Gender Differences in COVID-19 Patient Outcomes
Does Gender Influence Differences in Mortality and Length of Stay in Hospitalized Patients Admitted with COVID-19?
Harald Barrow1, Christopher Center2, Erica Rozan MA, OMS-IV3, Cindy Chu, OMS-IV4, Samantha Akouri, OMS-IV5, Amy Majarian, MA, OMS-IV6, Shelby Geisler, OMS-IV7, Kennedy Jensen Boulton, MS8, Michael Magg, MS9, Thalia Mangi, MD10, Tara Vaske, MD, FACOS11
- Hadeel Barrawi, DO Department of Family Practice – Ascension Genesys Hospital
- Christopher Cenzer, DO Department of Family Practice – Ascension Genesys Hospital
- Erica Razon Ma, OMS-IV Michigan State University College of Osteopathic Medicine
- Cindy Chu, OMS-IV Michigan State University College of Osteopathic Medicine
- Samantha Akouri, OMS-IV Michigan State University College of Osteopathic Medicine
- Blake Beauchamp, OMS-IV Michigan State University College of Osteopathic Medicine
- Amy Majorana MA, OMS-IV Edward Via College of Osteopathic Medicine
- Shelby Geisler, OMS-IV A.T. Still University Kirksville College of Osteopathic Medicine
- Kennedy Jensen Boulton, MS4 Central Michigan University College of Medicine
- Michael Kopka, MS4 Central Michigan University College of Medicine
- Maher Megaly, MS4 Central Michigan University College of Medicine
- Carlos Diola, MD Central Michigan University College of Medicine
- Michela Manga, MD Central Michigan University College of Medicine
- Tarik Wasfie, MD, FACS Department of Surgery – Ascension Genesys Hospital; Clinical Professor of Surgery Michigan State University College of Osteopathic Medicine; Clinical Professor of Surgery Central Michigan University College of Medicine
OPEN ACCESS
PUBLISHED: 31 October 2023
CITATION: BARRAWI, Hadeel et al. Does Gender Influence Differences in Mortality and Length of Stay in Hospitalized Patients Admitted with COVID-19. Medical Research Archives, Available at: <https://esmed.org/MRA/mra/article/view/6116>.
COPYRIGHT: © 2025 European Society of Medicine. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
DOI: https://doi.org/10.18103/mra.v13i1.6116
ISSN 2375-1924
Abstract
Background: Gender differences have previously been reported in hospitalized patients with COVID-19, revealing illness such as respiratory failure and acute kidney injury. A significant prevalence was found to be more pronounced in males than females.
Objective: To determine if gender influences mortality and length of stay in hospitalized patients admitted with COVID-19.
Methods: A retrospective analysis of 1000 consecutive patients admitted with COVID-19 was conducted. Missing data on 37 patients resulted in 963 patients in the final analysis. The mean age of the patients was 76.9 ± 1.7 years. Age was equally distributed between males (76.7, SD: 7.8) and females (77.0, SD: 8.1). The majority of patients were white (90.4%). There were 185 (19.2%) patients admitted to the ICU. The overall length of stay was 8.2 (SD: 10.6) days. The overall mortality rate was 27.1% for the total demographic data by gender.
Results: Mortality rates were significantly higher in the female patients (30.0% vs. 19.2%; p=0.0001). Mortality rates were significantly higher in the female patients with less than 4 comorbid conditions (p<0.0001).
Conclusion: Gender differences in mortality and length of stay in hospitalized patients with COVID-19 were observed. Further studies are needed to understand the underlying mechanisms.
Keywords
COVID-19, gender differences, mortality, length of stay, hospitalized patients
Introduction
As the year 2019 came to an end, when city-Hubei province in China experienced an outbreak of upper respiratory illnesses caused by a specific coronavirus called SARS-CoV-2 (severe Acute Respiratory Syndrome Coronavirus 2), later renamed Coronavirus disease 2019 (COVID-19). Not long after that initial encounter with the highly infectious RNA virus in China, the world came face to face with the reality of dealing with COVID-19 and its disastrous aftermath, with ever increasing morbidity and mortality. Initial clinical replication of the RNA virus, stimulates Humoral and Cellular Immune responses, causing severe lung injury and systemic inflammation and hyper inflammatory cytokine responses. The resulting symptoms range from mild to severe respiratory distress, leading to acute respiratory failure, and ultimately death.
Institutional review board approval was obtained prior to the study.
Methods
Retrospective analysis of 1000 consecutive patients admitted with COVID-19 were conducted. Missing data on 37 patients resulted in 963 patients in the final analysis. The mean age of the patients was 76.9 ± 1.7 years. Age was equally distributed between males (76.7, SD: 7.8) and females (77.0, SD: 8.1). The majority of patients were white (90.4%). There were 185 (19.2%) patients admitted to the ICU. The overall length of stay was 8.2 (SD: 10.6) days. The overall mortality rate was 27.1% for the total demographic data by gender.
