Histological Analysis of Bone Regeneration in Open Healing
A histological analysis of bone regeneration assessing the effects of Open Wound Healing: A case series
Dr. Lanka Mahesh, BDS, MBA, Ph.D 1, Dr. Sagrika Shukla, MDS, Ph.D 2, Dr. Ana Boquete-Castro, DDS, Ph.D 3, Dr. Praful Bali MDS, Ph.D 4, Dr. Nikita Gulati, BDS, MDS 5, Dr. Athreya Rajagopal, MDS, PhD 6
OPEN ACCESS
PUBLISHED: 31 December 2024
CITATION: Mahesh, L., Shukla, S., et al., 2024. A histological analysis of bone regeneration assessing the effects of Open Wound Healing: A case series. Medical Research Archives, [online] 12(12). https://doi.org/10.18103/mra.v12i12.6028
COPYRIGHT: © 2024 European Society of Medicine. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
DOI https://doi.org/10.18103/mra.v12i12.6028
ISSN 2375-1924
Abstract
Aim: To histologically study bone regeneration in cases of open wound healing
Material and method: In a case series of 20 patients, teeth which were fractured/ failed root canal which needed extraction and implant placement were included in the study. In all the cases, minimally invasive tooth extraction was done and care was taken not to damage either of the bony walls. Maxresorb bone graft (Botiss, Germany) was placed in the socket. A single layer of collagen membrane, Ossix plus membrane (Dentsply Sirona, Germany) was placed on the bone graft and 3-0 silk sutures were placed. After 5 months bone core was taken for histological analysis and Mis implant 3.75/11.5 implant was placed at the same site. For histopathology, neutralized buffered formalin solution was used to fix the 2 mm trephine core biopsies and the soft tissue they overlaid right away, lasting between 24 and 48 hours. After which, the normal laboratory approach for tissue processing involving dehydration, cleaning, and paraffin wax infiltration was conducted for both the tissues. Hematoxylin and Eosin stains were used on sections that were 3 microns thick. Van Gieson, Massons trichrome and Picrosirus red were performed.
Results: soft tissue showed long thin rete ridges of parakeratinizd startified suamous epithelium and underlying dense collagenous stroma with few inflammatory cells chiefly lymphocytes. Bony tissue displayed well-formed regions of bony trabeculae with various mineralization phases.
Conclusion: open wound healing leads to bony regeneration as one can predict in closed healing.
Keywords: wound closure, open healing, bone, regeneration, membrane
Introduction:
In literature two types of wound healing have been described, primary healing and secondary healing of wound closure. Primary wound closure is a fundamental surgical principle where edges of the flap are approximated in the same position as they were before the injury/flap reflection, as it creates an undisturbed/unaltered environment from external bacterial or mechanical insult. According to wang et al primary closure of wound is also one of the four principles needed for successful guided bone regeneration. (GBR). Most investigators have also advocated importance of primary closure for predictable GBR, in spite of few clinicians who have disputed its importance, general consensus states that it should be achieved whenever possible. Interestingly, authors also states that clinically sometimes to achieve primary closure is difficult as the approximation has to be without tension, it simply means that any primary flap closure will lead to localized low blood supply followed by increased rate of dehiscence, opening of the sutures and exposure of the underlying membrane.
In a meta-analysis, significant amount of reduced bone formation was observed in case of membrane exposure, in cases of submerged membrane, a mean 3.01 mm of new bone was seen but in cases of membrane exposure an average of only 0.56 mm of new bone was noted. Same authors noted that in guided tissue regeneration (GTR) cases, exposed membranes showed 0.47mm less attachment gain compared to membranes that remained submerged. Another author, Simion et al noted similar results, and reported 99.6% of bone regeneration in submerged membrane cases at the implant site at 6-8 months follow-up as compared to only 48.6% of bone regeneration was found when membrane exposure occurred earlier. Based on aforementioned studies, necessity of primary wound closure can be argued upon, especially when the procedure affects alveolar ridge preservation (ARP) and prognosis of an implant. Many studies have found that primary flap closure may be excluded in ARP. Favourable results in maintaining ridge dimension and vital bone formation were demonstrated in ARP without primary flap closure (i.e. an open‐ healing approach). Based on which, a case series of 20 patients has been discussed, out of which one case has been described, wherein, via histological representation of bone regeneration authors have tried to assess the impact of open wound on regeneration of bone when graft and membrane were placed.
