Maternal Health Literacy and Empowerment: A Review
Maternal Health Literacy and Empowerment in the United States: A Scoping Review
Elena T. Carbone, DrPH, Professor and Associate Dean1, Sandra A. Smith, PhD, Health Literacy Consultant2, Amos Laar, PhD, Professor3, Robert Akparibo, PhD, Associate Professor4
OPEN ACCESS
PUBLISHED: 30 December 2024
CITATION: CARBONE, Elena T. et al. Maternal Health Literacy and Empowerment in the United States: A Scoping Review. Medical Research Archives, [S.l.], v. 12, n. 12, dec. 2024.Available at: <https://esmed.org/MRA/mra/article/view/6182>.
DOI: https://doi.org/10.18103/mra.v12i12.6182
ISSN 2375-1924
ABSTRACT
Background: Global health scholars argue that efforts to improve maternal health literacy and empowerment can produce greater, more sustainable benefits than simple information-giving or health education. Further, efforts might differentially impact disadvantaged mothers and thereby reduce inequities. There is a substantial body of literature on improving maternal-child health, but relatively little on maternal health literacy. While empowerment and health literacy are closely related, they have rarely been addressed together.
Aims: This scoping review aims to: 1) examine the extent, range and nature of research related to maternal health literacy and empowerment; and 2) assess the potential value of a global systematic review. Specifically, this scoping review summarizes and synthesizes U.S. researchers’ reports about improving maternal health literacy and empowerment among women who are pregnant or raising infants/toddlers in poverty.
Methods: We searched MEDLINE and Google Scholar for primary sources addressing maternal health literacy in relation to health empowerment. Multiple keyword combinations captured sources throughout the medical and public health literature.
Results: Twelve studies met the inclusion criteria. Interventions were set in maternal-child health promotion programs (n=6) or prenatal care (n=1). Qualitative studies (n=5) elucidated mothers’ perceived health risks, decision networks, and experiences with prenatal care, immunizations, and technology. Overall, findings indicate that with support, mothers can learn interactive (social) and critical (thinking) skills that enable them to better manage their health and the health of their families, even if they have low functional literacy skills.
Conclusion: U.S. research related to maternal health literacy and empowerment is limited and not empirically robust. Due to measurement and definitional variation, a global systematic review is unlikely to allow comparison of intervention designs and evaluation. However, analysis of global findings from community-based participatory research, health education initiatives, and qualitative studies may aid identification and understanding of barriers, facilitators, and meaningful indicators of maternal health literacy and empowerment within and across cultures.
Keywords: Health Literacy, Empowerment, Maternal Health Literacy, Maternal Child Health, Scoping Review.
1. Introduction
This scoping review aims to examine the extent, range and nature of research related to maternal health literacy and empowerment and assess the potential value of a global systematic review.¹ Specifically, we summarize and synthesize U.S. research about improving maternal health literacy and empowerment among women who are pregnant or raising infants/toddlers in poverty. Findings could inform efforts to implement a recommendation of the United Nations General Assembly to reduce health disparities worldwide by improving health literacy in parents and empowering women.² ³
1.1. IMPROVING MATERNAL HEALTH LITERACY: AN EMPOWERMENT STRATEGY
In accordance with the United Nations call to action, we use the World Health Organization’s definition of health literacy:
“personal knowledge and competencies that accumulate through daily activities, social interactions and across generations [which]… are mediated by the organizational structures and availability of resources that enable people to access, understand, appraise and use information and services in ways that promote and maintain good health and well-being for themselves and those around them.”⁴
Maternal health literacy has been defined as obtaining cognitive and social skills, which empower women to better access, evaluate, understand, and use information to improve and maintain their health.⁵ By improving access to understandable and trustworthy health information, and capacity to use it effectively, health literacy is critical to empowering mothers to make decisions about their own personal health, as well as the health of their families.⁴
Also, Bertelsen and Holland⁶ define empowerment as a person’s or group’s “ability to make a choice and transform that choice into their desired actions and outcomes.” In the field of health education, empowerment is viewed as “a process through which people gain greater control over decisions and actions affecting their health.”⁴ Thus, promoting maternal health literacy is an empowerment strategy to increase mothers’ control, individually or in communities, over personal and child health.⁷ Indeed, the World Health Organization has identified health literacy and women’s empowerment as key components of maternal health improvement programs to achieve a sustainable future, encourage further research, reform policies and laws, and raise awareness.⁸
Mothers achieve and demonstrate maternal health literacy and empowerment by increasing their capacity to make health and healthcare choices for themselves and their children, act on those choices, and produce desired outcomes.⁶ This conceptualization differentiates maternal health literacy from health literacy in mothers as operationalized in many U.S. studies⁹ by:
-
focusing on action rather than understanding,
-
intending to empower rather than to educate, and
-
increasing skills and autonomy rather than improving information.
Early health literacy research often referred only to functional literacy skills (reading, numeracy) needed to access healthcare services and follow instructions. However, in keeping with more recent definitions of health literacy, maternal health literacy refers to the full range of literacy skills including functional skills, interactive (social) skills and critical (thinking) skills that empower mothers to prevent disease and promote health in home and community settings.¹⁰
Maternal health literacy is viewed as an empowering personal and community asset that can be developed.¹¹ This stands in contrast to a majority of early research in health literacy that investigated the construct as an individual function-focused attribute that is a risk to patients and healthcare systems.
Maternal health literacy may be both individual and distributed. Distributed maternal health literacy refers to the collective skills, practices, knowledge, and experience of a mother’s social networks. Mothers may draw on the skills of others to seek, personalize, and use health information, make decisions and plans, access care and resources, and take action.¹² ¹³
1.2. MATERNAL HEALTH LITERACY, EMPOWERMENT, AND HEALTH DISPARITIES
Improving maternal health literacy and empowering poor mothers may reduce disparities by enabling mothers to more effectively utilize and influence the quality of available health and social services, reduce risks, and maximize protective factors for themselves and their families.¹⁰ A mother’s health status, and her health- and healthcare-related practices and behaviors during pregnancy and early parenting, influence her child’s health across the life course.¹⁴ ¹⁶ While educational interventions can have both long- and short-term benefits, these benefits are socially distributed and do little to address underlying inequities.⁹ Global health scholars¹⁷ argue that efforts to improve health literacy and empowerment can produce greater and more sustainable benefits than information-giving or education. Further, efforts seem to differentially impact disadvantaged mothers and improve disparities and inequities.
