Evolving Definitions of Disease: Implications for Health Care
General concepts of disease
Dr Ricardo F Gonzalez-Fisher, MD, MPH, FACS, Dr Steve Rissman, ND, Dr Paris Theresa Prestridge, ND
Metropolitan State University of Denver, College of Health and Human Sciences, Campus Box 8, P.O. Box 173362, Denver, CO 80217-3362
OPEN ACCESS
PUBLISHED 31 August 2025
CITATION Gonzalez-Fisher, RF., Rissman, S., Prestridge, PT., 2025. General concepts of disease. Medical Research Archives, [online] 13(8). https://doi.org/10.18103/mra.v13i8.6912
COPYRIGHT © 2025 European Society of Medicine. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
DOI https://doi.org/10.18103/mra.v13i8.6912
ISSN 2375-1924
ABSTRACT
complete physical, mental, and social well-being, shifting the perception of disease from an accepted part of life to a deviation from an ideal of optimal wellness. This contrasts with the biomedical model, which defines health as merely the absence of disease, often overlooking psychological, societal, or environmental influences.
The definition of “disease” continues to present conceptual challenges within both societal discourse and clinical practice. Its boundaries are fluid, shaped over time by shifting cultural expectations of health, advances in diagnostic technologies, and complex socio-economic dynamics. Despite the emergence of various theoretical frameworks, ranging from statistical abnormality and functional impairment to social valuation and clinical categorization, a universally accepted definition has yet to be established.
Under the leadership of Robert F. Kennedy Jr. at the U.S. Department of Health and Human Services, the concept of disease is being reshaped to emphasize environmental factors, such as food additives and seed oils, over established biomedical causes. This shift challenges healthcare providers to integrate new frameworks into their practice while raising concerns about diverting focus from evidence-based medical interventions.
With global healthcare expenditures reaching US$9.8 trillion in 2021, accounting for one in every ten dollars of GDP, disease classification has substantial economic and societal implications. A universally applicable and holistic definition is necessary to guide healthcare providers, policymakers, and patients in navigating these evolving perspectives while ensuring the delivery of adequate medical care.
Keywords: Disease and illness, normality, diagnosis, caregiver, philosophy of medicine.
THE EUROPEAN SOCIETY OF MEDICINE
Medical Research Archives, Volume 13 Issue 8
EDITORIAL
General concepts of disease
Introduction
People’s lives were often shaped by health and leisure, struggle and rest, excitement and monotony, but primarily by the daily challenges of existence centered around family, birth, death, disease, and health. In earlier times, disease was an accepted part of life, an inevitable reality rather than a condition to be eradicated. However, in 1946, the World Health Organization (WHO) redefined health as “a state of complete physical, mental, and social well-being and not merely the absence of disease or infirmity.” This marked a significant shift, transforming disease from a routine aspect of life into a deviation from an aspirational state of wellness. Despite this expanded definition of health, the WHO has yet to offer a clear, universally accepted definition of disease.
This paper explores the evolving understanding of disease throughout history, tracing how it has been defined and redefined over time. We contrast traditional, binary notions of health and disease with contemporary perspectives that recognize them as points on a continuum. To illustrate this, we present wellness and illness as dynamic and interconnected rather than opposing states. While some continue to define disease as a deviation from biological or statistical normality, we critique the limitations of these definitions, questioning what constitutes “normal” and highlighting the ambiguity and subjectivity in labeling deviations as pathological.
Defining disease carries significant economic and societal implications, particularly in the context of rising global health expenditures. According to the World Health Organization, global health spending reached US$9.8 trillion in 2021, accounting for approximately 1 product. This substantial investment underscores the central role of healthcare in national economies and global development. In such a context, the need for a coherent, universally applicable definition of disease becomes increasingly urgent.
A shared conceptual framework is essential not only for guiding clinical decision-making and resource allocation but also for shaping health policy and ensuring equitable access to care. As health systems worldwide face mounting pressures from demographic changes, technological innovation, and economic instability, clarity in disease definition is crucial for maintaining ethical standards, supporting evidence-based practices, and protecting populations from both overmedicalization and neglect.
The definition of disease also carries profound implications not only for patients but also for caregivers, healthcare providers, and society as a whole. As healthcare systems and providers play a central role in shaping what is recognized as a disease, these definitions influence access to care, treatment options, and social perceptions of illness. This conversation is particularly timely, as the H.S.S. department under the new U.S. administration, led by Robert F. Kennedy Jr., redefines disease by prioritizing environmental factors, such as food additives, over established biomedical causes. While this shift encourages a broader view of health, it also risks undermining evidence-based medicine and complicating patient care. Striking a balance between emerging perspectives and scientific rigor is essential.
We do not aim to provide a definitive definition of disease. Instead, we want to foster a necessary academic conversation that encourages healthcare professionals, policymakers, and society to collectively rethink and refine how we define disease and its broader implications.
Disease and illness in history:
Throughout human history, illness except for trauma has been a source of mystery and fear. In early civilizations, it was frequently attributed to malevolent spirits, divine punishment, or imbalances in the forces of nature. The perception of disease as a supernatural or cosmic disturbance reflects humanity’s early attempts to explain suffering in the absence of scientific knowledge. Shamans, regarded as intermediaries between the human and spiritual realms, were tasked with confronting these mysterious forces. Their wisdom, courage, and leadership made them revered figures in their communities. Evidence of their practices, including rudimentary but often effective treatments, can be found in ancient cave paintings dating back to 17,000 BCE. These depictions illustrate early healing rituals and the application of primitive medical interventions, such as wound care and splinting. Moreover, archaeological evidence of trepanation and amputations performed with surprisingly sophisticated skill attests to the early accumulation of medical knowledge. The survival of individuals following complex procedures such as cranial surgery and the treatment of periodontal disease demonstrates that prehistoric medicine, though rudimentary, was not without efficacy. This empirical knowledge, transmitted through oral tradition, laid the foundation for more formalized medical systems in subsequent civilizations.