Materials and Methods:
20 patients were included in the study, based on the following inclusion criteria:
- Compliant patient above 20 years of age.
- Patients requiring replacement of missing teeth and willing for implant placement.
- Healthy patients without any/ controlled medical condition.
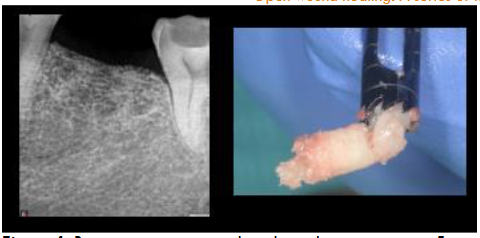
Described here is one case our of 20, wherein a healthy male patient without any medical condition, reported at the dental office with fractured lower mandibular first molar (#36). A treatment plan of socket preservation and implant placement was given to him to which he readily agreed. Minimally invasive tooth extraction was done under local anesthesia and care was taken not to damage either of the bony walls.

After extraction, the socket was not compressed so that the width of the ridge is maintained. Maxresorb bone graft (Botiss, Germany) was placed in the socket.

A single layer of collagen membrane, Ossix plus membrane (Dentsply Sirona, Germany) was placed on the bone graft and 3-0 silk sutures were placed in a manner to hold the tissue and membrane in place however no attempt was made to approximate the open ends of soft tissue. It should also be noted that in such cases achieving primary closure is not possible unless the mucoperiosteum flap is not mobilized.

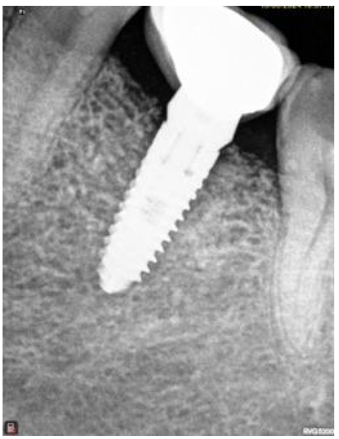
After a period of 5-month showing intraorally and radiographically the site from where bone core using trephine was taken for histological analysis; the same site where implant, Mis implant 3.75/11.5 was placed.

FOR HISTOPATHOLOGY:
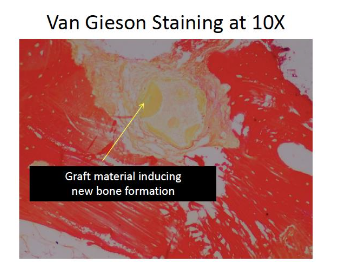
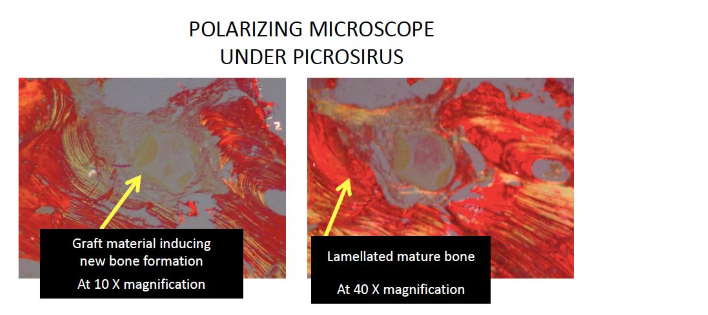
Neutralized buffered formalin solution was used to fix the 2 mm trephine core biopsies and the soft tissue they overlaid right away, lasting between 24 and 48 hours. After being decalcified in a moderate decalcifying agent (10% EDTA, pH 7.4), the hard tissue specimen was processed. The normal laboratory approach for tissue processing involving dehydration, cleaning, and paraffin wax infiltration was conducted for both the tissues. Paraffin wax was used for tissue block preparation and embedding. Hematoxylin and Eosin stains were used on sections that were 3 microns thick. Van Gieson, Massons trichrome and Picrosirus red were performed according to the standard procedure from Bancrofts textbook. The slides were examined using a research microscope (Olympus BX53) and polarizing microscope, with which low- and high-power digital photos were taken (Olympus EPL3).