2. Aims and Research Questions
The aims of this review were to examine the extent, range, and nature of research related to maternal health literacy and empowerment and assess the potential value of a global systematic review. This review represents one step in formulating a response to the United Nations recommendation that member countries undertake efforts to improve health literacy in parents and empower women as a global strategy to address health disparities.² ³ It focuses on mothers as the most powerful influence on child and family health and healthcare worldwide.¹⁸ Because age 0 to 3 years is identified as the most significant period of human development during which a person’s lifetime health trajectory is set,¹⁶ and because disease and low health literacy are associated with socio-economic disadvantage,¹⁹ we focused on maternal health literacy and empowerment among pregnant women and mothers raising infants and toddlers in poverty.
We purposefully took a broad view; therefore, seven research questions guided this process:
- What research has been generated on maternal health literacy and its improvement, and in what settings?
- What interventions have been reported to improve maternal health literacy?
- What experiences or situations have been documented through qualitative studies?
- How is maternal health literacy related to empowerment?
- How do maternal health literacy and empowerment develop?
- What supports or impedes improvement of maternal health literacy and empowerment?
- How has improvement of maternal health literacy and empowerment been measured?
3. Methods
3.1. APPROACH TO THE SCOPING REVIEW
We cast a broad net because the material related to maternal health literacy is poorly indexed and scattered throughout medical and public health databases. Empowerment research is scant in public health literature and nearly non-existent in medical literature; most is found in community development literature.²⁰
The objectives, inclusion criteria, and methods of this review adhere to the framework outlined in the Joanna Briggs Institute Reviewers’ Manual for scoping reviews.²¹ See Table 1 for details.
Table 1. Stepwise Approach to the Scoping Review
| Step | Activity |
|---|---|
| 1 | Discussion with health sciences librarian. |
| 2 | Preliminary literature review/develop research question. |
| 3 | Develop search strategy. |
| 4 | Initial title review, identify filters. |
| 5 | Develop inclusion/exclusion criteria. |
| 6 | Merge searches (omit duplicates). |
| 7 | Abstract review. |
| 8 | Develop Data Charting Form. |
| 9 | Full text review. |
| 10 | Identification of relevant articles. |
Adapted from Arksey and O’Malley.¹
Accordingly, this review establishes the extent and nature of the literature, but not the quality of studies. Two teams of reviewers adapted a search strategy developed by colleagues at the University of Sheffield²⁷ and synthesized results. An initial search in MEDLINE/PubMed, CINAHL, Science Direct, Google Scholar, and Web of Science databases revealed extensive duplication of citations and no previous scoping review on maternal health literacy. Therefore, we focused on MEDLINE/PubMed and Google Scholar and included other studies from gray literature that met our inclusion criteria.
3.2. INCLUSION AND EXCLUSION CRITERIA
Studies conducted in the U.S. that addressed maternal health literacy or health literacy or empowerment in mothers of children to age three published in English and available online were included in the review. Studies specific to maternal conditions (e.g., diabetes or HIV), or child conditions (e.g., asthma), which imply special medical needs and extra health literacy demands, were excluded, as well as studies related to preconception care, pregnancy planning, and pregnancy complications. Studies with special populations, such as mothers exposed to toxins, older mothers, and women with disabilities, were also excluded.
To reduce the sheer magnitude of sources, those that did not mention health literacy or a synonym in the abstract were excluded. Studies that operationalized maternal health literacy as mothers’ reading proficiency in a clinical setting, or that aimed primarily to increase knowledge were excluded because:
- improving maternal health literacy cannot rely on information-giving where access to information and ability to apply it are limited²³,
- maternal health literacy promotion cannot be restricted to clinical settings where access is limited, and information from those settings is interpreted and applied in other contexts (e.g., at home) and other domains (e.g., in disease prevention and health promotion)¹⁰,
- while reading skills for gaining knowledge are helpful, interactive skills and critical skills for obtaining, personalizing, and applying information in context can develop in their absence²⁴, and
- empowerment develops along with interactive and critical skills.¹¹ ²⁵
Outcomes of interest were: improvement in individual or community maternal health literacy demonstrated by a specified indicator beyond simple understanding or knowledge gain; impact on health empowerment; and impact on maternal-child health.
3.3. SEARCH STRATEGY
Searches examined individual health literacy and maternal-child health concepts using keywords, synonyms, and Medical Subject Headings (MeSH), including patient education, health education, education/non-professional, and consumer health information and were limited by “United States” and each state name. Health literacy-related terms.
(health literacy, health education, health knowledge, attitudes, behaviors, practices) were defined through a preliminary search of multiple databases with unlimited publication dates and language restricted to English. Maternal-child health terms (maternal and child, mother and child, mothers and children, early childhood well-being, child and maternal health, mother and child health, and mother-child health) were defined through an unrestricted search and refined after the initial search and again upon review of abstracts.²⁶ Phrases were used to delineate pregnancy stage (preconception, prenatal, perinatal, antenatal, postnatal, pregnancy), and outcomes of interest (maternal health and welfare, child health and welfare). A data charting form was used to extract data, merge findings and structure the full text review. Inconsistencies in data extraction were resolved in consultation with the other authors.
