Implementing Advanced Practice Nurses in Healthcare Systems
Exploring the Implementation of Advanced Practice Nurses in Healthcare Systems: Factors of Role Identity to Consider with Policy Development
Madrean Schober1, PhD, MSN, ANP, FAANP, FAAN
- President, Schober Global Healthcare Consulting
OPEN ACCESS
PUBLISHED: 30 June 2025
CITATION: Schober, M., 2025. Exploring the Implementation of Advanced Practice Nurses in Healthcare Systems: Factors of Role Identity to Consider with Policy Development. Medical Research Archives, [online] 13(6).
https://doi.org/10.18103/mra.v13i6.6689
COPYRIGHT: © 2025 European Society of Medicine. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
DOI https://doi.org/10.18103/mra.v13i6.6689
ISSN 2375-1924
ABSTRACT
Worldwide, countries are seeking answers to the challenge of meeting increasing demands to improve quality of and access to primary healthcare. An increase in communicable and noncommunicable diseases has stimulated governmental and nongovernmental authorities to seek solutions better suited for the healthcare needs of their populations. Significant gaps in primary healthcare along with fragmented healthcare delivery have caught the attention of governments and healthcare planners globally. The World Health Organization and the International Council of Nurses have identified the potential for nurses, as a resource, to enhance the provision of healthcare services. One proposal is the promotion of advanced practice nurses such as nurse practitioners and clinical nurse specialists. The process of integrating advanced practice nursing into the healthcare workforce and diverse healthcare settings is a dynamic process characterized by constant change, alterations in service delivery and progress toward a new era in nursing practice. The nature of these changes is met with both enthusiasm and skepticism. Challenges to successful implementation of advanced practice nurses include lack of role clarity and opposition or confusion from other healthcare professionals. Preparing for the implementation of advanced practice nurses within healthcare systems globally requires comprehending the advanced practice nurse concept and how health policy impacts their clinical practice. Supportive policy formation shapes and influences effective and sustainable implementation of advanced practice nurses. This article describes characteristics that define advanced practice nursing and identifies policy issues that significantly influence optimal scope of practice and appropriate education for this emerging field of nursing. The provision of advanced education, appropriate legislative and regulatory mechanisms along with anticipatory planning need to come together to guide role implementation. As countries assess the possibility of integrating advanced practice nurses into the healthcare workforce and in order to maximize their contributions, service delivery environments need to ensure that practice regulations are up to date and appropriate for advanced practice nurses.
Keywords:
health policy, scope of practice, advanced practice nursing, education, implementation, primary healthcare, universal healthcare
Introduction
The escalating costs of healthcare, an increased incidence of communicable and noncommunicable diseases along with aging populations have motivated countries worldwide to consider healthcare reform and new approaches toward improving primary healthcare (PHC) in the hope of achieving sustainable and accessible universal healthcare (UHC). In an effort to meet this challenge, the World Health Organization and the International Council of Nurses have identified advanced practice nursing (APN) as a potential resource for enhancing the provision of healthcare services. These factors present an opportunity for advanced practice nurses (APNs) to contribute to strategies that could ease the burden on the provision of PHC services. Acknowledging this perspective calls for a dynamic change in thinking along with implementation of health policies that promote APN clinical practice. Policy processes and decision-making that lead to supportive policy guidelines encourages favorable APN implementation. This includes policies and regulations linked to a professional standard that adopts a clear professional identity, support for optimal clinical scope of practice and appropriate advanced education. Preparing for the implementation of APNs within healthcare systems requires comprehending and appreciating how policy or lack thereof impacts APN practice. This article distinguishes issues of importance to the identity and clinical practice of advanced practice nurses when considering health policy development.
Providing Regulatory and Legislative Guidance
Health policy guidelines and related actions affect institutions, organizations, and healthcare professionals that provide healthcare services as well as funding arrangements of the healthcare system. Therefore, the context in which the term policy is used must be considered in order to identify the intended significance. Health policy helps to clarify priorities; it establishes roles and expectations for different groups, whether physicians, nurses or administrators. The health policy process also helps to build a consensus among the different participants in a community or a health system. Purposeful policy decisions represent a response to an issue that commands authority and impacts practice.