Results
All sites healed uneventfully. There was no sign of post-operative infection. None of the patients showed any complications post-surgical. Additionally, none of the surgical sites needed additional hard or soft tissue grafting. Upon implant placement, the surgical sites showed appropriate healing as it is seen in any other grafted areas. Furthermore, there was adequate bucco-lingual width of the grafted for Implants placement. Implants placed showed satisfactory primary stability.
Histopathological:
The overlying gingival core shows long thin rete ridges of parakeratinizd startified suamous epithelium and underlying dense collagenous stroma with few inflammatory cells chiefly lymphocytes.
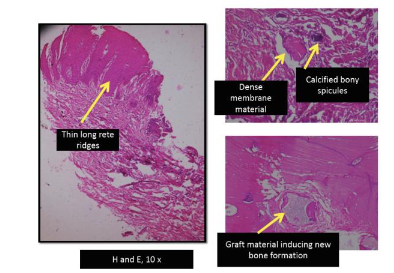
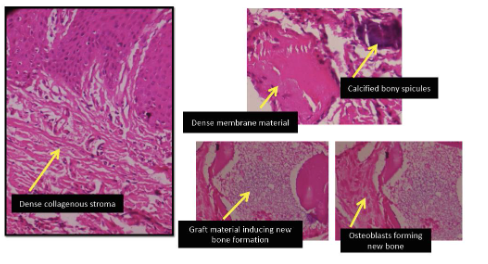
The bone tissue core’s submitted H and E section displays well-formed regions of bony trabeculae with various mineralization phases, figure 7 showing at magnification 10X and figure 8 at 40X magnification. At the graft-new bone interface, immature bony trabeculae with a high number of entrapped osteocytes and lined with osteoblatic rimming and vascular connective tissue are present, focal regions demonstrated the existence of new bone development and areas of remnant graft material. Osteocytes trapped in osteocytic lacunae and bone lining cells on the mature bone exhibit lamellations in majority of the bone core. Few areas also suggest calcification of the remanent graft material.

Discussion:
Bone undergoes lifelong changes of deposition and resorption. Keeping this anatomic consideration into account, in literature many techniques have been used to prevent bone resorption after tooth extraction or implant placement. Yet many methods and surgical techniques await a consensus, such as the surgical protocol, and the biomaterial used. Out of which, type of flap closure required or a necessity of primary closure is still controversial. As aforementioned, primary closure remains a fundamental principal and basic requirement for a predictable GBR, based on which many techniques of mobilising mucoperiosteal flaps have come into existence, some of which are traumatic in nature and difficult to achieve. Recently many authors have shown that predictable GBR can be achieved without primary closure, even when resorbable collagen membranes are left exposed in the oral cavity over the bone graft. Authors like Mardas et al have also shown similar results with the partial exposure of collagen membranes without primary closure after GBR and state good bone regeneration.
