Outcomes of Photodynamic Bone Stabilization in Humerus Fractures
Device-related clinical outcomes of the Photodynamic Bone Stabilization System in the treatment of pathologic humerus fractures: A Meta-Analysis of The Literature
Humaid Al Farii, MD 1, Grant McChesney, MD 2, Shalin S. Patel, MD 2, Robert Satcher, MD 2, Spencer Frink, MD 2, Bryan Moon, MD 2, Patrick Lin, MD 2, Valerae Lewis, MD 2, Justin E. Bird, MD 2
- Sultan Qaboos University Hospital, Department of Surgery, Oman.
- Anderson Cancer Center, Department of Orthopedic Oncology, Houston, TX
OPEN ACCESS
PUBLISHED: 31 January 2025
CITATION: Al Farii, H., McChesney, G., et al., 2025. Device-related clinical outcomes of the Photodynamic Bone Stabilization System in the treatment of pathologic humerus fractures: A Meta-Analysis of The Literature. Medical Research Archives, [online] 13(1). https://doi.org/10.18103/mra.v13i1.6255
COPYRIGHT: © 2025 European Society of Medicine. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
DOI: https://doi.org/10.18103/mra.v13i1.6255
ISSN 2375-1924
Abstract
Objectives: The humerus is one of the most common sites of metastatic disease to bone. Over the past decade, however, a novel, non-metallic Photodynamic Bone Stabilization System (PBSS) has become available, creating growing interest in the use of the system to treat pathologic fractures. We aimed to analyze device-related clinical outcomes extracted from a meta-analysis of the literature to determine appropriate use cases in the treatment of pathologic humerus lesions.
Methods: Using predetermined inclusion and exclusion criteria, Pubmed, Medline and Embase electronic databases were searched in January 2023 for relevant articles relating to IlluminOss implants for humerus pathologic fracture. Keywords used were “IlluminOss” OR “Photodynamic Bone Stabilization System” AND “Fracture”.
Results: 114 articles were identified and screened. A total of 67 humerus lesions stabilized with IlluminOss from 5 studies were included for review. 36 (54%) of these patients were female. There were 51 complete pathological fractures and 16 impending fractures. Sixteen of 67 (24%) patients had implant-related complications, including broken implants (13), traumatic periprosthetic fracture (1), proximal migration of implant (1), and intra-articular penetration by a supplemental screw (1). All complications occurred in the setting of complete pathological fractures (P value = 0.01). The distal humerus was the most common location (60%) for complications (P value = 0.02). Complications trended to occur more frequently in females (75%) and patients with renal cell carcinoma (33%), however, these factors were not statistically significant.
Conclusions: The IlluminOss implant has been successfully used to treat many pathological humerus fractures, however, the rate of implant-related complications was high in complete pathologic fractures located in the distal humerus. The most common mode of failure was broken implant. Orthopedic surgeons should consider complete pathologic fractures in the distal humerus as high risk for implant failure and may need to augment their stabilization or choose alternative means of treatment.
Keywords: IlluminOss, Photodynamic Bone Stabilization System, Humerus, Pathological Fracture
Introduction
Bone metastases are commonly associated with severe pain, morbidity, and poor quality of life. The humerus is one of the most common sites for metastatic bone diseases, after the spine and femur. Eighty percent of skeletal metastases originate from prostate, breast, lung, renal or thyroid cancers. Most patients who have a pathologic humerus fracture benefit from surgical intervention. Surgery minimizes pain, allows for early range of motion, and can improve functional abilities and performance status. The two most prevalent fixation methods for non-articular pathologic humerus fractures are intramedullary nail or plate fixation.
Although traditional metallic implants have produced reasonably acceptable clinical outcomes, there are still treatment failures, complications, challenging surgical approaches, and limitations on future imaging and radiation treatments due to the impact of metallic artifacts. Over the past decade, these concerns led to development of radiolucent implants that can be placed using minimally invasive techniques. The IlluminOss Photodynamic Bone Stabilization System (PBSS; IlluminOss Medical Inc), was cleared by Food and Drug Association (FDA) in 2018. It employs a light-curable polymer contained within an inflatable balloon catheter, that allows for additional fracture manipulation to achieve proper fracture reduction prior to hardening the polymer.
While numerous features of the IlluminOss system make it an attractive stabilization option, there are relatively few studies reporting device-specific clinical outcomes in pathological fractures. Therefore, we performed a systematic review of the literature in order to understand the device-related clinical outcomes, potential complications, and risk factors for device failure in the treatment of pathologic humerus lesions.
