Minimally Invasive Osteosynthesis for Distal Humerus Fracture
Minimally invasive osteosynthesis of distal humerus fracture with commercially available pre-contoured plate using an anterolateral fixation: mid to long-term results
Oscar Alejandro Mejía, M.D1., Jaime Valencia MD2, Carlos Eduardo Afanador, M.D2., Sebastián Calle Díaz, M.D3., Germán Alejandro Jaramillo, M.D4., Ana Milena Herrera, M.D., Ph.D5.
- Orthopedic surgeon. Shoulder and elbow orthopedics. Clínica del Campestre and Clínica Universitaria Bolivariana. Medellín. Colombia
- Orthopedic surgeon. Shoulder and elbow orthopedics. Hospital Pablo Tobón Uribe, Clínica Universitaria Bolivariana and Clínica del Campestre. Medellín. Colombia
- Orthopedic surgery resident. Facultad de Medicina, Universidad de Antioquia. Medellín. Colombia
- Orthopedic surgeon. Shoulder and elbow orthopedics. Clínica del Campestre and Clínica del Norte. Medellín. Colombia
- Epidemiology Unit, Clínica del Campestre. Medellin, Colombia
OPEN ACCESS
PUBLISHED:31 March 2025
CITATION: MEJÍA, Oscar Alejandro et al. Minimally invasive osteosynthesis of distal humerus fracture with commercially available pre-contoured plate using an anterolateral fixation: mid to long-term results. Medical Research Archives, Available at: <https://esmed.org/MRA/mra/article/view/6425>.
COPYRIGHT: © 2025 European Society of Medicine. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
DOI: https://doi.org/10.18103/mra.v13i3.6425
ISSN 2375-1924
ABSTRACT
Background: Treatment of distal humeral fractures (DHF) presents a challenge in orthopedic surgery owing to the complex elbow anatomy and proximity of neurovascular structures. These fractures have a bimodal distribution, mainly caused by high-energy traumas in the young population and by low-energy traumas or falls in older people. Restoration of elbow function and a stable fixation of all bone fragments is critical in managing DHF. Although there is no consensus on the best alternative for surgical treatment, for a while, open reduction and internal fixation (ORIF) with dual plates has been the treatment of choice, especially for more distal metaphyseal fractures.
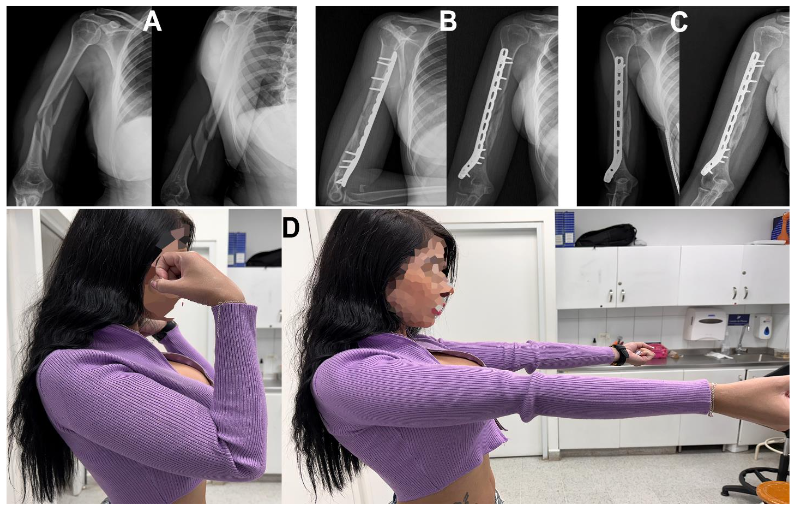
Methods: A retrospective study was conducted from March 2019 to June 2020. All procedures were carried out in Clínica del Especialista and Clínica Universitaria Bolivariana in Colombia. Adult patients (≥ 18 years) were eligible for the procedure if presented with an extrarticular type 12A to 12C DHF. Patients with less than 12 months of follow-up were excluded from the study. After the procedure, all patients were scheduled for routine follow-ups at 3 and 6 months, according to our clinical protocol. Clinical evaluations during follow-ups consisted of the range of motion (AROM) and functional scores, including the Mayo Elbow Performance Score (MEPS), and the presence of pain and complications.