4. Results
4.1. QUESTION 1: WHAT RESEARCH HAS BEEN GENERATED ON MATERNAL HEALTH LITERACY AND ITS IMPROVEMENT, AND IN WHAT SETTINGS?
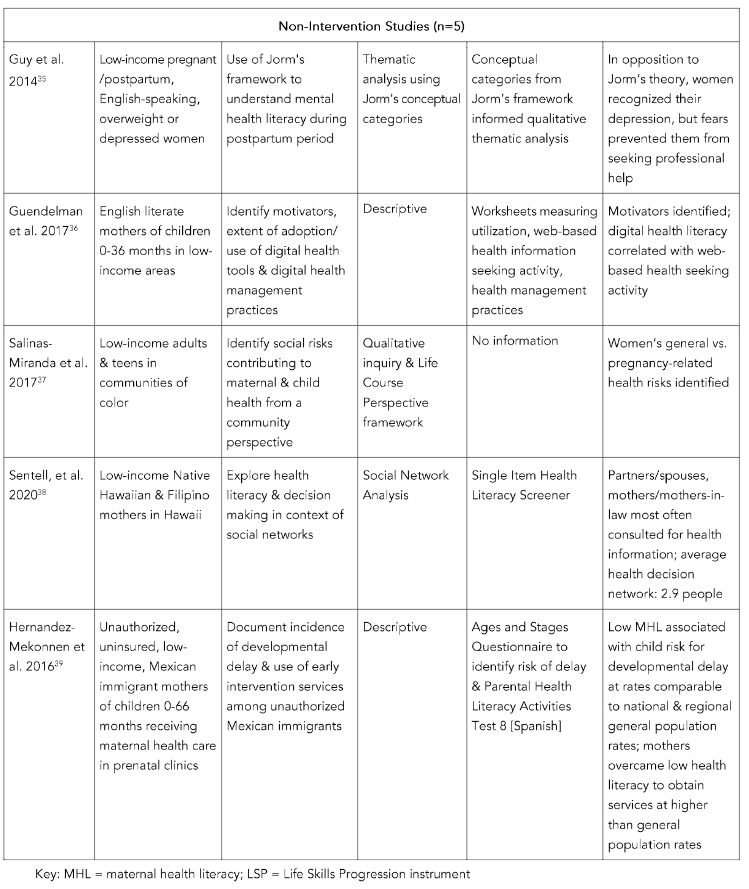
Figure 1 illustrates the study selection process. Table 2 summarizes research study characteristics and findings of the included studies related to research questions #1 – #3.

4. Results
4.1. Question 1: What Interventions Have Been Reported to Improve Maternal Health Literacy?
Records retrieved from searches conducted in electronic databases = 245,879.
Duplicates removed = 11,000.
Records screened = 234,879.
Full-text articles assessed for eligibility = 1,000.
Studies included in the review = 12.

4.2. QUESTION 2: WHAT INTERVENTIONS HAVE BEEN REPORTED TO IMPROVE MATERNAL HEALTH LITERACY?
Roter and colleagues²⁷ conducted a randomized controlled trial to evaluate the impact of a computer program to empower women’s communication in prenatal care by building their interactive skills. Researchers concluded the intervention successfully empowered all participants, including those with low literacy scores to interact more effectively with providers.
Smith and Carroll²⁸ described several quantitative studies evaluating nine implementations of a home-based program to promote maternal health literacy and empowerment, and child development. These studies used the Life Skills Progression instrument²⁹ as the primary data collection tool and service providers’ guide to tailoring interactions to mothers’ specific health and social needs. The Life Skills Progression scale is designed to show progress toward self-reliance and includes indicators of intermediate health outcomes. It includes indicators of change in healthcare services utilization and self-management of health, a reading level estimate, and child development data.
Improvement in outcome measures were found in all studies using the Life Skills Progression instrument, including those with parent educators in school districts³⁰, parents and children in programs served by public school nurses and/or family support workers³¹, depressed and non-depressed parents³², and low-income high risk perinatal women receiving home nursing visits.³³
Willis and colleagues³⁴ applied community-based participatory research principles in a multiphase project to improve information technology literacy and immunization literacy among 1,651 low-income parents/caregivers. The intervention included a web-based Toolkit and Interactive eLearning Café, a social marketing campaign to increase immunization safety awareness, and focus groups to build computer skills and knowledge through observational learning. Exposure to the website was associated with an increase in immunization rate (from 63% to 83%), an indication of improved health literacy.