Guidance for APNs is offered as health policy decisions are made in the process of developing and evaluating regulatory systems. Regulations and legislation in turn promote high-quality care by defining the scope and standard of practice, licensure, credentials and educational requirements. Internationally, regulations and legislation for APNs are variable and in many cases either absent or excessively restrictive. When present, policy and resulting regulatory mechanisms identifying title protection, standardized education and competencies have been found to improve role clarity and APN implementation. Conversely, absence of regulation contributes to lack of role clarity and variability in how APNs are integrated into the healthcare workforce. Thus, lack of health policy to acknowledge and guide APN workforce integration can have a negative impact on effective role implementation and sustainability.
In roles across health systems and community settings APNs are well positioned to assess individuals, communities, and populations; advocate for justice and equality; and partner with legislators and interprofessional leaders to identify, implement, and evaluate a strengths-based approach that engages communities. Health policy that influences regulation and legislation determines what nursing professionals can do, how they do it, and what they are paid. This becomes increasingly important as APNs seek to clearly define this category of nursing. Health policies and how they are implemented shape the direction of healthcare delivery. However, too often data and narrative accounts confirm that health policy relevant to APNs such as implementation of legislation, regulation and a professional standard are missing in national initiatives. Practice environments are not always well prepared to welcome APNs. Healthcare decision-makers frequently do not understand the APN concept. APNs are struggling to be recognized, to establish an appropriate practice standard, and to decide on what education is required in order to have their scope of practice legitimized and fully utilized in healthcare systems globally. In order to align APNs as a significant solution to closing the gaps and addressing the challenges in provision of healthcare services worldwide, supportive health policy guidance needs to be implemented for optimal workforce integration.
In countries where there are policies in place, the guidelines and procedures should be reviewed to assess if there is a need for improvement. The field of advanced practice nursing is dynamic and constantly changing. Health policy that was relevant a decade ago might be considered out of date or inadequate in the current healthcare environment.
Discussion
Advanced Practice Nursing Identity: Establishment of a Professional Standard
Advanced practice nurses are skilled in assessing individuals, families and community health needs. Their education prepares them to provide integrated care that includes health promotion and disease management. In order to provide these services health policies supportive of optimal clinical practice need to be considered. Issues that significantly impact APN implementation and recognition of this advanced level of nursing and that require policies are discussed in this section. Throughout this article reference is made to APNs in general, however, it is worth noting that the following categories are considered advanced practice nurses with a clinical focus in most countries:
- Clinical Nurse Specialists (CNS): CNSs provide direct clinical specialty care usually in hospital settings. In addition, they provide consultation and administrative guidance to nursing staff and healthcare systems in the management of complex patient care.
- Nurse Anesthetists (NA): NAs specialize in administering anesthesia and providing pain management for patients before, during, and after surgery, usually in collaboration with surgeons and other healthcare professionals.
- Nurse Practitioners (NP): NPs assess, diagnose, order and interpret laboratory tests and prescribe medications for individuals within a framework of collaboration with other healthcare professionals within health systems primarily focused on PHC.
- Nurse Midwives (NMW): NMWs specialize in women’s health and reproductive care providing a range of services including prenatal care, labor and delivery, and postpartum care. A NMW combines nursing expertise with the midwifery model of care.
In addition, as countries integrate the concept of APNs, there is also a tendency to adopt titles, roles and levels of practice associated with the setting in which they work and the environment of the implementing country.
Title Protection for the Advanced Practice Nurse
Designation of what title to use in reference to the nurse with advanced practice credentials is fundamental when proceeding with an APN initiative in order to reduce confusion when introducing this new professional to the healthcare workforce. A clearly identifiable and legally protected title safeguards the public from unqualified practitioners who have neither the education nor the competencies indicated by the title. The designated title refers to a certain level of confidence with respect to accountability and the healthcare services that this professional can provide. Once there is consensus on a title, the additional policies that guide the APN definition, scope of practice, competencies and professional standard can be developed relevant to the title. A representative and legally protected title is the quickest method to communicate to other healthcare professionals, managers, administrators, clinical staff and the public who these healthcare professionals are and what services they provide.