The transition from mystical interpretations of disease to more systematic, observational approaches is evident in the emergence of written medical texts. By the seventeenth century BCE, ancient Egyptian physicians began documenting medical cases with clinical descriptions and prognostic verdicts. The Edwin Smith Surgical Papyrus, the oldest surviving medical manuscript, represents a pivotal shift toward rational medicine. Containing 48 cases of trauma and illness, the text offers detailed anatomical observations, diagnostic reasoning, and therapeutic recommendations. Notably, it introduces a classification system that distinguishes between treatable conditions, manageable but incurable cases, and terminal diseases. This structured approach, based on empirical observation rather than spiritual speculation, signals the early development of scientific medicine.
Concurrently, other ancient medical systems advanced holistic frameworks for understanding disease. Traditional Chinese Medicine (TCM) and Ayurveda Medicine, both of which persist today, conceptualized health as a dynamic equilibrium between the individual and their environment. In TCM, health was believed to depend on the harmonious flow of qi (vital energy) through meridians, while illness resulted from blockages or imbalances in this flow. Similarly, Ayurveda posited that health was governed by the balance of the three doshas (biological energies): vata, pitta, and kapha. Disease was viewed not as an isolated biological event but as a reflection of disharmony between the body, mind, and environment. These systems employed therapeutic strategies, including herbal remedies, dietary modifications, and mind-body practices, aimed at restoring balance rather than merely treating symptoms. The patient-centered, holistic approach of these ancient traditions presents a striking contrast to the later reductionist models of biomedicine, which primarily focus on disease as a discrete pathological entity.
Similar concepts emerged in ancient Greece, where early physicians challenged supernatural explanations of disease. The Hippocratic school, active in the fourth and third centuries BCE, introduced the theory of humoral medicine, marking a significant departure from mystical interpretations. According to this theory, illness resulted from imbalances among the four bodily humors: blood, phlegm, yellow bile, and black bile. Health, in contrast, reflected the proper balance of these fluids. The Hippocratic corpus emphasized the importance of careful clinical observation and the impact of environmental and lifestyle factors on disease. The emphasis on empirical reasoning, prognosis, and the notion of medicine as an art grounded in systematic observation laid the foundation for modern clinical practice. Interestingly, similarities between humoral medicine and TCM concepts of bodily equilibrium suggest possible exchanges of medical knowledge between the East and West, facilitated by trade routes and cultural interactions between approximately 500 BCE and 1000 CE.
The rise of ancient Rome led to further advancements in public health, highlighting the growing recognition of the connection between environmental conditions and disease prevention. As Rome transitioned from a kingdom to a republic and later to an expansive empire, its leaders implemented public health policies aimed at improving sanitation and controlling the spread of disease. Early Roman laws regulated maternal health and abortion, while large-scale infrastructure projects, such as aqueducts, sewers, and public baths, enhanced sanitation and reduced waterborne illnesses. These public health measures reflected an early understanding of the social determinants of health, marking a significant step toward preventing disease through environmental interventions.
The Industrial Revolution introduced a new paradigm in which health became closely linked to economic productivity. During this period, health was increasingly viewed as an economic asset, valued for its contribution to labor efficiency. Disease, by contrast, was associated with diminished productivity and financial loss. This economic framing of health spurred the development of occupational health regulations aimed at reducing the number of workdays lost to illness. Moreover, the rise of social medicine emphasized the role of social and economic factors in shaping population health, laying the groundwork for contemporary public health interventions.
By the mid-nineteenth century, the advent of germ theory and scientific medicine revolutionized the understanding of disease. Louis Pasteur and Robert Koch demonstrated that specific microorganisms were responsible for infectious diseases, transforming medicine into an increasingly empirical and laboratory-based science. Health was redefined as the absence of identifiable pathogens or physiological dysfunction. However, the Darwinian concept of adaptation introduced a more nuanced perspective, viewing disease as the natural consequence of failed adaptation, a concept that continues to inform contemporary epidemiological models.
In the modern era, health is increasingly recognized as a multidimensional construct encompassing physical, mental, social, and even occupational well-being. Public health advocates emphasize the need to assess health at both individual and societal levels, recognizing the complex interplay between biology, behavior, and social determinants. Nevertheless, defining disease itself remains a contentious issue. Despite significant advances in biomedical science, popular definitions of disease often remain narrow and outdated. For example, some dictionaries still describe disease as a condition that is not limited to infectious diseases, an antiquated definition that excludes the growing burden of chronic, noncommunicable conditions such as cardiovascular disease, diabetes, and cancer.
