Outcomes of Vitrectomy for Type 2 MacTel Patients
Surgical and visual outcomes of small-gauge pars plana vitrectomy for full-thickness macular hole associated with type 2 idiopathic macular telangiectasia
Matthew A. Cunningham, MD1, Elias C. Mavrofrides, MD1, Luke Mavrofrides, MD2, Emily Schofield, MD3
University of Florida College of Medicine, Gainesville, Florida 32611
OPEN ACCESS
PUBLISHED: 30 December 2024
CITATION: CUNNINGHAM, Matthew A. et al. Surgical and visual outcomes of small-gauge pars plana vitrectomy for full-thickness macular hole associated with type 2 idiopathic macular telangiectasia. Medical Research Archives, [S.l.], v. 12, n. 12, dec. 2024.Available at: <https://esmed.org/MRA/mra/article/view/6187>.
COPYRIGHT: © 2025 European Society of Medicine. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
DOI: https://doi.org/10.18103/mra.v12i12.6187
ISSN 2375-1924
Abstract
Objective: To examine the clinical features and outcomes of pars plana vitrectomy for full-thickness macular hole (MH) in patients with type 2 macular telangiectasia (MacTel).
Methods: Retrospective, interventional case series of consecutive patients with MacTel type 2 who underwent surgical repair of full thickness macular holes from January 2015 to January 2021 at a busy vitreoretinal surgery practice. The rate of macular hole closure, and visual outcome following repair were evaluated.
Results: Eight eyes of MacTel patients with full thickness macular holes were identified; however, 4 of these eyes did not meet inclusion criteria (i.e. no surgical intervention, or inadequate follow up after surgical intervention). Macular hole closure was achieved in 100% of eyes, with one eye requiring multiple surgeries to obtain closure. The mean preoperative visual acuity was 0.775 logMAR units (20/119 Snellen Equivalent) and improved to 0.725 logMAR units (20/106 Snellen Equivalent, Wilcoxon test, p=0.854), at the last known follow-up after macular hole repair. Overall, 50% patients had improvement in visual acuity at the final postoperative visit. There were no cases of postoperative retinal tears, breaks, or endophthalmitis.
Conclusions: Macular hole formation in patients with Macular telangiectasia type 2 is rare. Macular hole closure was eventually achieved in 100% of eyes. Although favorable anatomic results can be obtained with vitrectomy surgery, the postoperative visual gains are variable.
Objective: To examine the clinical features and outcomes of vitrectomy for full-thickness macular hole (MH) in patients with type 2 idiopathic macular telangiectasia.
Keywords: macular hole, vitrectomy, idiopathic macular telangiectasia, visual outcomes
Introduction
Macular telangiectasia is a condition of the retina that is characterized by abnormalities in the perifoveal blood vessels.¹⁰ It was first described as idiopathic juxtafoveolar retinal telangiectasis by Gass in 1968.¹¹ ¹² It was later classified into different types. There are 3 types of macular telangiectasia with type 2 (MacTel) being the most common.¹³ MacTel causes bilateral foveal degeneration and is characterized by neurosensory atrophy, alterations of the macular capillary network, and foveal cystic changes most evident on optical coherence tomography (OCT). Patients usually are diagnosed in or after their fourth decade of life with symptoms such as metamorphopsia and decreased ability to read.¹⁴ ¹⁵
The etiology of MacTel is still unknown although recent reports have focused on Mueller cell abnormalities rather than primary capillary degeneration.⁸ ¹⁶ Another study by Gantner et al looked at serine and lipid metabolism as part of the pathophysiology of MacTel finding that these patients typically have low serine levels.¹⁶ ¹⁷
Idiopathic full-thickness macular holes (FTMH) are a common source of central vision loss in older adults without any other macular pathology. Idiopathic FTMH have an extremely high rate of successful closure with modern surgical techniques.¹⁸ In MacTel, full-thickness macular holes are a rare complication that can cause further visual dysfunction. Due to the limited number of reported cases, there is a lack of data on the ultimate surgical and visual outcomes for MacTel associated FTMH. To our knowledge, there have only been 12 studies with a total of 38 eyes reporting outcomes for surgical repair of FTMH associated with MacTel. Based on these studies, the macular hole is far less likely to remain closed following surgical repair in the presence of MacTel (50%) as compared to idiopathic macular holes (closure rates > 90%).¹⁸
We present the visual and surgical outcomes of our patients in a vitreoretinal private practice. The authors also compare our surgical results with those previously reported cases.