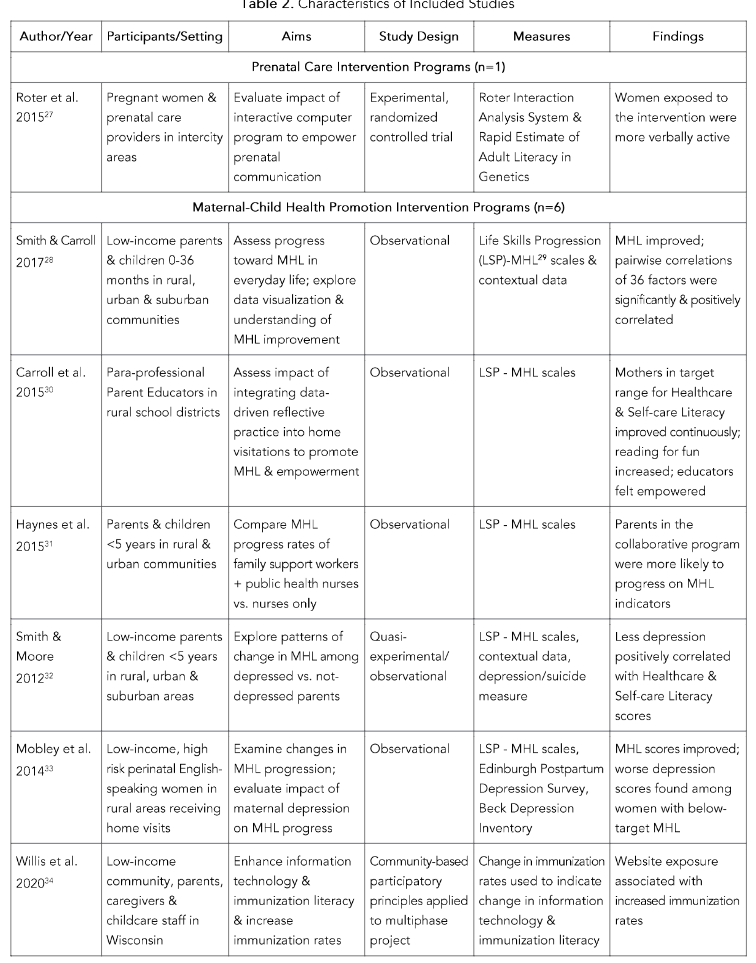
4.3. QUESTION 3: WHAT EXPERIENCES OR SITUATIONS HAVE BEEN DOCUMENTED THROUGH QUALITATIVE STUDIES?
Five non-intervention studies employing qualitative methodology were identified in this review. A secondary analysis of focus group data from 25 depressed or overweight postpartum women demonstrated that emerging maternal health literacy and empowerment can be squelched by external social factors.³⁵ Knowledge enabled women to recognize depression symptoms, but they did not overcome fears related to prior negative encounters with child protective services and health professionals, which inhibited care seeking.
Guendelman and colleagues³⁶ conducted 14 focus groups with 92 new mothers. They evaluated participants’ use of digital health tools for information seeking and health management practices. E-health literacy (defined as self-perceived confidence and skill to find, evaluate, and apply online information to health problems) were associated with widespread information seeking, but not with health management practices. Internal health orientation was a stronger predictor of actual and intentional use of digital health management practices. The authors cautioned that pregnant women’s Internet use should be considered a target for intervention.
Salinas-Miranda and colleagues³⁷ conducted focus groups with 78 low-income teens and adults. Participants identified social determinants of maternal and child health over three periods: women’s childhood, preconception adulthood, and pregnancy. Throughout their lives, participants said women in their communities faced risks of low education, low health literacy (described as inability to find and apply information about health), healthcare challenges, inadequate parenting skills, and financial problems. During pregnancy, these accumulated general risks were exacerbated by lack of support systems, unhealthy diet, obesity, lack of physical activity and unrenlenting stress.
Sentell and colleagues³⁸ used social network analysis to explore distributed health literacy and decision making among low-income mothers and members of their social networks. Mothers were enrolled in home visitation programs to promote maternal health and child development. Mothers reported making health decisions in consultation with up to six others, most often their partners/spouses and mothers/mothers-in-law. The authors concur with others¹² ¹³ that distributed maternal health literacy of social networks can be measured, tested, and changed and that interventions focused on social networks can address disparities by overcoming low-income mothers’ limited access to health experts. They recommend interventions to help support and create community-based peer experts through community health worker programs or support groups.
Hernandez-Mekonnen and colleagues³⁹ found that Spanish-speaking mothers with low health literacy scores were strongly associated with increased child risk of developmental delay, but not with use of early intervention services. Despite their low health literacy scores, along with access barriers related to immigration status, low education and poverty, participants obtained services for 38% of the children at risk, compared to 10% in the general population. The finding that low functional health literacy does not prevent mothers who accept direct information support from overcoming barriers to obtain recommended health services aligns with other studies included in this review.²⁷ ³¹ ³³
Two mixed method intervention studies documented the experience of service providers promoting maternal health literacy and empowerment. Carroll and colleagues³⁰ used proceedings of parent educators’ monthly case conferences with trainers to document their experiences of integrating reflective practices and data collection/interpretation into their usual activities and shifting their intent from educating to empowering. Parent educators felt empowered themselves and viewed reflective questioning as more effective and less stressful than delivering an expert-defined curriculum. Thomas and colleagues⁴⁰ analyzed visit notes of four registered nurse case managers to explain the failure of 37 of 106 participants in an earlier study³³ to achieve maternal health literacy scores in the target range. Explanatory factors were social determinants of health, notably lack of transportation, poor housing, intimate partner violence, and early end to case-management.
4.4. QUESTION 4: HOW IS MATERNAL HEALTH LITERACY RELATED TO EMPOWERMENT?
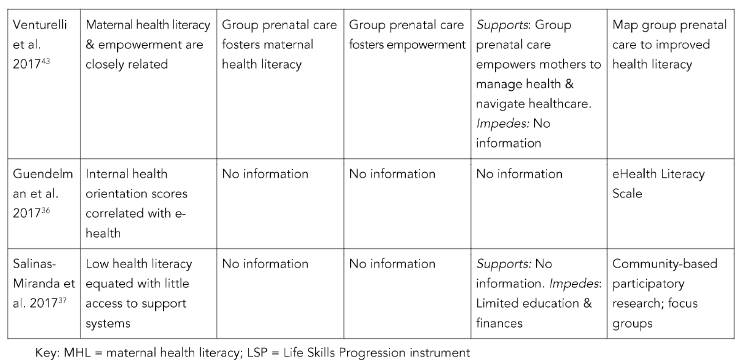
Table 3 presents information about the relationship between maternal health literacy and empowerment related to research questions #4 – #7.
Maternal health literacy and health empowerment are closely related.⁴⁰ In the articles reviewed here, health empowerment is discussed both as a process and an outcome. Carroll and colleagues³⁰ addressed the relationship using Gibson’s Definition of Empowerment, which frames empowerment as “a social process of recognizing, promoting and enhancing people’s abilities to meet their own needs, solve their own problems and mobilize the necessary resources in order to feel in control of their lives.”⁴¹ This definition describes reflective questioning, an empowerment method used in multiple interventions described previously to transfer power to respondents,⁴² position mothers as experts on their children, facilitate self-directed learning, enhance mothers’ capacity to meet their own needs, and support empowerment of both mothers and service providers.³⁰
Gibson’s description of empowerment also aligns with the World Health Organization’s definition of maternal health literacy as an outcome³; namely, skills enabling women to use information and services in ways that enhance health. Roter and colleagues²⁷ described an interactive computerized empowerment process with the intended empowerment outcome of more active participation in prenatal care communication.