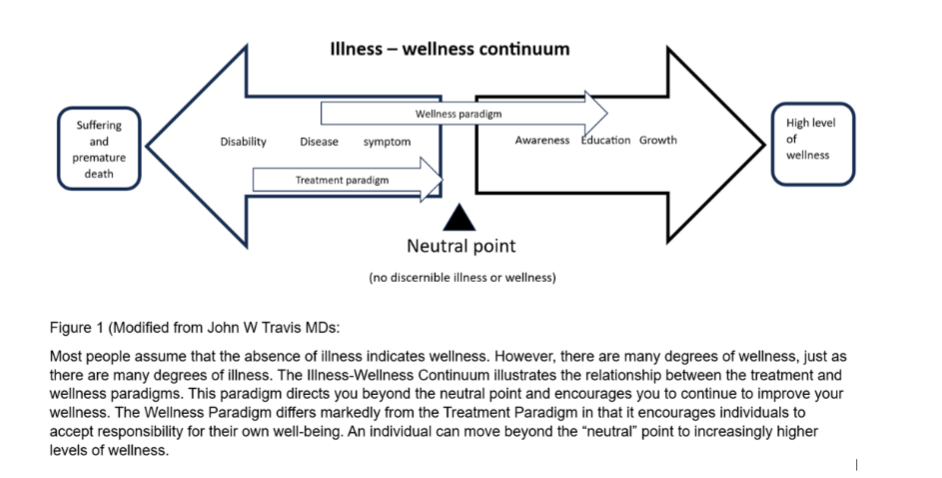
The limitations of binary definitions have prompted the adoption of more fluid, continuum-based models of health and disease. In 1972, John Travis introduced the Illness-Wellness Continuum, which conceptualized health and disease as endpoints on a dynamic spectrum (Figure 1). This model illustrates that individuals can move bidirectionally along the continuum, toward wellness through health-promoting behaviors or toward illness through disease processes. The continuum framework highlights the dynamic nature of health, challenging the notion of disease as a static state.
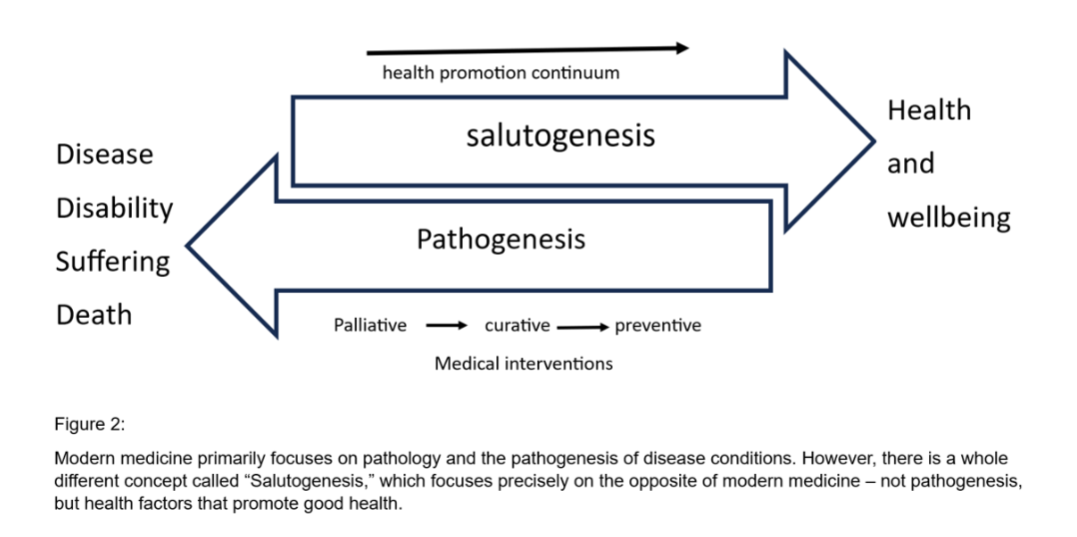
Complementing this continuum model, the salutogenic approach offers an alternative perspective by shifting the focus from disease prevention to health promotion (Figure 2). Developed by Aaron Antonovsky, the salutogenic model emphasizes identifying factors that foster well-being and resilience, even in the presence of illness. Unlike the pathogenic model, which seeks to eliminate disease through external interventions, the salutogenic model prioritizes internal coping mechanisms and adaptability. This perspective encourages healthcare systems to emphasize curative capacity to maintain health and well-being.
Despite these conceptual advancements, contemporary Western medicine relies heavily on diagnostic categorization. The labeling of diseases creates the illusion of neatly defined pathological entities. Nevertheless, disease is rarely a fixed condition; it is often a gradual and evolving process. Many pathological changes occur long before symptoms manifest, and psychological, social, and environmental factors profoundly shape understanding. Illness requires a holistic approach that considers the patient, family dynamics, and lived experiences.
Finally, defining disease merely as a “deviation from normal” introduces further complexities. The concept of “normal” is highly subjective, shaped by cultural norms, medical conventions, and technological advancements. While biomedical models strive for diagnostic precision, they often fail to capture the fluid, personalized, and context-dependent nature of disease. This highlights the need for a broader, more nuanced discourse that critically examines evolving definitions of disease and their implications for patients, caregivers, and healthcare systems alike.
Defining disease
Central to this discourse is the concept of normality, which has become the foundation for assessing health and diagnosing disease. In clinical medicine, the distinction between health and disease is often based on biological or physiological parameters. This distinction carries significant implications for everything from patient self-perception and doctor-patient communication to the goals of clinical interventions, healthcare plans, insurance policies, and public health measures and policy interventions.
In practice, defining disease is far from straightforward, as it can be defined in multiple ways, each with its limitations and consequences. In statistical normality, normality and abnormality are often used to define clinical variables such as basal metabolism, weight, sugar level, height, pulse, and respiration. Any measure beyond the defined normal range is considered an abnormality or a disease condition and signifies the need for medical attention. Where the “normal” body mass index indicates that people are considered overweight or underweight. This standard definition of normal was primarily used in professional settings where it referred to a range of variations known as the “reference” population. This symmetric, bell-shaped distribution of data assumes that the results for a group of presumably healthy people will fit a specific theoretical distribution where most data will fall near the center.
Statistical normality is frequently used to define clinical variables such as basal metabolism, weight, sugar level, height, pulse, and respiration. A disease condition and signifies the need for medical attention. Where the “normal” body mass index indicates that people are considered overweight or underweight. This standard definition of normal was primarily used in professional settings where it referred to a range of variations known as the “reference” population. This symmetric, bell-shaped distribution of data assumes that the results for a group of presumably healthy people will fit a specific theoretical distribution where most data will fall near the center.
