. American College of Rheumatology Clinical Guidance for Multisystem Inflammatory Syndrome in Children Associated With SARS-CoV-2 and Hyperinflammation in Pediatric COVID-19: Version 1. Arthritis Rheumatol. 2020;72(11):1791-805.
10. Aretz HT, Billingham ME, Edwards WD, Factor SM, Fallon JT, Fenoglio JJ Jr, Olsen EG, Schoen FJ. Myocarditis: a histopathologic definition and classification. Am J Cardiovasc Pathol. 1987; 1: 3–14.
11. Malčić I, Jelašić D, Šarić D i sur. Dijagnostička vrijednost biopsije miokarda i suvremena analiza bioptata u dijagramu dijagnostičkog toka primarnih i drugih kardiomiopatija u djece. Diagnostic value of myocardial biopsy in the diagnostic algorithm in cardiomyopathies in children. Liječ Vjesn 2004;26: 227–34.