In another study,³⁴ technology coupled with health education aided community-based efforts to improve health literacy and child immunization rates in poor minority communities and thereby reduced disparities. Use of web-based platforms and social media networks were credited for success in expanding results to a broader population. Salinas-Miranda and colleagues³⁷ concluded that low health literacy disempowers mothers by limiting their ability to navigate healthcare and social service systems and access to parenting support services.
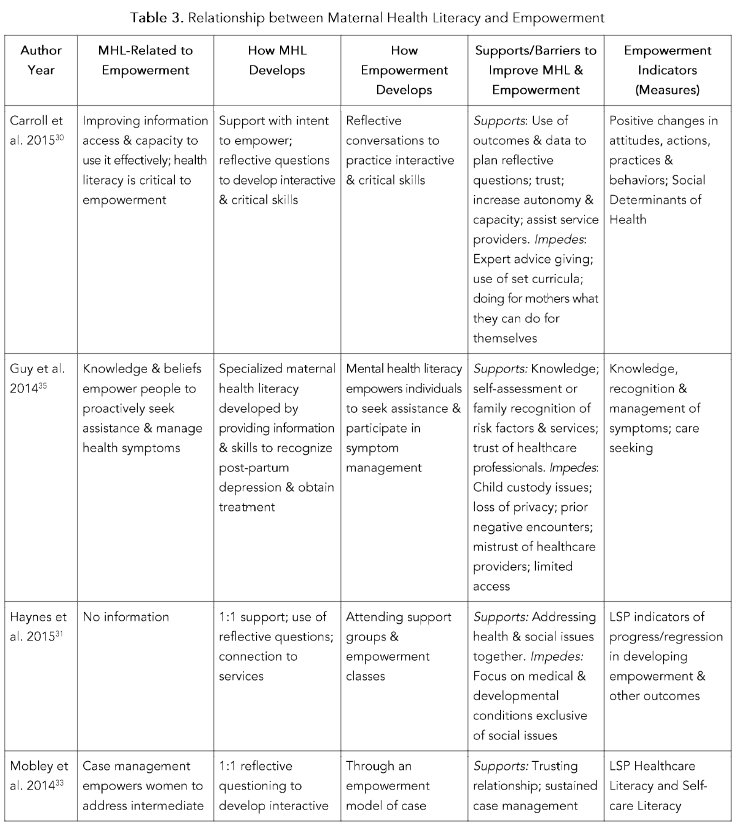
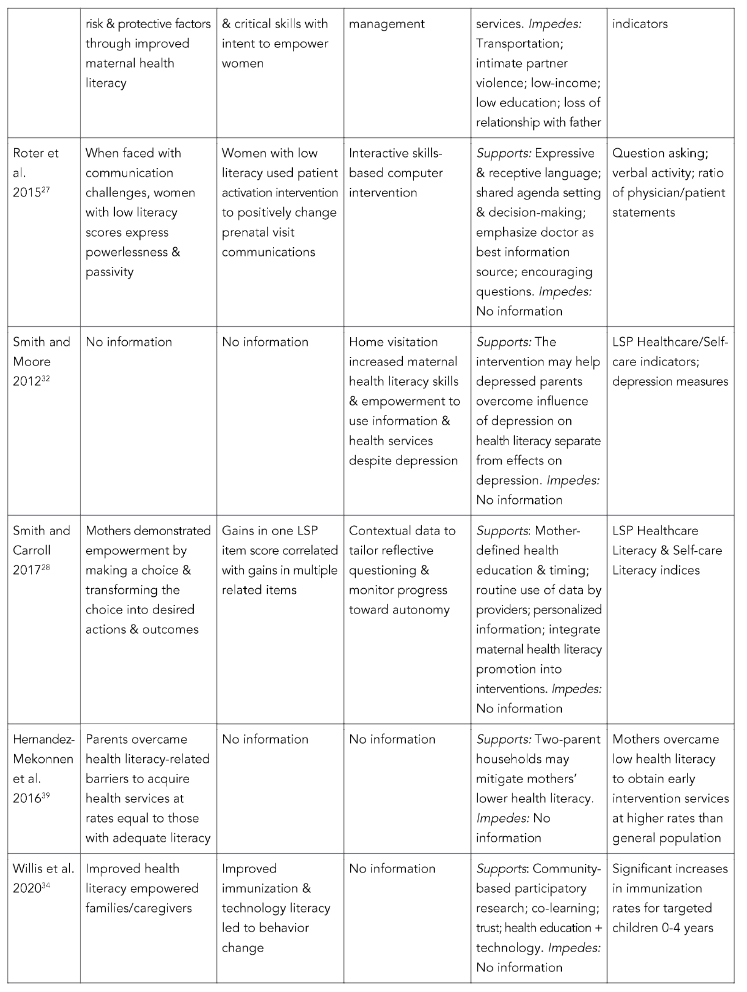
4.5. QUESTION 5: HOW DO MATERNAL HEALTH LITERACY AND EMPOWERMENT DEVELOP?
Reported findings support the premises that health literacy can be developed through usual health promotion activities: health education, skills development, and direct information support⁴⁴; and that empowerment develops along with interactive and critical skills through direct information support.²⁰
All the reviewed interventions used some form of health education. Five used home-based one-to-one, in-person collaborative learning directed by participants rather than by experts or expert-defined curriculum.²⁸ ²⁰ ³³ One relied on an interactive computer program.²⁷ Another involved community members in determining educational content and designing its delivery through in-person group training combined with web-based education and social media reinforcement.³⁴ An important factor differentiates these projects from usual health education: their primary aim was to empower rather than simply to increase knowledge. A qualitative study demonstrated that nearly all women raising children in poverty engaged in self-education by seeking health information online.³⁶
Each of the reviewed intervention studies involved health literacy development along with health education. Roter and colleagues²⁷ focused on interactive skills to increase active participation in prenatal care discussions. Willis and colleagues³⁴ focused on technology skills to increase infant and toddler immunization rates. The home-based interventions aimed to develop functional, interactive and critical skills and the capacity to use them to identify and prioritize problems, set goals, recognize knowledge gaps, seek and evaluate information, build support networks and marshal community resources. In addition, these programs honed parenting skills, along with patient skills such as setting and keeping appointments, maintaining health records, asking questions, and reconciling conflicting information.²⁸ ³⁰ ³³
Distributed health literacy provides informal information support.¹² ¹³ Despite low health literacy, with support to recognize their knowledge gaps and transform information into solutions, mothers were able to overcome barriers to obtain care for themselves and their children.²⁸ ³¹ ³³ ³⁸ ³⁹ Studies considered information support provided in-person, in mothers’ homes by social services providers (n = 4) or public health nurses/case managers (n = 3), in group prenatal care by fellow patients and midwives or physicians (n = 1), computerized information support in community (n = 1), or clinical settings (n = 1); or through social networks (n = 2).