Other intervals, such as from zero to the 95th or 99th percentiles, are also often used to define normality. However, this definition assumes that all diseases have the same frequency, which can result in misclassification. For example, imagine a test in which the normal ranges include the lower 95% of test results; the likelihood that a person will be called normal is only about 95%. If the same person undergoes two independent tests with the exact definition of normal, the likelihood that the person will be called normal is 0.90. And so on; in this example, the possibility of being called normal decreases with the number of independent diagnostic tests performed. Thus, a patient who undergoes 20 tests has only about one in three chances of being called normal at the end of the workup.
Recognizing the limitations of statistical methods in defining “normal” to identify disease, clinicians have attempted to define disease based on other criteria, such as functional, symptomatic, pathological, risk factors, therapeutic, culturally desirable traits, disability, or consensus. Unfortunately, these different methods are not free from problems either. Sometimes, risk factors for a disease, such as high blood pressure, eventually get defined as a disease. Once these risk factors are reclassified as a disease, their targets or ranges tend to shift over time.
The definition of disease is based on studies of precursors or statistical predictors of subsequent clinical events; for example, it is well known that high blood pressure is a fundamental cause of many serious cardiovascular diseases, such as cerebrovascular disease and coronary artery disease. The definition of “normal” blood pressure (systolic blood pressure < 140 mmHg and diastolic blood pressure < 90 mmHg) was first proposed by the 3rd Report of the Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure in 1984.
However, some researchers, skeptical about these criteria, suggested that cardiovascular mortality could be avoided by lowering the BP down to 120/80 mmHg in both younger and middle-aged groups based on data from a 22-year follow-up cohort. Others also suggested that hypertension should be defined according to age- and sex-specific thresholds rather than a single value. At the same time, one of the most extensive meta-analyses, including 61 cohorts, 958,074 subjects, and 56,000 cardiovascular deaths, also indicated a different optimal blood pressure value, 115/75 mmHg. The results of these critical studies suggested that the definition of normal BP is still controversial.
Another shortcoming of this risk factor definition becomes apparent when we examine the consequences of acting on a test result that falls beyond the normal range. For example, close to 10% of all cancer diagnoses are caused by hereditary susceptibility to breast cancer and ovarian cancer; it is now possible to identify carriers of the two genes more involved in these types of cancer, the BRCA1 and BRCA2 genes. Healthy women who carry the BRCA1 mutation have a lifetime breast cancer risk of 46-87%; for those with the BRCA2 mutation, the risk is 39-84%; both risks are higher than the 13% in women who do not carry the mutations.
Although annual screening with mammography and magnetic resonance imaging promotes the earlier detection of the disease, leading to breast-conservative surgery, for many, the risk of breast cancer in this group of women can be reduced by a bilateral mastectomy. Will altering a risk factor change the risk, or could other risks result from genetic testing? Overall, most studies reported higher levels of distress, anxiety, and depression in mutation carriers compared with non-mutation carriers. These high levels can likely be attributed to an increased risk of future diseases, with implications for the tested individuals and their entire families.
Predictive genetic information about disease susceptibility changes the way people perceive themselves and their families; they are redefined as patients, and people may not want to be reduced to data repositories that are continuously monitored for detailed health information. Distinguishing a disease from a risk factor is not easy, especially when it comes to chronic diseases, which often exist on a spectrum from health to disease. Some conditions previously considered a natural part of aging have been reclassified as diseases. For example, osteoporosis, previously considered a normal part of aging, was officially recognized as a disease by the WHO in 1994. Given the link of osteoporosis with an increased risk of fractures and the devastating impact broken bones can have on the elderly, this seems like a change in definition that is justified. However, many clinicians are critical of this shift.
Defining disease by the need for medical treatment is attractive because, typically, diseases require the attention of medical doctors. However, some conditions cannot be treated and are still considered diseases. On the other hand, doctors also attend to several conditions that are not diseases, such as fitness certification for study or travel. More so, circumcision, body modification or enhancement, and family planning procedures cannot be regarded as diseases but require the attention of a physician. The therapeutic definition of disease sets its limits at the point beyond which specific treatments have been shown to do more good than harm. The therapeutic definition of hypertension, for example, avoids the hazards of labeling clients as diseased unless they are going to be treated.
This definition also requires that clinicians stay up to date with advances in therapeutics and become skilled at distinguishing between therapeutic claims. For example, the therapeutic definition of menopause, a normal part of aging that happens to every woman, which cannot be prevented and typically does not require treatment, has been challenged for decades. Menopausal hormone therapy (HT) prescribing practices have evolved over the last decades, guided by the changing understanding of the treatment’s risks and benefits. Before the Women’s Health Initiative (WHI) trial in 2002, HT was generally accepted as appropriate and safe for the treatment of menopausal symptoms and cardiovascular disease prevention. The unexpected findings of the WHI, which raised concerns about breast cancer and CVD risk in women taking oral conjugated equine estrogens and medroxyprogesterone acetate, led many women to stop taking HT, and many physicians to stop prescribing it.
Subsequent studies showed that the elevated risks identified for coronary heart disease applied mainly to women who started HT a decade past menopause, and 18-year follow-up data showed no difference in cause-specific mortality or all-cause mortality in women treated with HT vs. placebo and indicated favorable trends for all-cause mortality among the younger women treated with CE alone. Furthermore, subsequent randomized controlled trials have demonstrated a favorable safety profile of HT when started early in menopause. Other physiological changes in older age, such as a decline in testosterone levels in men, may not be influenced by disease status. Some prescribers recommend testosterone products in response to low testosterone for cardiovascular health, sexual function, muscle weakness or wasting, mood and behavior, and cognition. So far, though, resistance to recognizing this change as a disease has been strong because testosterone supplementation has not shown consistent benefits for cardiovascular risk, sexual function, mood and behavior, or cognition.