Absence of a legally protected title leads to lack of role clarity and confusion when seeking to proceed with implementation of APNs. This poses a major barrier to role integration for a recognizable clinical position that effectively integrates APNs into the healthcare workforce.
Scope of Practice for Advanced Practice Nurses
A defined APN scope of practice describes the range of activities related to recognized professional responsibilities that are consistent with boundaries imposed by regulations relevant to the context and setting in which the APN practices. APN scope of practice statements define what an APN can do, what population can be seen or treated and under what circumstances the APN can provide care. The scope of practice provides guidance and direction to other healthcare professionals, educators, regulatory authorities and the public. Once defined, the scope of practice and associated competencies are linked to a designated title and form the foundation for developing APN education and curricula.
In addition, an established APN scope of practice is one way of informing the public, administrators, and other healthcare professionals about the role in order to differentiate the qualified APN from other nurses who do not have the qualifications to be identified as an APN or have not been authorized to practice in this capacity. Specifying an APN scope of practice also assists government agencies, healthcare planners and healthcare institutions with workforce planning that integrates the APN for optimal clinical practice.
An APN scope of practice could originate from a professional association or organization as a health policy guideline or from a regulatory body as a legal requirement. In defining a scope of practice for the APN, challenges arise when there is resistance to progress beyond the generic nursing definition when developing a standard that emphasizes the advanced level of knowledge, competencies, clinical judgement and decision making that APNs bring to their practice setting.
Prescriptive Authority for Advanced Practice Nurses
Prescriptive authority is an issue that fuels animated debate when seeking policy that supports this feature of APN practice. The discussion focuses on the changes in the boundaries of nursing practice and the impact this change has on other healthcare professions, usually a concern that it will impinge on the professional role of physicians.
The degree of authority and the type of limitations placed on APN prescribing varies across jurisdictions. Approaches to APN prescriptive authority are mirrored in the wider debate on the APN concept and level of practice, and reflects the confusion that surrounds APN evolution, definition and regulation worldwide. Establishment of policies and legal authority for APN prescribing may lag behind the reality of actual clinical practice. If advancement in nursing is to take place, defined prescriptive authority is a requisite for optimal clinical practice. Consistency in criteria and education for APN prescribing in turn enhances the credibility for APN scope of practice. This requires clear health policy guidelines and regulation.
Education Criteria for Advanced Practice Nursing
Education criteria for the APN provide the basis for establishing credibility for the advancement of this nursing role and level of practice. The current international requirement is a minimum of a master’s degree. However, variations exist in entry requirements for participants in APN education programs and the availability of appropriate programs. The integrity of APN for the future will rely on consistency for entry level criteria that a nurse must have to begin a specifically designated APN program. Education recommendations require that curricula content must be specific and appropriate to the defined category of APN and associated APN scope of practice.
When a consistent standard for APN education is lacking the issue of lack of role clarity and acceptance in the healthcare workforce continues to be questioned. This variability and inconsistency put at risk the future of quality care and contributions to healthcare systems provided by APN expertise. APN development and implementation benefits from the foundation of a consistent and aligned education pathway.
Credentialing the Advanced Practice Nurse: Certification / Endorsement / Licensure / Registration
Policy decisions guide or determine APN credentialing. Credentialing processes and procedures refer to the mechanisms that officially regulate and define APN practice. This can include but is not limited to, the assignment of degrees, authorization, endorsement, certification, licensure, accreditation and registration. The methods and processes are connected to a country’s regulatory traditions and agency resources in addition to what level is determined to be necessary to authorize a nurse to work within a scope of practice for an APN but beyond the scope of practice for a generalist nurse.