This closure of wound is possible due to a biological phenomenon ‘creeping attachment’ of gingiva which was first described by Goldman and Cohen in 1964. Though mostly described in terms of gingival recession, the process simply makes gingival tissues to proliferate covering the defect. However, the prime requisite is maintenance of oral hygiene by the patient so that healing can take place uneventfully. This also emphasises the role of mouthwash for the prevention of surgical site infection. There is enough literature stating advantages of chlorhexidine mouthwash in prevention of surgical site infection and decreasing bacteraemia during dental surgery. In an overview of reviews, and in a systematic review and meta-analysis, authors state that Approximately 12% of bacteraemia cases can be prevented if a population is exposed to chlorhexidine. However, a collagen membrane disintegrates and resorbs faster when exposed to oral cavity and may not be a suitable bio-material in providing stabilization to bone graft material specially a single layered. Hence authors advocate the use of double layered collagen membrane in cases of open healing for GBR. According to authors Kim et al placement of double-layer collagen technique showed a statistically significant benefit in comparison to the single-layer technique for maintaining the stability GBR and bone graft resorption. Nonetheless, no previous report has explored the quantitative effects of single-layer vs. double-layer coverage with resorbable collagen during open-healing ARP. Therefore, the present authors hypothesized that double-layer coverage of collagen membranes would provide better healing results than single-layer coverage for ARP. However, it is interesting to note that open‐ healing approach using a single layer of resorbable membrane is effective even though rapid resorption of the membrane can be expected. Furthermore, no significant difference in ridge dimensional changes could be seen between open‐ healing approaches with double and single layers of the membrane.
In the current study, authors would like to state that the results are consistent with the results of Choi et al. Authors had used a single layer collagen membrane and none of the cases which were included in the study showed any sign of infection, decreased bucco-lingual width of the alveolar process. In none of the cases, no additional hard or soft tissue grafting was required. This can also be attributed to the type of membrane used, OSSIX Plus, which is an ossifying and resilient collagen barrier membrane, developed via GLYMATRIX core technology, it is sugar cross-linked, contributing to improved clinical outcomes. The main advantage is that it is Resistant to degradation when exposed in the oral cavity. Other advantage of open wound healing is the fact that the closure takes place tension-free which does not hamper the blood supply.
Conclusion:
Open wound healing is a good technique to follow provided clinicians use appropriate biomaterials which do not hamper GBR. Having said that, clinician must try to attain primary closure, however in many cases, such as described here, primary closure is not possible, hence alternate technique of healing is used keeping advantages of the Ossix membrane and biology into consideration.
Conflict of interest: None declared.
Funding: None
Acknowledgement: None
Authors’ Contribution
| Author | Conceptualization | Data curation | Formal analysis | Funding acquisition | Investigation | Methodology | Project administration | Resources | Software | Supervision | Validation | Visualization | Writing – original draft | Writing – review & editing |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Dr. Lanka Mahesh | X | X | X | X | X | X | X | |||||||
| Dr. Sagrika Shukla | X | X | X | X | X | X | ||||||||
| Dr. Ana Boquete-Castro | X | X | X | X | ||||||||||
| Dr. Praful Bali | X | X | X | X | X | |||||||||
| Dr. Nikita Gulati | X | X | X | |||||||||||
| Dr. Athreya Rajagopal | X | X | X |
References:
- wang HL. Boyapati L. “PASS” Principles for Predictable Bone Regeneration. Implant Dent 2006;15:8 –17.
- Becker W, Becker BE. Flap designs for minimization of recession adjacent to maxillary anterior implant sites: A clinical study. Int J Oral Maxillofac Implants. 1996;11:46-54.
- Fugazzotto PA. Maintenance of soft tissue closure following guided bone regeneration: Technical considerations and report of 723 cases. J Periodontol 1999;70:1085-1097.
- Goldstein M, Boyan BD, Schwartz Z. The palatal advanced flap: A pedicle flap for primary coverage of immediately placed implants. Clin Oral Implants Res 2002;13:644-650
- Lazzara RJ. Immediate implant placement into extraction sites: Surgical and restorative advantages. Int J Periodontics Restorative Dent. 1989;9:332-343.
- Dahlin C, Lekholm U, Becker W, et al. Treatment of fenestration and dehiscence bone defects around oral implants using the guided tissue regeneration technique: A prospective multicenter study. Int J Oral Maxillofac Implants. 1995;10:312-318.