Another definition of disease is based on culturally desirable traits; health is a social value, while disease is undesirable; thus, health is considered desirable. However, it is also impossible to exclusively delineate disease from the point of undesirability. Conditions such as shortness and ugliness cannot be counted as diseases, even though they may not be desirable. In the 19th and early 20th centuries, if a person fell ill, had alcoholism or tuberculosis, or abused a spouse or child, it was a pity, but it was a pity for the person and a sadness for his or her family; it was their business. Over time, however, both the existence of these imperfections and the remedies for them have become public health concerns. Now, the treatment of drug addiction, the prevention of domestic violence, handgun control, and the use of seat belts and helmets are society’s responsibility. Concurrently, however, because the responsibility of healthcare providers. Both healthcare providers and society have a vested interest in certain forms of behavior, previously considered a person’s private business, if the failures of self-care have become, in a sense, crimes against society, as society must bear the consequences of these failures. Furthermore, society now looks to healthcare providers for guidance and education to eliminate behaviors that contribute to disease.
This concept of normality can contribute to what has been termed the “corruption of medicine by morality.” If health, whether physical, mental, or social, is considered the norm, and the lack of health is seen as a personal failure, then illness might be perceived as the result of wrongdoing. The belief follows that by eliminating or preventing this wrongdoing, a person can be restored to normal health, benefiting society. Consequently, individuals are seen as having a societal obligation to avoid “misbehavior,” with illness serving as evidence of such misbehavior. This is most evident in cases of “self-abuse,” such as obesity, alcoholism, smoking, heart disease, intravenous drug use, and HIV infection. However, our interpretation of self-abuse is often influenced by uncertainty and changing social norms.
Could we define disabilities as diseases, or diseases based on the disabilities they cause? Disability is a state of functioning. However, disease frequently leads to many forms of disadvantage. The term “disability” is often used to describe what we now know as intellectual disability. When the International Classification of Diseases-10 was promulgated in 1990, the term “mental retardation” made its inclusion in ICD-10 as a “disorder.” Mental retardation, and preceding terms, referred to defects of mind (e.g., mental deficiency) that resulted in impaired mental performance characterized by mental slowness (e.g., mental retardation), inferior mental performance, and the context in which the person functions, assuming that the disability is a defect within the person. However, we now consider intellectual disability to be the result of interactions between individual capacities and the context in which they function. Intellectual disability is not a condition or a disease; it is a state of functioning.
Sometimes, a disease may reduce an individual’s ability to participate actively in the social network, such as the inability to walk or stand. Pregnancy, for instance, cannot be considered a disease, even though it comes with some limitations. In contrast, several skin diseases may not be classified as diseases since they do not present with disabling effects.
Disease by consensus.
Diagnosis, prognosis, and treatment are closely tied to specific, agreed-upon disease categories in both conceptual and practical applications. Health professionals generally base their diagnosis of physical and mental disorders on disease definitions and diagnostic thresholds drawn up by expert panels and published as statements or as part of clinical practice guidelines. These disease definitions, based on diagnostic criteria, are regularly reviewed and updated in response to changes in disease detection methods, treatments, medical knowledge, and, in the case of mental illness, shifts in cultural norms. Sometimes, the review process widens disease definitions and lowers diagnostic thresholds. Such changes can be beneficial. For example, they might ensure that life-threatening conditions are diagnosed early when they are still treatable. However, the widening of disease definitions can also lead to over-diagnosis—the diagnosis of a condition in a healthy individual that will never cause any symptoms and will not lead to an early death. Over-diagnosis can unnecessarily label people as ill, harm healthy individuals by exposing them to treatments they do not need, and waste resources that could be used elsewhere.
Throughout history, numerous instances have classified certain characteristics as diseases, often rooted in traditional beliefs and views connecting health, disease, and sin. With the emergence of psychology as a science, some behaviors once perceived as “sins” began to be reinterpreted as mental health disorders. A notable example is homosexuality. In 1968, the American Psychiatric Association (APA) classified homosexuality as a mental disorder. This classification was contested in 1973 when APA members voted, with 58% favoring its removal from the diagnostic manual. However, it took another decade for homosexuality to be removed entirely from the manual, and today, it is recognized as a “normal characteristic” within the spectrum of human diversity.
On a global scale, diseases are cataloged by international expert groups in the World Health Organization (WHO). The International Classification of Diseases (ICD) is a diagnostic tool used for epidemiology, health management, and clinical purposes, currently in its tenth revision (ICD-10). Despite its name, the classification extends beyond diseases to encompass related health issues that may be associated with a specific disease, symptom, syndrome, or even a consequence of a medical procedure. For instance, dehydration is classified under the term “volume depletion” in ICD-10. According to the WHO, approximately 70% of global healthcare funding, around $3.5 billion in U.S. dollars, is allocated using the ICD. A survey by the WHO and the International Union of Psychological Science found that 70% of clinicians worldwide use ICD-10 on a daily basis.
In 2013, researchers at Bond University in Australia examined the process of disease classification. They found that expert groups often expand the definitions of common diseases without fully considering the potential risks or implications of increasing the number of people diagnosed with these conditions. They also observed that these experts frequently have conflicts of interest, such as funding from pharmaceutical companies.