The reviewed studies confirm that empowerment develops along with interactive and critical skills. Intention to empower rather than educate, and a tailored problem-focused collaborative approach, rather than imparting condition-focused facts, may enable mothers to overcome fears and other barriers as indicated by the results of five intervention studies previously mentioned. In those studies, service providers collected and interpreted contextual data to tailor the empowerment process (reflective questioning), which led to personal empowerment of mothers and collective empowerment of service providers.³⁰
Venturelli and colleagues⁴³ sought an explanation for research findings that, compared to women who obtained conventional individual prenatal care, those who participated in group prenatal care had a significantly lower incidence of preterm birth. They concluded that group prenatal care fosters empowerment and maternal health literacy by focusing on group learning, encouraging questions, social support, and connection with a provider.
4.6. QUESTION 6: WHAT SUPPORTS OR IMPEDES IMPROVEMENT OF MATERNAL HEALTH LITERACY AND EMPOWERMENT?
Low health literacy, especially among mothers, is a social risk recognized by poor communities.³⁷ Haynes and colleagues³¹ revealed that mothers visited by nurses who screened for medical conditions and poor child development were significantly less likely to increase their maternal health literacy scores than women in the same community who were also visited by social workers who addressed social determinants of health.
Several studies²⁸ ³⁰ ³⁴ ³⁹ showed that social and instrumental support from home visiting paraprofessionals, social workers or nurse case managers promoted progress toward maternal health literacy and empowered mothers to overcome multiple challenges to maintaining personal and family health. As mothers’ and children’s needs changed, mothers demonstrated new skills while maintaining progress in other areas. Improvement occurred across health literacy domains, showing that maternal health literacy develops over time with need, opportunity, experience, and support.²⁰ Technology skills training, an interactive computer program, and social networks leveraged mothers’ skills and knowledge for health decision making.²⁷ ³⁴ ³⁶ ³⁸ ⁴⁴
Factors impeding mothers’ progress toward maternal health literacy and empowerment include low education; financial problems; poor housing; lack of social support²⁸ ³² ³³ ³⁷; and intimate partner violence.⁴⁰ Unremitting stress, particularly during pregnancy³⁷; lack of computer equipment and skills³⁴ ³⁶; limited access to care due to lack of transportation,³⁰ ³³ insurance,⁴⁰ or childcare²⁸ ³² ³⁹; language barriers²⁸ ³⁹; fear of loss of child custody or privacy; and prior negative experiences in health-care²⁷ ³⁵ were additional barriers. Two studies found, against expectations, that mothers’ depression did not impede maternal health literacy improvement.³² ³³ Reading skills were found to be the least influential of 36 factors positively correlated with maternal health literacy; self-confidence was most influential.²⁸
4.7. QUESTION 7: HOW HAS IMPROVEMENT OF MATERNAL HEALTH LITERACY AND EMPOWERMENT BEEN MEASURED?
No studies in this review measured maternal health literacy and empowerment separately. While measures of empowerment abound, they exhibit a high degree of specificity and lack of validation, similar to health literacy measures.⁴⁵ Many authors used indicators embedded in descriptions and definitions of health- or patient empowerment as indicators of maternal health literacy. Conversely, Smith and Carbone²⁰ inferred increased empowerment from evidence of improved maternal health literacy and identified indicators that have been used to assess both health literacy or critical health literacy, and health- or patient empowerment; notably, self-confidence, autonomy, and behavior change.
5. Conclusion
5.1. SCOPE AND NATURE OF THE LITERATURE
U.S. research on maternal health literacy and empowerment is limited, poorly indexed, and not empirically robust. Twelve studies met selection criteria for this review. Much of the evidence, including studies with “maternal health literacy” in the title, was limited to documenting deficits in functional health literacy or pregnancy-related knowledge among women with specific conditions. Most research focused on functional health literacy in mothers, and on the impact of efforts to simplify information or improve its delivery. We included only publications from the U.S. published in English and accessible online. Relevant articles indexed elsewhere or not accessible online may have been missed.
5.2. KEY RESEARCH FINDINGS
Health literacy and empowerment are closely related. Empowerment is described as both an outcome of maternal health literacy and a process for achieving health literacy.⁴⁶ This review provides some evidence that empowerment develops in tandem with interactive and critical health literacy skills and that improving these skills is feasible, even where functional skills are lacking. Further, more developed individual and distributed maternal health literacy skills can empower socioeconomically disadvantaged mothers to improve health services utilization and engage in preventive practices with benefits that extend to their children, family, and community.
Progress toward maternal health literacy and empowerment was not impeded by limited reading ability or maternal depression. However, it may be impeded by prior negative experience, social determinants of health and other factors. Social determinants of health present specific challenges to maternal health literacy. Direct support to make personal meaning from information and apply it in context may be essential to empowering mothers to obtain the benefits of health education and social services. Support has been provided by social services providers, healthcare professionals, peers, and/or interactive digital programs.