Methods
A retrospective chart and electronic medical record review of patients with MacTel type 2 undergoing surgical repair for macular hole with 23- or 25-gauge pars plana vitrectomy at a busy, multiple-physician vitreoretinal surgery practice from January 2015 to January 2021 were reviewed. Due to the prevalence of this disease process a six year time frame was determined to be adequate to identify enough patients to meet the inclusion criteria.
Institutional Review Board (IRB) approval for this HIPAA-compliant, retrospective analysis was obtained from Advarra Institutional Review Board for Human Subjects Research, and the study adhered to the tenets set forth in the Declaration of Helsinki. Informed consent was not required due to the retrospective nature of this study.
The patients with MacTel type 2 were identified by the ICD-9 codes 362.15, and ICD-10 code H35.079. All cases undergoing macular hole repair were identified using CPT codes 67042. Chart review of clinic notes, operative reports, and surgical logs were used to confirm these cases.
For macular hole repair, all patients underwent 23- or 25-gauge PPV with internal limiting membrane peeling, gas tamponade, and post-operative face down positioning. Demographic data (including age and gender), initial ophthalmic presentation, presence of posterior vitreous detachment (PVD) and ERM, ophthalmic findings, and any postoperative complications were recorded.
All patients underwent examination on postoperative day 1, week 1, and month 1 after surgery. A minimum follow-up duration of 3-months was required to evaluate surgical outcomes, including MH closure rate and visual acuity (VA) improvement (Snellen). Exclusion criteria included history of venous or arterial occlusive disease and advanced glaucoma.
The mean and standard deviation of preoperative and postoperative vision were calculated after the conversion to the logarithm of minimum angle of resolution (logMAR) equivalent of each patient’s Snellen visual acuity. Visual acuity was recorded at time of MH diagnosis and at the most recent visit following MH surgery. The paired t-test was used to compare VA between the preoperative values, specifically prior to the repair of the MH and those obtained following surgery at the most recent visit. In all analyses, a two-tailed P value of less than 0.05 was considered statistically significant.
This study was a retrospective review of patients undergoing pars plana vitrectomy for the treatment of MH associated with MacTel2. The study was approved by the institutional review board.
Results
There were a total of 1261 MH repairs during the study period, of which eight had MacTel type 2 during the 6-year study period. Four of the 8 patients met the study criteria of having a MacTel type 2 diagnosis, undergoing vitrectomy repair of a macular hole, and having follow-up of at least 3 months.
All four patients included in the study were female with the average age of 74.5 years (range 68–81 years). Three of the 4 cases were phakic at the time of MH repair. All patients included in the study underwent 23- or 25-gauge PPV with internal limiting membrane peeling and gas tamponade for the MH repair (Table 1). Three of the patients had long term, successful closure of the hole with one surgery as seen in Figure 1. One of the patients (case #4) required a total of 3 surgeries to attain closure of the macular hole, as seen in Figure 2. Therefore, macular hole closure was eventually accomplished in 4/4 (100%) eyes, at the last follow up (average 16 months, range 9–25 months).
The mean preoperative VA (prior to MH repair) was 0.775 logMAR units (20/119 Snellen Equivalent) and improved to 0.725 logMAR units (20/106 Snellen Equivalent, p=0.854), at the last known follow-up after MH repair. Overall, 50% of patients had improvement in VA at the final postoperative visit, 1 patient had the same VA, and 1 patient experienced VA loss despite MH repair. A final VA of 20/200 or better was achieved in 100% of cases.
The four patients that were not included were all female with an average age of 73.25 ± 2.6 years. The average diameter of the macular holes in these four patients was 950 ± 191.5 microns, compared to an average macular hole diameter of 408.75 microns in the four included patients. These optical coherence tomography images are shown in Figure 3. The visual acuity in these four patients were: 20/400, 20/70, 20/100, and 20/200; the mean visual acuity was 0.875±0.35 logMAR units. One patient underwent pars plana vitrectomy, but was lost to follow-up after post-operative week 1; the other 3 patients were offered surgical intervention, but deferred. Therefore, in this study, surgery was completed on 5 eyes, with one patient excluded due to lack of follow up.