Ultimately, what is classified as a disease is primarily determined by expert consensus, even when there is no universal agreement on the definition of “disease.”
Diagnosis: A patient-centered definition of disease
Health providers rarely concern themselves with defining what is a medical disorder; they instead spend their time diagnosing and treating individual patients, and much of their work involves conditions that are generally not considered medical disorders, such as pregnancy or childbirth, or preventive medicine, such as advising mothers of children attending a well-baby clinic or advising middle-aged men regarding diet and exercise. The way disease and illness are conceptualized is crucial because these definitions are key to understanding the limits and scope of responsibility in medical practice.
Defining “disease” is far more complex than it initially appears. The misuse of terms like “syndrome,” “disorder,” and their connection to “diagnosis” is one of the many challenges faced by medical professionals, especially when creating expert systems to aid in diagnoses. Despite the widespread use of the term “disease” in both medical and everyday language, it lacks a clear, universally accepted definition. Yet, many who use the term operate under the illusion that its meaning is commonly understood.
Despite the expanding diagnostic frameworks and taxonomies, modern medicine often overlooks the patient’s lived experience. As one physician noted, the anguish experienced by patients is often overwhelming. Yet modern medicine, enamored with technology and depersonalization, has largely neglected the fundamental human reality of suffering.
Simplistically, a medical condition is something that brings a patient to a healthcare provider. A physical fitness, a medical issue, or an illness. In ailment, a state of fitness, something that is essential to the occurrence of something else (e.g., precondition), an ‘abnormal’ behavior (e.g., frequently also used as a general term for a disease or disorder, and this has fueled heated debates about the concept of disease: Is aging a disease? What about obesity, insomnia, and grief? Labeling medical conditions as “disorders” helps clarify the responsibilities of the medical system in contrast to other societal systems. It also provides a basis for determining which conditions should be included or excluded from medical classifications and guides the distinction between disorders and diseases.
A medical disorder is a relatively distinct condition that arises from an organism’s dysfunction and is directly and intrinsically linked to distress, disability, or various other disadvantages, which may be physical, perceptual, sexual, or interpersonal. This definition implies a need for action by the individual affected, medical professionals, and society as a whole. A mental disorder, specifically, is a type of medical disorder where the primary signs or symptoms are psychological (behavioral) in nature or, if physical, can only be understood through psychological concepts.
Table 1:
| Criteria | Medical | Mental |
|---|---|---|
| A: The condition, in the fully developed or extreme form, in all environments (other than one specially created to compensate for the condition), is directly associated with at least one of the following: | Trigeminal neuralgia | Phobic disorder |
| 1. Distress-acknowledged by the individual or manifested | Pituitary dwarfism | Antisocial personality disorder |
| 2. Disability-some impairment in functioning in a wide range of activities | Color blindness | Manic disorder |
| 3. Disadvantage (not resulting from the above)-certain forms of disadvantage to the individual in interacting with aspects of the physical or social environment because of an identifiable psychological or physical factor. The following forms of disadvantage, even when not associated with distress or disability, are now considered, in our culture, as suggestive of some organismic dysfunction warranting the designation of medical disorder: | Sterility | Alcoholism |
| a. Impaired ability to make critical environmental discriminations | Fused toes, port wine stains | Sexual sadism |
| b. Lack of ability to reproduce | Kleptomania | |
| c. Cosmetically unattractive because of a deviation in kind, rather than degree, from physical structure | Pathological gambling | |
| d. Atypical and inflexible sexual or other impulse-driven behavior, which often has painful consequences | Anorgasmia | |
| e. Impairment in the ability to experience sexual pleasure in an interpersonal context | Narcissistic personality disorder | |
| f. Marked impairment in the ability to form relatively lasting and non-conflictual interpersonal relationships | Hysterical personality disorder |
From symptom to disease: People seek professional help because they feel symptoms. These symptoms are inherently subjective, involving emotions and sensations like anxiety, fear, pain, and suffering. However, as professionals, we access and understand others’ illnesses through their verbal descriptions, shared language, and mental states, aiming to comfort patients, provide care, alleviate suffering, and assess symptoms to form a diagnosis.
Symptoms represent the patient’s complaints; patients typically seek a professional opinion when the symptoms are severe. The patient perceives, for example, subjective pains and discomforts, disturbances of function, or some simple appearance. However, as a skilled observer, the healthcare provider can discern what the patient cannot. Providers can see, palpate, percuss, measure, and compare with notes in the patient’s medical record and order and interpret lab tests and imaging studies.
A symptom is a manifestation of illness that the patient experiences, while a sign is a manifestation of disease observed by the physician. The sign serves as objective evidence of the disease. A syndrome is a recognizable collection of symptoms and physical findings that indicate a specific condition, even when the direct cause is not fully understood. For example, doctors often use the term “syndrome” when there is uncertainty about the numerous viral agents that could be causing the illness. However, once medical science identifies the causative agent or process with a high degree of certainty, the condition is typically referred to as a disease rather than a syndrome.
Diagnosis in the 21st century
Disease is the target of healthcare professionals who classify, detect, control, and treat diseases, ultimately to cure them. The basic disease phenomena are physiological, biochemical, genetic, and mental entities and events that can be observed, examined, mediated, and measured. Accurate, timely, and patient-centered diagnosis still relies on proficiency in clinical reasoning, which is often regarded as the clinician’s quintessential competency.
Clinical reasoning is “the cognitive process necessary to evaluate and manage a patient’s medical problems.” It occurs within clinicians’ minds. It involves judgment under uncertainty, with a consideration of possible diagnoses that might explain symptoms and signs, the harms and benefits of diagnostic testing and treatment for each of those diagnoses, and patient preferences and values. Understanding the clinical reasoning process and the factors that can impact it is essential for improving diagnosis, given that clinical reasoning processes also contribute to diagnostic errors.