5.3. VALUE OF A GLOBAL SYSTEMATIC REVIEW
Results of this review made clear that a U.S.-centric view of maternal health literacy and empowerment misses a rapidly developing global literature from high-, low- and middle-income countries that has yet to be fully synthesized and evaluated, and that could inform thinking about interventions for U.S. populations, and globally across cultures. Indeed, a recently published bibliometric review noted the multidisciplinary nature and benefits of global Latin American and Caribbean health literacy research.⁴⁷ While measurement and definitional variation make comparison of intervention designs and evaluation less informative, analysis of global findings from community-based participatory research and qualitative studies may aid identification of barriers, facilitators, and meaningful indicators of maternal health literacy and empowerment common across cultures and geography.
Conflict of interest statement:
The authors have no conflicts of interest to declare.
Funding Statement:
This work was funded in part by a Worldwide Universities
References
1. Arksey H, O’Malley L. Scoping studies: Towards a methodological framework. J Int Soc Res. 2005;8(1):19–32.
doi:10.1080/1364557032000119616.
2. United Nations General Assembly. Political declaration of the high-level meeting on the prevention and control of non-communicable diseases: draft resolution September 16, 2011. Accessed October 11, 2024.
https://digitallibrary.un.org/record/710899?ln=en.
3. World Health Organization. Promoting health in the SDGs. Report on the 9th global conference for health promotion, Shanghai, China, November 21–24, 2016: All for health, health for all. Published May 10, 2017. Accessed October 13, 2024. https://www.who.int/publications/i/item/promoting-health-in-the-sdgs.
4. World Health Organization. Health promotion glossary of terms 2021. Accessed October 16, 2024. https://www.who.int/publications/i/item/9789240038349.
5. Renkert S, Nutbeam D. Opportunities to improve maternal health literacy through antenatal education: An exploratory study. Health Promot Int. 2001 Dec 1;16(4):381–8. doi: 10.1093/heapro/16.4.381.
6. Alsop R, Bertelsen M, Holland J. Empowerment in practice: from analysis to implementation. The International Bank for Reconstruction and Development/The World Bank; 2006. Accessed October 14, 2024.
https://openknowledge.worldbank.org/server/api/core/bitstreams/43f6c98e-646c-5caa-bf46-2cae86e82a7c/content.
7. Kickbush I, Maag D. Health literacy. In: Heggenhougen K, Quah S, eds. International Encyclopedia of Public Health. Vol 3. Academic Press; 2008:204-211.
https://www.ilonakickbusch.com/kickbusch-wAssets/docs/kickbusch-maag.pdf. Accessed October 17, 2024.
8. World Health Organization. Standing up for sexual and reproductive health and human rights;
2020. Accessed October 20, 2024.
https://www.who.int/news/item/19-11-2020-who-stands-up-the-right-to-health.
9. DeWalt DA, Hink A. Health literacy and child health outcomes: A systematic review of the literature. Pediatrics. 2009 Nov;124(Suppl 3):S265–74. doi: 10.1542/peds.2009-1162b.
10. Sørensen K, Van den Broucke S, Fullam J, et al. Health literacy and public health: A systematic review and integration of definitions and models. BMC Public Health. 2012 Jan 25;12(80).
https://bmcpublichealth.biomedcentral.com/articles/10.1186/1471-2458-12-80. Accessed October 14, 2024.
11. Nutbeam D. The evolving concept of health literacy. Soc Sci Med. 2008 Dec;67(12):2072–8. https://www.sciencedirect.com/science/article/pii/S0277953608004577. Accessed October 14, 2024.
12. McKinn S, Linh DT, Foster K, McCaffery K. Distributed Health Literacy in the maternal health context in Vietnam. Health Lit Res Pract. 2019;3 (1):e31-e42. doi:10.3928/24748307-20190102-01.
13. Muscat DM, Gessler D, Ayre J, et al. Seeking a deeper understanding of ‘distributed health literacy’: A systematic review. Health Expect. 2022;25(3) :856-868. doi:10.1111/ hex.13450.
14. Wadhwa PD, Buss C, Entringer S, Swanson JM. Developmental origins of health and disease: Brief history of the approach and current focus on epigenetic mechanisms. Semin Reprod Med. 2009; 27(5):358-368. doi:10.1055/s-0029-1237424.
15. Halfon N, Hochstein M. Life course health development: An integrated framework for developing health, policy, and research. Milbank Q. 2002 Sep;80(3):433–79. doi: 10.1111/ 1468-0009.00019.
16. National Research Council and Institute of Medicine Committee on Integrating the Science of Early Childhood Development, Shonkoff JP, Phillips DA, eds. From Neurons to Neighborhoods: The Science of Early Childhood Development. Washington DC: National Academies Press; 2000.
17. Hanson M, Gluckman P, Nutbeam D, Hearn J. Priority actions for the non-communicable disease crisis. Lancet. 2011 Aug;378(9791):566–7. doi.org/10.1016/s0140-6736(11)61286-5.
18. Plianbangchang S. Keynote speech on women’s health and development. Fourth Central Asia Medical Women Association Conference; 2007 June 14-16; Bangkok, Thailand.
http://apps.who.int/iris/bitstream/10665/126437/1/RD-speeches_14JUNE07.pdf. Accessed October 13, 2024.
19. Schillinger D. Social determinants, health literacy, and disparities: Intersections and controversies. Health Lit Res Pract. 2021;5(3):e234-e243. doi:10.3928/24748307-20210712-01.
20. Smith SA, Carbone ET. Reintegrate empowerment and health literacy to advance public health and healthcare delivery. In: Logan RA, Siegel ER, eds. Health Literacy in Clinical Practice and Public Health. IOS Press; 2020:369-399.
21. Peters M, Godfrey C, McInerney P, Soares C, Khalil H, Parker D. The Joanna Briggs Institute Reviewers’ Manual 2015: Methodology for JBI Scoping Reviews. The Joanna Briggs Institute. Adelaide, SA Australia; 2015. Accessed October 14, 2024. https://reben.com.br/revista/wp-content/uploads/2020/10/Scoping.pdf.
22. Harris J, Springett J, Croot L, et al. Can community-based peer support promote health literacy and reduce inequalities? A realist review. Public Health Res. 2015 Feb;3(3):1–192. doi:10.3310/phr03030.