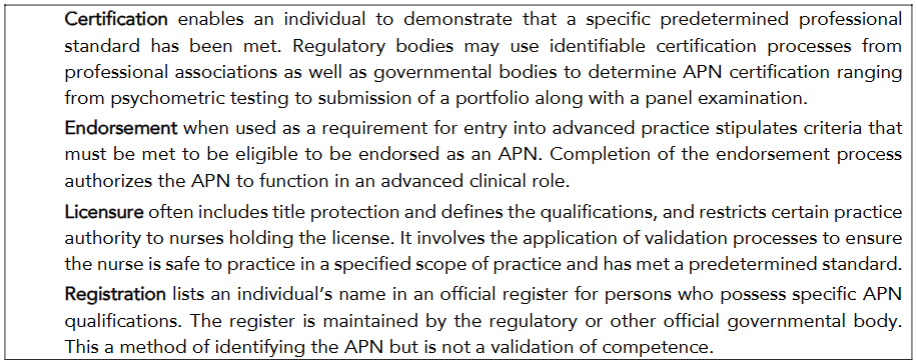
Credentialing can be considered mandatory or voluntary based on the established professional standard and requirements for the APN in the country and/or region where the APN practices. Whichever process is selected, identifying a process of credentialing, along with establishing a professional standard is essential in supporting the legitimacy of APNs within healthcare systems and the healthcare workforce. APN role development involves a transformation in the role identity of the nurse. Even though a credentialing process is viewed as fundamental; it is worth noting that an overly restrictive credentialing process can impede the optimal nature of APN practice.
Health Policy and the Future for Advanced Practice Nurses in Healthcare Systems
Health policy will continue to drive consumer’s decisions, healthcare funding, research and identification of professionals in the healthcare workforce. If APNs are considered to be an option in provision of healthcare services for the future, policymakers and healthcare professionals must be involved in developing supportive health policy. Skilled leadership and evidence informed decisions will be required. Advocating for change requires an understanding of how policy impacts APN implementation. APNs in the future must themselves continue to influence health policy and actively guide development in order to respond to opposition, overcome barriers and ensure that their scope of practice is expanded across all healthcare settings.
Country Issues That Shape Advanced Practice Nurse Development and Implementation
International enthusiasm for the APN concept continues to increase. However, it is important to recognize that the country and regional context in which the APN will practice influences development and implementation. Clinical practice for the APN requires sensitivity to the nursing, medical and societal cultures of the populations they will take care of. The professional status of nurses and their ability to introduce a new category of clinical practice will influence the ability to successfully initiate an APN scheme. The maturity of nursing in the country can be assessed by the level of education for nurses, the presence of other nursing specialties, existing policies specific to nurses (i.e. a nurse practice act) and the extent of nursing research.
Conclusion
Understanding the significance of how health policy impacts components of APN clinical practice is fundamental for the successful implementation of APNs. The rapid proliferation of technology and complex global healthcare needs mandates comprehension of the effect of health policy decisions and their relevance to APN development. This article describes the importance of this knowledge and identifies the issues that require informed health policy decision-making. A case has been made for the necessity to establish health policies that promote legislation and regulations supportive of APNs. However, the barriers and challenges require knowledgeable and skilled policymakers, health professionals and APNs to collaborate in establishing and promoting sound health policies. Integration of APNs in the healthcare workforce is a powerful strategy that addresses global health challenges in seeking to achieve universal healthcare. The path forward requires an evidence informed approach to identify hurdles to implementation while fostering supportive policy environments. Promoting the expertise of APNs underscores the aim to improve health outcomes and build responsive healthcare systems by increasing access to quality healthcare services.
Conflict of Interest Statement:
None.
Funding Statement:
None.
Acknowledgements:
None.
References:
- World Health Organization European Region. Technical brief on strengthening the nursing and midwifery workforce to improve health outcomes. What is known about advancing roles for nurses: evidence and lessons for implementation. Copenhagen, WHO Regional Office for Europe, 2023.
- World Health Organization. State of the worlds nursing 2025: investing in education, jobs, leadership and service delivery. Geneva, World Health Organization, 2025.