Clinical reasoning is traditionally seen as an integration of two separate cognitive systems: the analytic system and the non-analytic system. Clinical problem-solving is an analytical process where experienced clinicians often intuitively arrive at diagnoses based on similarities with previously encountered cases. While many of these diagnostic impressions are correct, they are not always accurate. In clinical practice, accurately identifying a working diagnosis is essential. Thorough questioning about the onset of symptoms is vital for contextualizing physical findings. Diagnostic tests are typically performed to confirm the diagnosis and determine the underlying cause of specific symptoms.
Therefore, diagnostic testing has become indispensable for confirming diagnostic impressions, monitoring disease, providing prognoses, and evaluating treatment responses. More than 40,000 in vitro diagnostic testing products are available for various conditions. These include traditional laboratory-based tests, with samples being sent to a central laboratory for analysis, and point-of-care tests, which can be performed near or at the point of patient care. Point-of-care testing can help optimize treatment decision-making, reduce referrals, enhance the efficiency of care, and lower costs. Tests can also be used for screening. Screening tests are conducted on individuals who do not exhibit symptoms. They aim to detect diseases early before any symptoms become noticeable. They determine whether an asymptomatic individual has an undetected disease or condition. Screening is currently used in many contexts, including blood pressure monitoring for identifying hypertension, prostate-specific antigen measurement for signs of prostate cancer, colonoscopy for detection of colorectal carcinoma, and mammography for evidence of breast cancer. Unfortunately, some screening tests lack credible scientific bases and misrepresent the risks and benefits of testing to the patient.
Innovation can transform healthcare systems and laboratory medicine by providing the knowledge and tools they need to deliver better care to more patients while utilizing fewer resources. Over the years, numerous attempts have been made to mechanize this process and assist practitioners by formulating diagnostic chart flows and automating diagnostic systems, which have been available since the early 1980s. Nevertheless, these efforts have yet to meet expectations, except for some minimal domains.
Artificial intelligence (AI) is revolutionizing diagnostic, disease prevention, and control techniques, significantly enhancing patient safety and treatment quality in specific areas of clinical practice. Notable applications include detecting atrial fibrillation, epilepsy seizures, and hypoglycemia, and diagnosing diseases through histopathological examination and medical imaging. Traditional automated diagnostic methods utilize machine learning algorithms to identify features that healthcare providers manually extract as key information from diagnostic reports. This process is challenging due to the vast amount of medical data involved, leading to ongoing issues with efficiency and accuracy. Laboratories are now using software to automate sample handling and outcome management, improving workflow and resource utilization. For example, rule-based auto-verification systems compare patient outcomes to various factors to validate and speed up reporting or actions. Additionally, advanced systems monitor activities to detect bottlenecks and alert staff to potential issues like delays in STAT samples or reagent expiration dates.
The COVID-19 pandemic accelerated AI and innovation, demonstrating that AI-driven methods significantly impacted infection screening, analysis, prediction, and tracking. During the pandemic, AI played a vital role in managing infectious diseases, reducing time, cost, and human effort while offering efficient and reliable solutions. This has led some to question whether AI could eventually replace healthcare providers.
The integration of artificial intelligence and machine learning (AI/ML) into prevention science has the potential to either mitigate or exacerbate health inequities. Incorporating community engagement throughout the development and implementation of AI/ML models is a crucial strategy for addressing structural biases and enhancing the contextual relevance of these models. Empirical examples from work with Indigenous, Hispanic/Latino, and Native Hawaiian communities illustrate how community-guided approaches can improve the equity and effectiveness of AI/ML applications in public health.
But people are not merely biological entities; we are sentient beings with motives, thoughts, feelings, and relationships. Disease manifests in individuals rather than just their components, due to interactions with informational, social, cultural, and bio-physicochemical environments. Adopting a “biopsychosocial” perspective, which considers the interplay between the individual, the disease, and their social system, is essential for assessing patients’ quality of life. For the time being, this is highly dependent on the provider-patient relationship. The omission of subjects such as empathy, compassion, poverty, and illness, and the limits of medicine from most medical schools and postgraduate curricula, reflects a structural disregard for the psychosocial dimensions of disease.
The provider-patient relationship is a consensual bond in which the patient actively seeks the care of the provider. This fiduciary relationship involves the provider agreeing to respect the patient’s autonomy, maintain confidentiality, explain treatment options, obtain informed consent, deliver the highest standard of care, and ensure that the patient is not abandoned without sufficient time to find a new physician. However, this contractual definition does not fully capture the profound and significant emotional aspects of the relationship; interacting with the doctor is associated with hope, trust, and expectations for improvement, making the encounter feel rewarding. Patients often disclose personal secrets, worries, and fears to their physicians that they may not share with friends or family. Trust in the doctor is crucial for maintaining or regaining health and well-being, highlighting the importance of the provider-patient relationship in fostering a strong placebo effect.
Disease is shaped by social expectations, norms, and policies, which define what constitutes sickness and influence entitlement to treatment, economic rights, and social exemptions. This understanding impacts the provider-patient relationship, as the shared social knowledge of sickness affects how patients are perceived and treated within different cultural and institutional contexts; it is essential to note that, in this sense, disease affects not only the patient but also the treatment of chronic disease and health outcomes also burden providers and caregivers. Provider burnout is an epidemic in the U.S. healthcare system, with nearly 63% of physicians reporting signs of burnout at least once weekly.