Discussion
Full thickness macular holes, in the setting of MacTel, are an uncommon but potentially visually significant issue. The variable hole closure rates and visual outcomes after surgical management leads to uncertainty about the best management course in these patients. A recent study by Miller et al found no significant difference in VA between surgically treated and medically managed patients with MacTel associated FTMH; the authors further recommended that these patients may benefit more from observation than surgical intervention.⁹ In contrast, Ahmad et al found VA improvements (ranging from 20/50–20/200 pre-operatively, to 20/20–20/40 post-operatively) in all four cases with successful macular hole closure.⁸ These results support surgical intervention.
In our series, we found that FTMH developed in 8 patients with MacTel during a 6-year study period. Although 5 of the 8 patients underwent surgical intervention, only 4 patients met inclusion criteria based on follow-up. We were able to achieve long-term closure of the FTMH in all four cases, but only three of these cases were closed with a single surgery. Our closure rate of 75% with a single surgery (and 100% overall) is higher than the previously reported closure rates in this condition, which is around 50%.
In our cases with FTMH closure after a single surgery, visual improvement was achieved in two of the three cases. One patient (Case #1) improved from 20/100 to 20/60 and Case #2 from 20/200 to 20/50. The third patient (Case #3) remained the same at 20/200, but had concomitant macular degeneration which likely played a role in the final visual outcome.
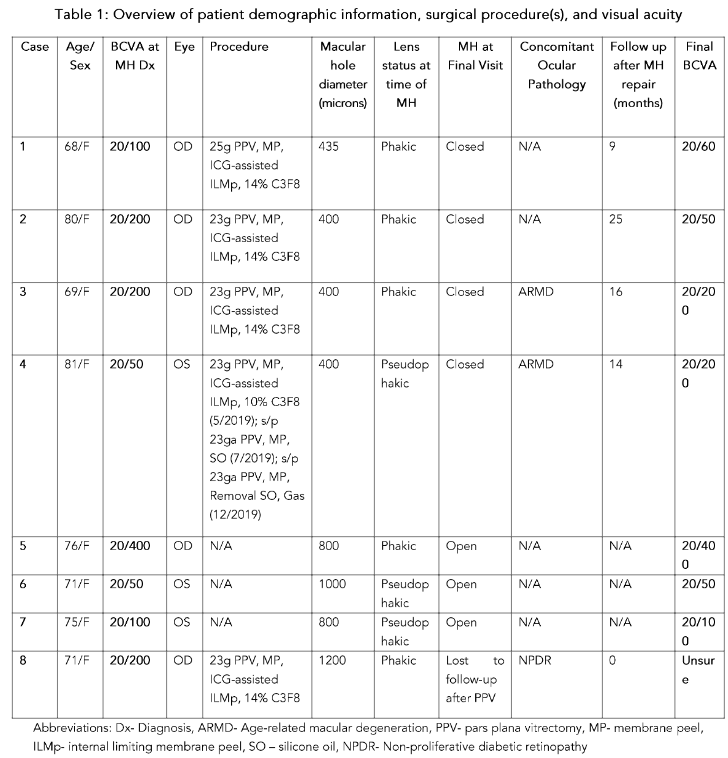
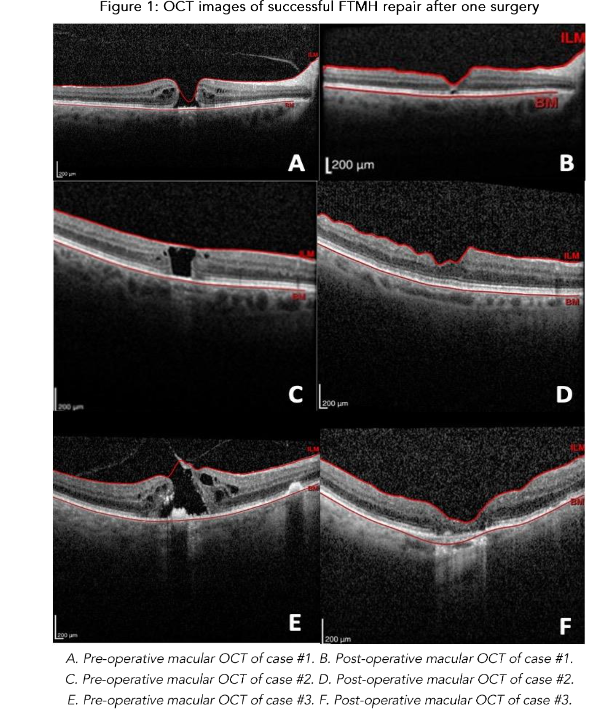
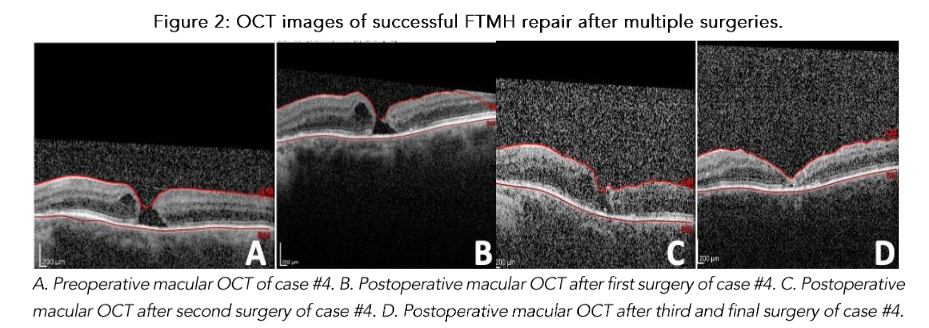
Figure 2: OCT images of successful FTMH repair after multiple surgeries.