23. United Nations Educational, Scientific, and Cultural Organization (UNESCO) Institute for Statistics Information Paper. Adult and Youth Literacy: National, Regional and Global Trends:1985-2015; 2013. Accessed October 14, 2024.
https://uis.unesco.org/sites/default/files/documents/adult-and-youth-literacy-national-regional-and-global-trends-1985-2015-en_0.pdf.
24. Freire P. Pedagogy of the Oppressed. Bloomsbury Academic; 1970.
25. Sykes S, Wills J, Rowlands G, Popple K. Understanding critical health literacy: A concept analysis. BMC Public Health. 2013 Feb 18;13;150-60. doi: 10.1186/1471-2458-13-150.
26. Colquhoun HL, Levac D, O’Brien KK, et al. Scoping reviews: Time for clarity in definition, methods, and reporting. J Clin Epidemiol. 2014 Dec;67(12):1291–4. doi: 10.1016/j.jclinepi.2014.03.013.
27. Roter DL, Erby LH, Rimal RN, et al. Empowering women’s prenatal communication: Does literacy matter? J Health Commun. 2015;20 Suppl 2(0 2):60-68. doi:10.1080/ 10810730.2015.1080330.
28. Smith SA, Carroll LN. Data-driven maternal health literacy promotion and a postscript on its implications. Stud Health Technol Inform. 2017; 240:144-165.
29. Wollesen L, Peifer K. Life Skills Progression: An Outcome and Intervention Planning Instrument for Use with Families at Risk. Brookes Publishing Company; 2006.
30. Carroll LN, Smith SA, Thomson NR. Parents as Teachers Health Literacy Demonstration project: Integrating an empowerment model of health literacy promotion into home-based parent education. Health Promot Pract. 2015;16(2):282-290. doi:10.1177/1524839914538968.
31. Haynes GW, Neuman D, Hook C, et al. Comparing child and family outcomes between two home visitation programs. FCSRJ. 2015 Feb 13;43(3): 209–28. doi: 10.1111/ fcsr.12098.
32. Smith SA, Moore EJ. Health literacy and depression in the context of home visitation. Matern Child Health J. 2012;16(7):1500-1508. doi:10.1007/s10995-011-0920-8.
33. Mobley SC, Thomas SD, Sutherland DE, Hudgins J, Ange BL, Johnson MH. Maternal health literacy progression among rural perinatal women. Matern Child Health J. 2014;18(8):1881-1892. doi:10.1007/s10995-014-1432-0.
34. Willis E, Gundacker C, Harris M, Mameledzija M. Improving immunization and health literacy through a community-based approach. Stud Health Technol Inform. 2020;269:142-152.
doi:10.3233/SHTI200028.
35. Guy S, Sterling BS, Walker LO, Harrison TC. Mental health literacy and postpartum depression: A qualitative description of views of lower income women. Arch Psychiatr Nurs. 2014;28(4):256-262. doi:10.1016/j.apnu.2014.04.001.
36. Guendelman S, Broderick A, Mio H, Gemmill A, Lindeman D. Listening to communities: Mixed-method study of the engagement of disadvantaged mothers and pregnant women with digital health technologies. JMIR. 2017 Jul 5;19(7):e240. doi: 10.2196/jmir.7736.
37. Salinas-Miranda AA, King LM, Salihu HM, et al. Exploring the life course perspective in maternal and child health through community-based participatory focus groups: Social risks assessment. J Health Dispar Res Pract. 2017;10(1):143-166.
38. Sentell T, Agner J, Pitt R, Davis J, Guo M, McFarlane E. Considering health literacy, health decision making, and health communication in the social networks of vulnerable new mothers in Hawai‘i: A pilot feasibility study. Int J Environ Res Public Health. 2020 Mar 31;17(7):2356. doi: 10.3390/ijerph17072356.
39. Hernandez-Mekonnen R, Duggan EK, Oliveros-Rosen L, et al. Health literacy in unauthorized Mexican immigrant mothers and risk of developmental delay in their children. J Immigr Minor Health. 2016;18(5):1228-1231. doi:10.1007/s10903-015-0284-z.
40. Thomas SD, Mobley SC, Hudgins JL, Sutherland DE, Inglett SB, Ange BL. Conditions and dynamics that impact maternal health literacy among high risk prenatal-interconceptional women. Int J Environ Res Public Health. 2018;15(7):1383. doi:10.3390/ijerph15071383.
41. Gibson CH. A concept analysis of empowerment. J Adv Nurs. 1991;16(3):354-361. doi:10.1111/j.1365-2648.1991.tb01660.x.
42. Lee GV, Barnett BG. Using reflective questioning to promote collaborative dialogue. J
Staff Dev. 1994;15(1):16-21. https://eric.ed.gov/?id=EJ482565. Accessed October 16, 2024.
43. Venturelli N, Kalia I, Reed T, et al. Could group prenatal care work by improving maternal health literacy? Clin Obstet Gynecol Reprod Med. Jan 1 2017;3:1-4. doi:10.15761/COGRM.1000190.
44. Nutbeam D. Health outcomes and health promotion – defining success in health promotion. Health Promot Austr. 1996;6(2):58-60.
https://www.researchgate.net/publication/287376562_Health_outcomes_and_health_promotion_Defining_success_in_health_promotion. Accessed October 16, 2024.
45. Akey TM, Marquis JG, Ross ME. Validation of scores on the Psychological Empowerment Scale: A measure of empowerment for parents of children with a disability. Educ Psychol Meas. 2000;60 (3):419-438. doi:10.1177/00131640021970637.
46. Crondahl K, Karlsson LE. The nexus between health literacy and empowerment: A scoping review. SAGE Open. 2016 May 2;1-7. doi:10.1177/2158244016646410.
47. Paucar-Caceres A, Vílchez-Román C, Quispe-Prieto S. Health literacy concepts, themes, and research trends globally and in Latin America and the Caribbean: A bibliometric review. Int J Environ Res Public Health. 2023;20(22):7084. doi:10.3390/ijerph20227084.