Results: The cohort included six males and four females with a median age of 28.5 years (range 19 – 61 years) at the time of the procedure. Seven patients presented with an intra-articular fracture, and one patient required removal of the osteosynthesis material due to pain with elbow flexion. All patients reported being satisfied with the functional outcome of the surgery.
Conclusion: For meta-diaphyseal and distal diaphyseal extra-articular humerus fractures, a MIPO technique with an anterior approach and anterolateral fixation provided a stable reduction and fixation with satisfactory mid-to-long term results.
Keywords
distal humerus fracture, minimally invasive osteosynthesis, anterolateral fixation, MIPO technique, clinical outcomes
INTRODUCTION
Treatment of distal humeral fractures (DHF) presents a challenge in orthopedic surgery owing to the complex elbow anatomy and proximity of neurovascular structures. These fractures have a bimodal distribution, mainly caused by high-energy traumas in the young population and by low-energy traumas or falls in older people. Restoration of elbow function and a stable fixation of all bone fragments is critical in managing DHF. Although there is no consensus on the best alternative for surgical treatment, for a while, open reduction and internal fixation (ORIF) with dual plates has been the treatment of choice, especially for more distal metaphyseal fractures.
METHODS
A retrospective study was conducted from March 2019 to June 2020. All procedures were carried out in Clínica del Especialista and Clínica Universitaria Bolivariana in Colombia. Adult patients (≥ 18 years) were eligible for the procedure if presented with an extrarticular type 12A to 12C DHF. Patients with less than 12 months of follow-up were excluded from the study.
After the procedure, all patients were scheduled for routine follow-ups at 3 and 6 months, according to our clinical protocol. Clinical evaluations during follow-ups consisted of the range of motion (AROM) and functional scores, including the Mayo Elbow Performance Score (MEPS), and the presence of pain and complications.
RESULTS
The cohort included six males and four females with a median age of 28.5 years (range 19 – 61 years) at the time of the procedure. Seven patients presented with an intra-articular fracture, and one patient required removal of the osteosynthesis material due to pain with elbow flexion. All patients reported being satisfied with the functional outcome of the surgery.
Statistical analysis was performed using SPSS statistical software (version 25.0; IBM Corp, Armonk, NY, USA). The last follow-up was carried out in a median of 36.9 months (95% CI: 32.5-42.5 months). During the last follow-up, 3 median elbow flexion was 125 degrees (range 110 – 130 degrees), and median MEPS was 85 (range 70 – 100).