Methods
SEARCH STRATEGY
The research question and inclusion/exclusion criteria for individual studies were established prior to searching the databases. Online databases (PubMed, Medline and Embase) were used to find literature related to the use of the IlluminOss implant in the treatment of pathologic humerus fractures. Keywords used were “IlluminOss” OR “Photodynamic Bone Stabilization System” AND “Fracture”. Searches were conducted in January 2023 yielding a total of 114 articles from all databases, without any restriction on language or date of publication.
| All Databases (PubMed, Medline & Embase) | Total articles |
|---|---|
| “Photodynamic Bone Stabilization System” [All Fields] | 43 |
| “IlluminOss” [All Fields] | 132 |
| “Fracture” [All Fields] | 1550860 |
| Total “1” OR “2”, AND “3” | 114 |
INCLUSION AND EXCLUSION
We included all pathologic humerus fractures surgically treated using IlluminOss implants irrespective of whether the fractures were complete or impending. The following exclusion criteria were used (1) Non humerus, (2) Non pathological fractures, (3) Animal studies, and (4) Studies classified as technique articles, cadaveric studies, or review articles.
STUDY SELECTION
Combined results of all searches produced 114 articles. In the first review stage, titles and abstracts were screened. Full articles were reviewed if abstracts were consistent with inclusion study criteria. Eight studies satisfied all inclusion and exclusion criteria. An independent reviewer performed full-text review of the eligible studies and an additional three studies were excluded. The final number of pathological humerus lesions was 67 humeri from 5 studies.

DATA ABSTRACTION
One reviewer (H.F) retrieved relevant study data from the final pool of included studies and recorded them on a spreadsheet and IBM SPSS Statistics (version 28). These included study and publication information (author, year of publication, study design, level of evidence, and sample size), patient and disease data (age, sex, primary pathology, medical and radiation treatments), surgical details (procedures performed, technique, and implants), complications, mode of implant failure and follow-up.
Results
A total of 67 pathologic humerus fractures treated using IlluminOss implants from 5 studies were included. Thirty-six patients were female (54%). The mean age was 64 years (range 41-80 years). The average follow up was 14 months (range 2-60 months).
| Article | Humeri (No.) | Age (mean) | Sex | Location | Fx. Imp. | Pathology | Add. Fixation | F/u (Mon.) | Failure | Revision |
|---|---|---|---|---|---|---|---|---|---|---|
| Hoellwarth et al. 2020 | 19 | 63.7 | 11 F, 8 M | 14 Prox., 4 Shaft, 1 Distal | 18 Fx, 1 Imp | 3MM, 3RCC, 8 Breast, 2 Lung, 1 Mela., 1 Prost., 1 HCC | 2 Screws | 16 | 3 Broken implants, 1 Arthroplasty, 1 Resection Arthroplasty, 1 Refused | |
| Albertini et al. 2020 | 2 | 60 | 2 F | 2 Shaft | 2 Fx | 2 RCC | None | 6 | None | None |
| Krumme et al. 2021 | 27 | 63.3 | 15 F, 10 M | 2 NR, 4 Prox., 1 4Shaft, 9 Distal | 18 Fx, 9 Imp | 10MM, 6RCC, 4 Breast, 4 Lung, 2 Mela., 1 Cholang., 1 Lymph. | 4 Screws, 1 Plate | 8.4 | 8 Broken implants, 1 Peripros. Fx, 1 IA screw, 4 ORIF, 1 Screw removal | |
| Zoccali et al. 2021 | 13 | 63.3 | 5 F, 8 M | 13 Shaft | 9 Fx, 4 Imp | 6MM, 1RCC, 2 Breast, 3 Lung, 1 Gastric | 5 Screws | 21.9 | 2 Broken implants, 1 Nail migration, 2 ORIF, 1 Cutting migrated part | |
| Perisano et al. 2022 | 6 | 72.2 | 3 F, 3 M | 6 Prox. | 4 Fx, 2 Imp | 3MM, 3RCC | None | 18.2 | None | None |
From this data, the most common pathology was multiple myeloma (33%) followed by renal cell carcinoma (22%), breast cancer (21%), lung cancer (13%), and melanoma (4%). Singular cases of prostate cancer, hepatocellular carcinoma, cholangiocarcinoma, gastric cancer, and lymphoma were identified. Of note, there was one patient who had diagnoses of both renal cell carcinoma and lung carcinoma; however, the underlying pathology specifically related to the humerus lesion was not determined.
Complete pathological fractures were present in 51 humeri (76%) and impending fractures in 16 humeri (24%). The humeral shaft was the most common location (33 humeri, 49%), followed by the proximal humerus (24 humeri, 36%), and then the distal humerus (10 humeri, 15%). In terms of additional fixation, 11 cases included supplemental fixation in the form of derotational screws and one had plate fixation. There were 17 cases in which supplemental fixation could not be determined. Thirty-eight cases clearly used IllumiOss implants alone. Sixteen device-related failures (24%) were identified, and the most common cause of failure was breakage of the implant (13/16 cases). Failure mode of the three remaining cases included one proximal nail migration, one case in which a supplemental screw was found to penetrate the articular surface of the joint, and one traumatic periprosthetic fracture. All device failures occurred in the treatment of complete fractures compared to no failures in the treatment of impending fractures (P value = 0.01 and confidence interval (CI) 0.08-0.52). Complications also trended to occur in females (12 cases, 75%) (P value = 0.2, CI -0.38-0.09), and within first year from surgery (mean 9 months).