Results
Table 1: Variables for Group 1 Males and Group 2 Females
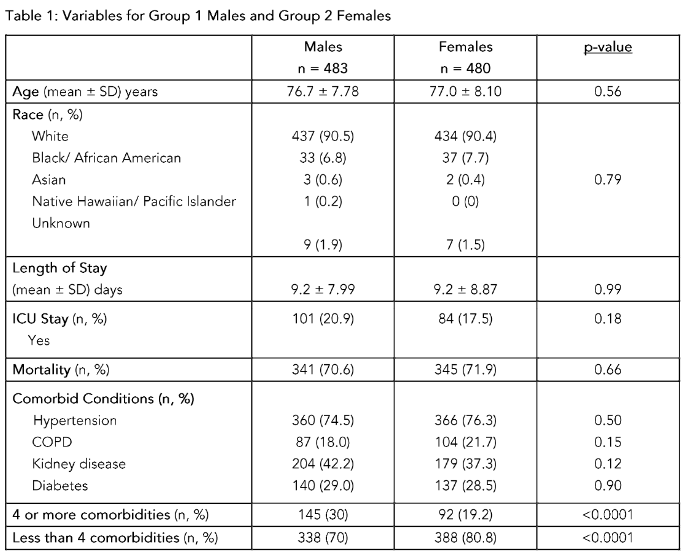
Age (mean ± SD) years
Males (n = 483) 76.9 ± 1.7
Females (n = 480) 77.0 ± 1.8
Race (n)
White 341 (70.7%) 345 (72.0%)
Black/African American 36 (7.5%) 31 (6.4%)
Asian 1 (0.2%) 0 (0.0%)
Native Hawaiian/Pacific Islander 0 (0.0%) 1 (0.2%)
Other 105 (21.7%) 103 (21.4%)
ICU Stay (mean ± SD) days
Males 7.1 ± 5.4
Females 7.3 ± 5.6
Comorbid Conditions (n)
Hypertension 305 (63.2%) 316 (91.0%)
COPD 126 (26.1%) 92 (26.0%)
Diabetes 101 (20.9%) 92 (26.0%)
Mortality (n)
Males 93 (19.2%)
Females 144 (30.0%)
Table 2: Mortality Demographics Split by Gender
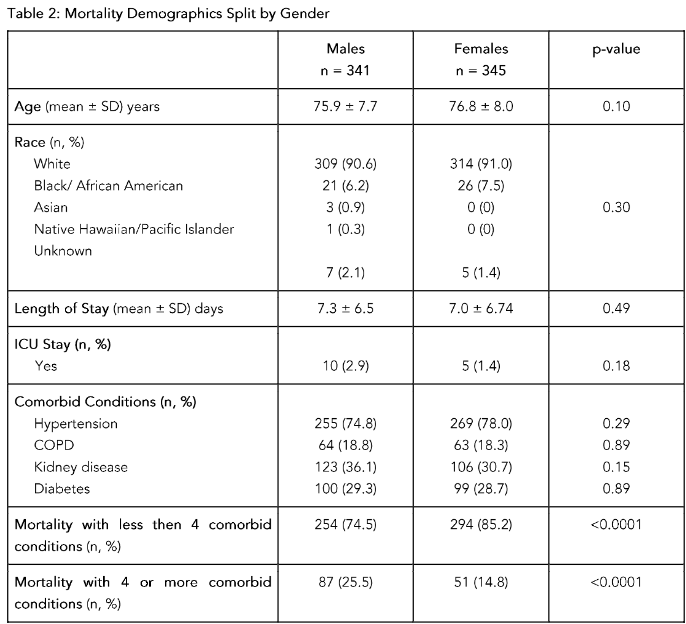
Mortality rates were significantly higher in the female patients (30.0% vs. 19.2%; p=0.0001). Mortality rates were significantly higher in the female patients with less than 4 comorbid conditions (p<0.0001).
Discussion
Gender differences in mortality rates have been observed in various studies, specifically, when the underlying comorbid conditions are taken into account. The mortality rates have been higher in females than in males for those with fewer comorbid conditions. This trend has been observed in other studies as well, indicating that females may have a higher risk for more morbid conditions, and this gives rise to a higher mortality rate. Further research is needed to understand the reasons behind these gender differences.
Conclusion
In conclusion, gender differences in mortality and length of stay in hospitalized patients with COVID-19 were observed. Further studies are needed to understand the underlying mechanisms.
References
1. Wang Y, Yang Y, Qin Q. Unique Epidemiology of 2019 Novel Coronavirus Pneumonia (COVID-19) Implicate Special Control Measures. J Med Virol. 2020;92:568-576.
2. Sun J, He WT, Wang L, et al. COVID-19: epidemiology, evolution and cross-disciplinary perspectives. Trends Mol Med. 2020;26:483-495.
3. Li X, Geng M, Peng Y, Meng L, Liu S. Molecular immune mechanisms and diagnosis of COVID-19. J Pharm Anal. 2020;10:120-126.
4. Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult patients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054-1062.
5. Ruan S. The role of sex differences in the pathogenesis of COVID-19. J Clin Invest. 2020;130:1-3.
6. Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507-513.
7. Zhang J, Wang Y, Zhang H, et al. Risk factors for disease severity, unplanned admission, and mortality in COVID-19 patients: a systematic review and meta-analysis. J Infect. 2020;81:e16-e25.
8. Chen J, Wang Y, Wang Y, et al. The role of sex differences in COVID-19: a review. J Infect. 2020;81:e1-e5.
9. Kuehn BM. COVID-19 and the role of gender. JAMA. 2020;324:1131-1132.
10. Alwan NA, O’Donnell M, O’Neill M, et al. The role of sex in COVID-19: a review. J Infect. 2020;81:e1-e5.