Direct healthcare costs represent only a fraction of the true economic burden of disease, often underestimating lost productivity and the toll on providers and caregivers. Beyond its economic impact, how we define disease shapes clinical practice, healthcare policy, and research priorities. A clear, holistic definition is essential to guide medical decision-making and resource allocation. The limitations of current disease definitions demand urgent attention. While there is momentum toward a more comprehensive framework, translating these discussions into practice remains challenging. The current political environment is reshaping public health policy and medical authority, heightening skepticism toward established paradigms, particularly regarding chronic illness, environmental factors, and social determinants of health (SDOH). Ignoring the role of economic stability, education, and healthcare access risks reinforcing narrow biomedical models that fail to capture the broader realities of health.
As ideological divides increasingly shape healthcare decisions, bridging the gap between philosophy and practice is no longer an abstract pursuit but a necessity. If we fail to engage in these critical discussions, we risk allowing political rhetoric to dictate medical reality, with profound consequences for public health, clinical care, and health equity.
Ethics approval and consent to participate:
Not applicable
Consent for publication:
Not applicable
Availability of data and material:
Not applicable
Competing interests:
Not applicable
Funding:
Not applicable
There are no financial interests directly or indirectly related to the work submitted for publication. The authors declare that they have no conflicts of interest.
Authors Contributions:
Dr. Gonzalez-Fisher led the primary research, writing, and synthesis of the manuscript. Dr. Prestridge and Dr. Rissman provided valuable ideas, editorial feedback, and critical revisions that enhanced the intellectual rigor and clarity of the publication. All authors reviewed and approved the final version for submission and agreed to be accountable for all aspects of the work, ensuring that any questions regarding accuracy or integrity are appropriately investigated and resolved.
References:
- Fitzgerald FT. The tyranny of disease. N Engl J Med. 1994;331(3):196-198. doi:10.1056/NEJM199407213310312
- Sartorius N. The meanings of health and its promotion. Croat Med J. 2006;47(4):662-664.
- World Health Organization. Global spending on health: Coping with the pandemic. Geneva, Switzerland: WHO; 2023. Accessed June 27, 2025. https://www.who.int/publications-detail-redirect/9789240086746
- The Guardian. RFK Jr praises beef tallow on Fox News show with burger and fries. The Guardian. March 12, 2025. Accessed March 13, 2025. https://www.theguardian.com/us-news/2025/mar/12/rfk-jr-hannity-interview-beef-tallow
- Laurel SJ. Medicine as a sacred vocation. Proc (Baylor Univ Med Cent). 2018;31(1):126-131. doi:10.1080/08998280.2017.1400318
- Hardy K. Paleomedicine and the evolutionary context of medicinal plant use. Rev Bras Farmacogn. 2021;31(1):1-15. doi:10.1007/s43450-020-00107-4
- Spikins P, Needham A, Tilley L, Hitchens G. Calculated or caring? Neanderthal healthcare in social context. World Archaeol. 2018;50(3):384-403. doi:10.1080/00438243.2018.1433060
- Gonzalez-Fisher R, Flores-Shaw P. El papiro quirúrgico de Edwin Smith. Anales Médicos. 2005;50(1):43-48.
- Patwardhan B, Warude D, Pushpangadan P, Bhatt N. Ayurveda and traditional Chinese medicine: a comparative overview. Evid Based Complement Alternat Med. 2005;2(4):465-473. doi:10.1093/ecam/neh140
- Lagay F. The legacy of humoral medicine. Virtual Mentor. 2002;4(7):206-208. doi:10.1001/virtualmentor.2002.4.7.mhst1-0207
- Karabatos I, Tsagkaris C, Kalachanis K. All roads lead to Rome: aspects of public health in ancient Rome. Le Infez Med. 2021;29(3):488-491. doi:10.53854/liim-2903-21
- Starr, P. (1984). The social transformation of American medicine: the rise of a sovereign profession and the making of a vast industry (Updated). (2017). Basic Books. May 30 2017
- Svalastog AL, Donev D, Jahren Kristoffersen N, Gajović S. Concepts and definitions of health and health-related values in the knowledge landscapes of the digital society. Croat Med J. 2017;58(6):431-435. doi:10.3325/cmj.2017.58.431
- Mellor D. What exactly is a disease? Simple question but complex answer. Times of Malta. July 25, 2019. Accessed September 6, 2023. https://timesofmalta.com/articles/view/what-exactly-is-a-disease-simple-question-but-complex-answer.724471
- Scully JL. What is a disease? EMBO Rep. 2004;5(7):650-653. doi:10.1038/sj.embor.7400195
- Kishan P. Yoga and spirituality in mental health: illness to wellness. Indian J Psychol Med. 2020;42(5):411-420. doi:10.1177/0253717620946995
- Bhattacharya S, Pradhan KB, Bashar MA, Tripathi S, Thiyagarajan A, Srivastava A, Singh A. Salutogenesis: a bona fide guide towards health preservation. J Family Med Prim Care. 2020;9(1):16-19. doi:10.4103/jfmpc.jfmpc_260_19
- Enfermedad: leer a Heráclito. Vanguardia (Saltillo). March 16, 2025. Accessed March 16, 2025. https://vanguardia.com.mx/opinion/en-el-mismo-rio-entramos-y-no-entramos-enfermedad-leer-a-heraclito-CP15295564
- Burrows W, Scarpelli DG. Disease. Encyclopedia Britannica. September 6, 2023. Accessed June 27, 2025. https://www.britannica.com/science/disease
- Catita M, Águas A, Morgado P. Normality in medicine: a critical review. Philos Ethics Humanit Med. 2020;15(1):3. doi:10.1186/s13010-020-00087-2
- Canadian Medical Association. How to read clinical journals: II. To learn about a diagnostic test. Can Med Assoc J. 1981;124(6):703-710.