| Patient # | Sex | Age (years) | Trauma mechanism | Type of fracture | Distal segment length |
|---|---|---|---|---|---|
| 1 | Radial n. praxia | 20-110° | 80-120° | 12A | 8.5 cm |
| 2 | Radial n. praxia | 10-110° | 80-120° | 12B | 7.5 cm |

DISCUSSION
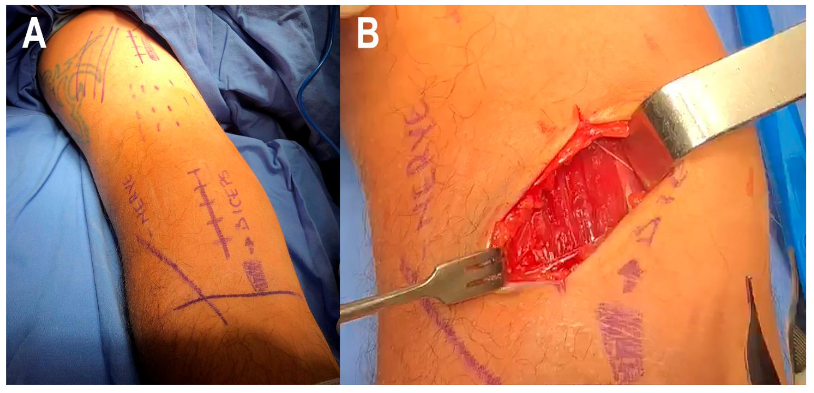
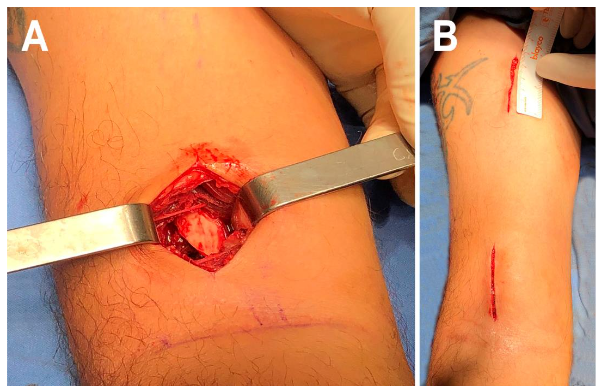
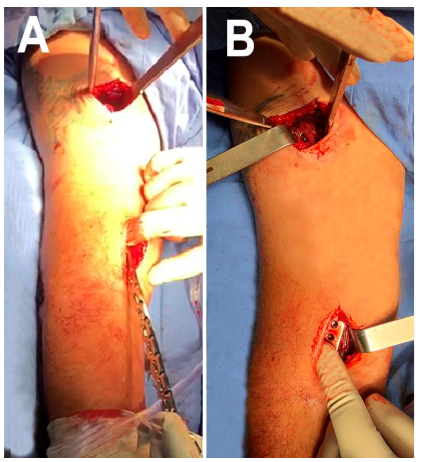
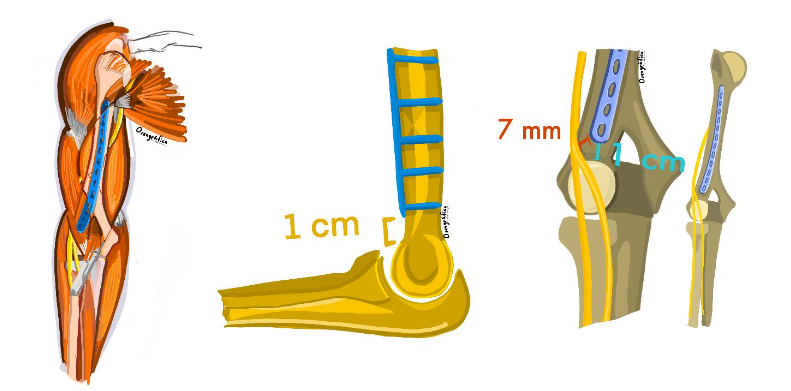
The study showed satisfactory mid-to-long-term clinical and functional outcomes and low complication rates in patients with DHF treated with a MIPO with an anterolateral fixation following the technique described by Mejía et al. In our series of ten patients, 80% had recovered the AROM, and 60% functionally recuperated after six- and twelve-months post-surgery, respectively. Only two patients presented radial nerve praxia, which resolved without long-term consequences. Fifty percent of the patients had shown a stable fixation and good clinical results in the mid-to-long term.
ORIF is probably the most used surgical treatment for distal DHF; however, MIPO, through an anterolateral approach, has been gaining more attention due to its advantages, such as less soft tissue dissection and lower complication rates.
CONCLUSION
For meta-diaphyseal and distal diaphyseal extra-articular humerus fractures, a MIPO technique with an anterior approach and anterolateral fixation provided a stable reduction and fixation with satisfactory mid-to-long term results.
ACKNOWLEDGMENTS
The authors have no conflicts of interest to declare.
REFERENCES
1. Miguelh L.A., Stephens B., Stone G.P., Cottrell B.J., Yamini N., Shultz M. Anterior intramedullary fixation for distal humeral shaft fractures. Injury. 2015 Jan;46(1):91-604.
2. Nowak L., Dehghan N., McKee M.D., Schemitsch E.H. Plate fixation for management of humerus fractures. Injury. 2018 Jun;49:533-8.
3. Morrey J.E., Morrey B.F., Sanchez-Sotelo J., Barlow J.D., O’Driscoll S. A review of the surgical management of distal humerus fractures and nonunions: From fixation to arthroplasty. J Clin Orthop Trauma. 2021; 12: 1-10.
4. Bealley J.C., Barza N., Jordan M.C. Minimally invasive plate osteosynthesis for distal humeral fractures. J Orthop Trauma. 2011; 25(11):1333-63.
5. Beasley J.C., Goyal G.S., Garg R., Hanke J., Yamin N., Shultz M. Anterior intramedullary fixation for distal humeral shaft fractures: surgical tactics and a clinical series. European Journal of Orthopaedic Surgery and Traumatology. 2020 Dec 1;30(8):1151-21.