- International Council of Nurses. Nursing and primary health care. Towards the realization of universal health care. A discussion paper. Geneva, 2024.
- Barton D, East L. The evolution of advanced nursing practice. In: Barton DT, Allan D, eds. Advanced nursing practice: Changing in a changing world. Palgrave Macmillan; 2015: 1-20.
- Bryant-Lukosius D, Wong FKY. International development of advanced practice nursing. In: Tracy MF, O’Grady ET, eds. Advanced practice nursing: An integrative approach, 6th ed. Elsevier; 2019: 129-141.
- Harris JL. Turning health policy into practice. In: Goudreau KA, Smolenski MC eds. Health policy and advanced practice nursing, 3rd ed. Springer Publishing Company LLC; 2023: 3-11.
- Maier C, Aiken L, Busse R. Nurses in advanced roles in primary care: Policy levers for implementation. OECD Health Working Paper no. 98, 2017. https://doi.org/10.1002/14651858.CDOO1271.pub3
- Rosa WE, Fitzgerald M, Davis S, Khanyola J, Kwong J, Moreland PJ, Rogers M, Sibanda B, Turale S. Leveraging nurse practitioner capacities to achieve global health for all: COVID-19 and beyond, INR 2020; 67(4): 554-559. https://doi.org/10.1111/inr.12632
- World Health Organization. State of the world’s nursing 2020: Investing in education, jobs and leadership. World Health Organization; World Health Organization 2020.
- World Health Organization. Global strategic directives for nursing and midwifery 2021-2025. World Health Organization; 2021.
- McGee P. Influences on the development of advanced nursing practice in the UK. In: McGee P, Inman C, eds. Advanced practice in healthcare: Dynamic developments in nursing and allied health professions. 4th ed. Wiley Blackwell; 2019: 65-84.
- Porche DJ. Health policy: application for nurses and other healthcare professionals. Sudbury. Jones & Bartlett Learning; 2012.
- Milstead JA. Health policy and politics: a nurse’s guide, 4th ed. Jones and Bartlett; 2013.
- International Council of Nurses. Nursing regulation. https://www.icn.ch/sites/default/files/2023-04/B04_Nsg_Regulation.pd. 2013.
- Chappell KB, Howard MS, Lundmark V, Ivory C. Credentialing and certification: Overview, science and impact on policy regulation and practice. INR 2021; 68(4):551-556. https://doi.org/10.1111/inr.12721
- Wheeler, KJ, Miller M, Pulcini J, Gray D, Ladd E, Ravens MK. Advanced practice nursing roles, regulation, education and practice: A global study. Ann Glob Health 2022; 88(1). https://doi:10.5334/aogh.3698
- De Raeve P, Davidson PM, Bergs J, Patch M, Jack SM, Castro-Ayala A, Xyrichis A, Preston W. Advanced practice nursing in Europe-Results from a pan-European survey of 35 countries, JAN 2023: 00, 1-10. https://doi.org/10.1111/jan.15775
- Schober M. Strategic planning for advanced nursing practice. Springer Nature; 2017.
- Pulcini J, Jelic M, Gul, Loke AY. An international survey on advanced practice nursing education, practice and regulation. J Nurs Scholarsh 2010; 42(1):31-39. https://doi:10.1111/j.1547-5069.2009.01322
- Schober M. Introduction to advanced nursing practice: An international focus. Springer Nature; 2016.
- Donald F, Bryant-Lukosius D, Martin-Misener R, Kaasalainen S, Kilpatrick K, Carter N, Harbman P, Bourgeault I, DiCenso A. Clinical nurse specialists and nurse practitioners: title confusion and lack of role clarity. Can J Nurs Leadersh 2010; 23 (Special Issue):189-210. https://doi:10.12927/cjnl.2010.22276
- Hanson CM, Cahill M. Understanding regulatory, legal and credentialing requirements. In: Tracy MF, O’Grady ET, eds. Advanced practice nursing: An integrative approach, 6th Edition, 2019: 563-584.