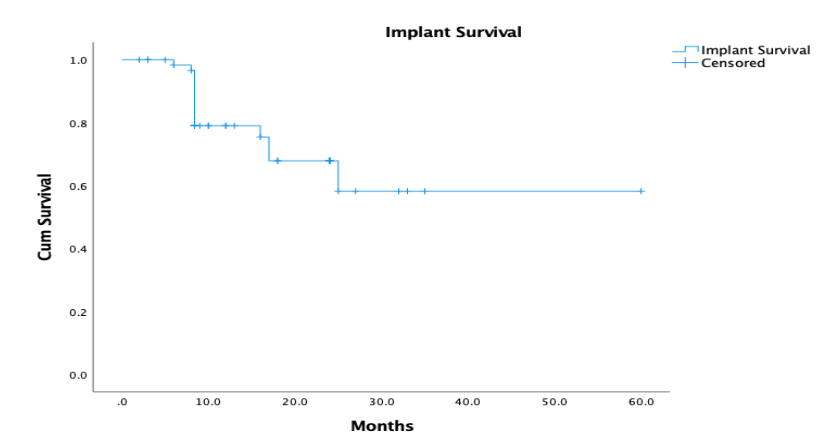
Five device failures occurred in humeri with renal cell carcinoma metastases, followed by 4 with multiple myeloma, 3 with lung carcinoma, 2 with breast carcinoma, 1 with melanoma, and 1 with cholangiocarcinoma. Regarding the location, 4 failures occurred in the proximal humerus, 6 in humeral shaft and 6 in distal humerus. Subgroup analysis revealed that device complications occurred most commonly in the renal cell carcinoma cohort (5/15; 33%) although this was not statistically significant (P value = 0.74, CI -.28- 0.20). Location was a significant factor however, and the distal humerus had the highest rate of device failure (6 /10 distal humeri; 60%), (P value = 0.02, CI -0.48- -0.04). Although 13 cases reported broken implants, only 7 cases reported surgical revisions. Five cases reported performing ORIF, one reported shoulder hemiarthroplasty and one resection arthroplasty. Of the remaining 3 device-related failures, the periprosthetic traumatic fracture was treated with ORIF, the prominent IlluminOss implant was surgically trimmed, and the malpositioned intra-articular screw was removed.
Discussion
Photodynamic Bone Stabilization is a novel technology with promising results in many use cases. The European Union Registry reported initial procedural success among 149 fractures in 2017, preceding FDA clearance in 2018. The benefits of the IlluminOss PBSS include minimally invasive insertion techniques, non-metallic implants, and the ability to place the device in irregular shaped bones that are typically not amenable to traditional intramedullary rods or plates. As interest grows and use cases expand, it becomes extremely important to analyze the outcome data generated in order to determine appropriate use cases, device-related clinical outcomes, and risk profiles. These data driven insights may then be used to guide surgeons who seek to improve patient outcomes by implementing this promising technology in the most appropriate ways.
In our systematic review of 67 pathologic humerus fractures treated with the IlluminOss system, we identified a 24% device-related complication rate, with the most common mode of device failure being implant breakage. Surprisingly, only 50% of the cases with broken implants went on to have a second surgery. Unfortunately, we were unable to further analyse those patients who underwent additional management due to the limitations inherent to literature reviews.
Although pathologic fractures were not included in the Vegt et al. study, the overall complication rate of IlluminOss was a reported 35%, which was not higher than what was reported in the literature for other stabilization devices. Through a subgroup analysis, we identified four factors that could lead to device failures. All device-related complications occurred when the IlluminOss system was used to treat complete pathological fractures and the distal humerus had the highest rate of device failure (60%). Failures more commonly occurred in females (75%), and in patients with renal cell carcinoma (33%).
Eleven cases reported placing supplemental derotational screws and one case reported supplemental plate fixation. Seven cases with supplemental fixation (58%) were among the failures and this was statistically significant (P value = 0.001, CI 0.16-0.57). We did not have enough detailed information to comment more on the utility of supplemental fixation (screws versus plate and screws).
This review has a number of limitations. Given the retrospective nature of the papers in our analysis, there was significant variability in the methodology and non-uniformity in the data reported. For these reasons, we were unable to analyze radiographic parameters, implant size or selection, or other medical complications such as cardiopulmonary events, thromboembolism or wound-related complications.