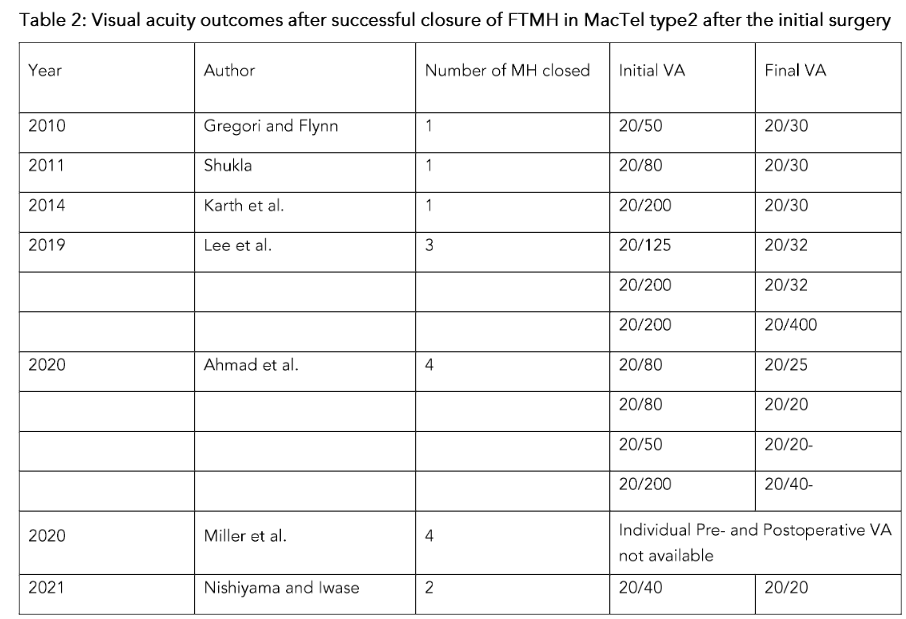
Other studies have also shown impressive visual improvements when the hole closes following the initial surgery. Table 2 details the visual outcomes achieved after successful long-term closure of the macular hole after the initial surgery. In these cases, the average pre-operative visual acuity was zero point seven zero six logMAR (approximately twenty over one hundred one point four Snellen equivalent) and improved to zero point three one seven six logMAR (approximately twenty over forty-one point six Snellen equivalent) post-operatively. Miller et al. did not provide individual preoperative and postoperative visual acuity changes for patients, so this study’s data was excluded from the analysis. Interestingly, visual improvement was seen in fifteen of the seventeen patients (eighty-eight point two percent) that achieved hole closure after a single surgery. Although successful closure with a single surgery is lower in patients with MacTel type two (fifty percent) as compared to idiopathic FTMH (over ninety percent), notable visual acuity gains are frequently achieved in these cases. This information can be used when guiding patients with FTMH and MacTel whether to proceed with surgical repair.