- Machtei EE. The effect of membrane exposure on the outcome of regenerative procedures in humans: A meta-analysis. J Periodontol. 2001;72:512-516.
- Simion M, Baldoni M, Rossi P, et al. A comparative study of the effectiveness of e-PTFE membranes with and without early exposure during the healing period. Int J Periodontics Restorative Dent. 1994;14:166-180.
- Cho IW, Park JC, Shin HS. A comparison of different compressive forces on graft materials during alveolar ridge preservation. J Periodontal Implant Sci 2017;47:51–63. https://doi.Org/10.5051/jpis.2017.47.1.51
- Cardaropoli D, Tamagnone L, Roffredo A, Gaveglio L, Cardaropoli G. Socket preservation using bovine bone mineral and collagen membrane: A randomized controlled clinical trial with histologic analysis. Int J Perio Restorative Dent 2012;32:421–430.
- Kim DM, De Angelis N, Camelo M, Nevins ML, Schupbach P, Nevins M. Ridge preservation with and without primary wound closure: A case series. Int J Perio Restorative Dent 2013;33:71–78. https://doi.org/10.11607/%20prd.1463
- Mahesh L, Calvo Guirado JL, Shukla S, Kumar VR, Kumar YR. Clinical and radiographic findings without the use of bone substitute materials in extraction sockets and delayed implant placement- A case series. J Oral Biol Craniofac Res. 2020 Apr-Jun;10(2):141-145. Doi:10.1016/j.jobcr.2020.03.011.
- Cardaropoli D, Cardaropoli G. Preservation of the postextraction alveolar ridge: a clinical and histologic study. Int J Periodontics Restorative Dent 2008;28:469-77.
- Araújo MG, Lindhe J. Ridge alterations following tooth extraction with and without flap elevation: an experimental study in the dog. Clin Oral Implants Res 2009;20:545-9.
- Roccuzzo M, Gaudioso L, Bunino M, Dalmasso P. Long-term stability of soft tissues following alveolar ridge preservation: 10-year results of a prospective study around nonsubmerged implants. Int J Periodontics Restorative Dent 2014;34:795-804.
- Mardas N, Chadha V, Donos N. Alveolar ridge preservation with guided bone regeneration and a synthetic bone substitute or a bovine-derived xenograft: a randomized, controlled clinical trial. Clin Oral Implants Res 2010;21:688-98.
- Ekşi C. Two Cases Demonstrating the Role of Creeping Attachment in the Treatment of Keratinized Gingival Deficiency With Free Gingival Graft: A 12-Month Follow-Up. Cureus. 2023 Nov 28;15(11):e49537. Doi:10.7759/cureus.49537.
- Goldman HM, Cohen DW. Periodontal Therapy. 3rd ed. St. Louis: The C. V. Mosby Company; 1964:560.
- Cao Y, Jiang Q, Hu J. Prophylactic therapy for prevention of surgical site infection after extraction of third molar: An overview of reviews. Med Oral Patol Oral Cir Bucal. 2023 Nov 1;28(6):e581-e587. Doi:10.4317/medoral.25999. PMID: 37471296; PMCID: PMC10635635.
- Arteagoitia I, Rodriguez Andrés C, Ramos E. Does chlorhexidine reduce bacteremia following tooth extraction? A systematic review and meta-analysis. PloS One. 2018 Apr 23;13(4):e0195592. Doi:10.1371/journal.pone.0195592.
- Choi HK, Cho HY, Lee SJ, Cho IW, Shin HS, Koo KT, Lim HC, Park JC. Alveolar ridge preservation with an open-healing approach using single-layer or double-layer coverage with collagen membranes. J Periodontal Implant Sci. 2017 Dec;47(6):372-380. Doi:10.5051/jpis.2017.47.6.372.
- Kim SH, Kim DY, Kim KH, Ku Y, Rhyu IC, Lee YM. The efficacy of a double-layer collagen membrane technique for overlaying block grafts in a rabbit calvarium model. Clin Oral Implants Res 2009;20:1124-32.