In conclusion, the IlluminOss Photodynamic Bone Stabilization System is a promising system for the treatment of pathologic humerus lesions and particularly successful when used to stabilize impeding fractures. Device-related complications were highest when used to treat complete fractures in the distal humerus. Implant breakage was the most common mode of device failure. Large lytic lesions with complete fractures are particularly challenging to stabilize by any means, therefore, as with any device, proper patient selection is key. Surgeons should be aware of the limitations of these devices and choose implants carefully. While our analysis provides some insight on the use of the IlluminOss PBSS for pathologic humerus fractures, future well-designed studies are necessary to evaluate and compare IlluminOss with other traditional implants to identify optimal surgical protocols.
COI: No conflicts of interest are declared by any author on this study.
Funding: No funding required for this study.
Ethical approval: Not required for this study.
Informed consent: Not required.
Acknowledgments: Nothing to disclose.
References
- Frassica FJ, Frassica DA. Evaluation and treatment of metastases to the humerus. Clin Orthop Relat Res. 2003;(415):S212-S218.
- Zimel MN, Hwang S, Riedel ER, et al. Carbon fiber intramedullary nails reduce artifact in postoperative advanced imaging. Skeletal Radiol. 2015;44(9):1317-1325. doi:10.1007/s00256-015-2140-x
- Zoccali C, Soriani A, Rossi B, et al. The Carbofix™ “Piccolo Proximal femur nail”: A new perspective for treating proximal femur lesion. A technique report. J Orthop. 2016;13(4):343-346. doi:10.1016/j.jor.2016.08.012
- Coleman RE. Metastatic bone disease: clinical features, pathophysiology and treatment strategies. Cancer Treat Rev.2001;27(3):165-176. doi:10.1053/ctrv.2000.0210
- Saad F, Lipton A, Cook R, et al. Pathologic fractures correlate with reduced survival in patients with malignant bone disease. Cancer. 2007;110(8):1860-1867. doi:10.1002/cncr.22918
- Wedin R, Hansen BH, Laitinen M, et al. Complications and survival after surgical treatment of 214 metastatic lesions of the humerus. J Shoulder Elbow Surg. 2012;21(8):1049-1055. doi:10.1016/j.jse.2011.06.002
- Weiss KR, Bhumbra R, Biau DJ, et al. Fixation of pathological humeral fractures by the cemented plate technique. J Bone Joint Surg Am. 2011;93(12):1093-1097. doi:10.2106/JBJS.J.01032
- IlluminOss Medical. IlluminOss Medical granted FDA marketing clearance for the IlluminOss® bone stabilization system. GlobeNewswire News. Published January 9, 2018. Accessed March 15, 2024. http://www.globenewswire.com/news-release/2018/01/09/1286073/0/en/IlluminOss-Medical-Granted-FDA-Marketing-Clearance-for-the-IlluminOss-Bone-Stabilization-System.html
- Vegt P, Muir JM, Block JE. Photodynamic bone stabilization system: A minimally invasive, percutaneous intramedullary polymeric osteosynthesis for simple and complex long bone fractures. Med Devices (Auckl). 2014;7:453-461. doi:10.2147/MDER.S67681
- Hoellwarth JS, Weiss K, Goodman M, et al. Evaluating the reoperation rate and hardware durability of three stabilizing implants for 105 malignant pathologic humerus fractures. Injury. 2020;51(4):947-954. doi:10.1016/j.injury.2020.01.030
- Albertini U, Conti A, Ratto N, et al. Electrochemotherapy and simultaneous photodynamic bone stabilization of upper limbs in metastatic renal cancer disease: Case report and literature review. Case Rep Med. 2020;2020:8408943. doi:10.1155/2020/8408943
- Krumme J, MacConnell A, Wallace M, et al. Early experience in pathologic humerus fracture treated with the photodynamic bone stabilization system shows limitations related to patient selection. Orthopedics. 2021;44(3):154-159. doi:10.3928/01477447-20210427-03
- Zoccali C, Attala D, Pugliese M, et al. The IlluminOss® photodynamic bone stabilization system for pathological osteolyses and fractures of the humerus: Indications, advantages, and limits in a series of 12 patients at 24 months of minimum follow-up. BMC Musculoskelet Disord. 2021;22(1):63. doi:10.1186/s12891-021-03957-1
- Perisano C, Greco T, Fulchignoni C, et al. The IlluminOss® system: A solution in elderly patients with upper limbs bone metastases. Eur Rev Med Pharmacol Sci. 2022;26(1 Suppl):119-126. doi:10.26355/eurrev_202201_27517
- Gausepohl T, Pennig D, Heck S, et al. Effective management of bone fractures with the Illuminoss photodynamic bone stabilization system: Initial clinical experience from the European Union registry. Orthop Rev (Pavia). 2017;9(1):6988. doi:10.4081/or.2017.6988