This data also suggests that improving macular hole closure rates after an initial surgery could result in improved overall visual outcomes. Ahmad et al suggests that Mueller cell loss results in foveal instability and tissue loss making hole closure more difficult in MacTel type two. Identifying risk factors or OCT characteristic that increase the likelihood of developing a FTMH in MacTel type two could be vital to early identification and repair of the hole, potentially improving initial closure rates. Further understanding of the pathophysiology of the underlying condition and potential factors contributing to the development of the FTMH, may also help improve surgical techniques and initial closure rates. In this regard, recent techniques like the use of the ILM inverted flap could be beneficial in improving initial hole closure rates, but further investigation is necessary. The study by Rangel et al. found success with the use of plasma rich growth factor in treating the FTMH in one patient with MacTel, but more studies will need to be done to prove the efficacy.
One of our patients did not achieve hole closure after the initial surgery (Case number four). An additional two surgeries were required in order to achieve long term MH closure in this patient. Despite the long-term hole closure, the patient experienced vision loss from twenty over fifty to twenty over two hundred. This suggests that reoperation to achieve hole closure may have a poorer visual prognosis. Nevertheless, two recent papers have reported the use of autologous ILM grafts to manage a persistent macular hole in MacTel patients after failure of the initial PPV with standard ILM peeling. These cases achieved both anatomic closure and visual improvement. This may be a promising approach in those patients that have failed initial surgery. Further investigation and reporting of this technique is also warranted.
Our study is limited by its retrospective nature and the small number of patients included, which is expected based on the uncommon incidence of this condition. The authors believe our case series will add to the literature on this rare condition, and help guide clinicians on presenting options to patients with MacTel associated macular holes. We demonstrated excellent anatomic hole closure after initial surgery (in three cases) with standard vitrectomy, ILM peeling, gas tamponade, and strict prone positioning. Overall, the authors demonstrated a final one hundred percent closure rates in our four cases, with variable post-operative visual gains.
Conclusion
Macular telangiectasia is a rare disease with type two being the most common. It is uncommon for patients with macular telangiectasia type two to develop full thickness macular holes. In our case series we were able to demonstrate a one hundred percent closure rate with notable postoperative visual improvement. thickness macular holes in patients with type two macular telangiectasia, but it is important to note that the visual outcomes might not always be achieved even with successful surgical closure. Based on previous studies, including our cases, the authors recommend surgical intervention in MacTel patients with a macular hole diameter less than four hundred fifty micrometers. We also suggest discussing that the best chance for visual improvement usually occurs if the macular hole closes after the initial repair.
Ethical Approval:
Ethical approval was obtained from the University of Florida Institutional Review Board for Human Subjects Research (Pro00028884).
Statement of Informed Consent:
The authors declare that informed consent was not sought for the specifics of their research, authoring, and/or publication of this article.
Funding:
The authors declare no financial support for the research, authorship, and/or publication of this article.
Acknowledgments:
We would like to thank Lesa Melaugh for her assistance.
References
[2] Rishi P., Kothari A. R. Parafoveal telangiectasia (PFT) has been associated with changes in macular architecture and macular holes (lamellar and full thickness)Retina. 2008;28(1):184–185. doi:10.1097/IAE.0b013e31815e98c0
[3] Gregori N., Flynn H. W. Surgery for full-thickness macular hole in patients with idiopathic macular telangiectasia type 2. Ophthalmic surgery, lasers and imaging retina. 2010
doi: 10.3928/15428877-20100726-10.
[4] Karth P. A., Raja S. C., Brown D. M., Kim J. E. Outcomes of macular hole surgeries for macular telangiectasia type 2. Retina. 2014;34(5):907–915. doi: 10.1097/IAE.0000000000000009.
[5] Lee S. C., Hwang D. J., Lee K. M., Park Y. S., Sohn J. H. Surgical outcomes of macular telangiectasia type 2 associated with macular hole. Journal of Retina. 2019;4(2):48–54. doi: 10.21561/jor.2019.4.2.48.
[6] Charbel Issa P., Scholl H. P. N., Gaudric A., et al. Macular full-thickness and lamellar holes in association with type 2 idiopathic macular telangiectasia. Eye. 2009;23(2):435–441. doi: 10.1038/sj.eye.6703003.
[7] Patel P., Flaxel C. Visual and anatomic outcomes in eyes with idiopathic juxtafoveal macular telangiectasia (MacTel) and full thickness macular holes undergoing surgical repair. Enliven: Clin Ophthalmol Res. 2015;1(1):p. 005.
[8] Ahmad KT, Chacko J, Sallam AB, Warner DB, Uwaydat SH. Surgical Outcomes in Macular Telangiectasia Type 2-Related Macular Holes: A Report on Four Patients. Case Rep Ophthalmol Med. 2020;2020:8884638.
[9] Miller, A. G., Chandra, R., Pophal, C., Schartman, J. P., Hornik, J. H., & Miller, D. G. (2020). Efficacy of Macular Hole Surgery in Patients with Idiopathic Macular Telangiectasia Type 2. Ophthalmology. Retina, 4(5), 494–497.
[10] Nishiyama, S., & Iwase, T. (2021). Two years outcomes of treating full-thickness macula hole associated with idiopathic macular telangiectasia type 2 by internal limiting membrane inverted flap technique: Case reports. Medicine, 100(36), e27078.
[11] Gass JD, Oyakawa RT. Idiopathic juxtafoveolar retinal telangiectasis. Arch Ophthalmol. 1982;100 (5):769-780. doi:10.1001/archopht.1982.01030030773010
[12] Gass JD, Blodi BA. Idiopathic juxtafoveolar retinal telangiectasis. Update of classification and follow-up study. Ophthalmology. 1993;100(10): 1536-1546.
[13] Yannuzzi LA, Bardal AM, Freund KB, Chen KJ, Eandi CM, Blodi B. Idiopathic macular telangiectasia. Arch Ophthalmol. 2006;124(4):450-460. doi:10.1001/archopht.124.4.450
[14] Gillies MC, Zhu M, Chew E, et al. Familial asymptomatic macular telangiectasia type 2. Ophthalmology. 2009;116(12):2422-2429. doi:10.1016/j.ophtha.2009.05.010
[15] Kedarisetti KC, Narayanan R, Stewart MW, Reddy Gurram N, Khanani AM. Macular Telangiectasia Type 2: A Comprehensive Review. Clin Ophthalmol. 2022;16:3297-3309. Published 2022 Oct 10. doi:10.2147/OPTH.S373538
[16] Zucker CL, Bernstein PS, Schalek RL, Lichtman JW, Dowling JE. High-throughput ultrastructural analysis of macular telangiectasia type 2. Front Ophthalmol (Lausanne). 2024;4:1428777. Published 2024 Jul 30. doi:10.3389/fopht.2024.1428777
[17] Gantner, M. L., Eade, K., Wallace, M., Handzlik, M. K., Fallon, R., Trombley, J., Bonelli, R., Giles, S., Harkins-Perry, S., Heeren, T. F. C., Sauer, L., Ideguchi, Y., Baldini, M., Scheppke, L., Dorrell, M. I., Kitano, M., Hart, B. J., Cai, C., Nagasaki, T., Badur, M. G., … Friedlander, M. (2019). Serine and Lipid Metabolism in Macular Disease and Peripheral Neuropathy. The New England journal of medicine, 381(15), 1422–1433. https://doi.org/10.1056/NEJMoa1815111
[18] Ittarat, M., Somkijrungroj, T., Chansangpetch, S., & Pongsachareonnont, P. (2020). Literature Review of Surgical Treatment in Idiopathic Full-Thickness Macular Hole. Clinical ophthalmology (Auckland, N.Z.), 14, 2171–2183. https://doi.org/10.2147/OPTH.S262877
[19] Sborgia, G., Niro, A., Coassin, M., Sborgia, L., D’Oria, F, Pastore, V., Albano, V., Tritto, T., Sborgia, A., Boscia, F., & Alessio, G. (2021). Inverted internal limiting membrane-flap technique to treat a full-thickness macular hole complicating idiopathic macular telangiectasia type 2. European Journal of Ophthalmology, 31(2) NP81-NP85.
doi: 10.1177/1120672119886177
[20] Rangel, C., Blanco, N., Pedraza-Concha, A., Gomez, M., Parra, M., & Arias, J. (2022) Plasma rich in growth factors as treatment for a full0 thickness macular hole due to macular telangiectasia type 2. Arch Soc Esp Oftalmol. 2022; 97:219:223
[21] Hewson, A., McAllister, A., & Reddie, I. (2020). Autologous neurosensory retinal flap for closure of refractory macular hole in a patient with macular telangiectasia. American journal of ophthalmology case reports, 18, 100644.
[22] Bozdogan, Y. C., Erol, M. K., Suren, E., & Gedik, B. (2021). Internal limiting membrane graft in full-thickness macular hole secondary to macular telangiectasia type 2. Journal francais d’ophtalmologie, 44(9), 1419–1424.


