Area Postrema Syndrome: Insights from Two Case Reports
Unrelenting Hiccups as a Clue: Area Postrema Syndrome in Medullary Infarct Two Case Reports
Baiakmenlang Synmon 1, Iada Tiewsoh 2, K G Lynrah 3, S R Sharma 4, Mahendra Thakre 5, Hum sheer Sethi 6, Ayush Jain 6,7, Sanchu T K Shreeraj 6,7, Junaid Rashid Dar 6,7
- Baiakmenlang Synmon Associate professor of neurology, NEIGRIHMS
- Iada Tiewsoh Additional professor of Medicine, NEIGRIHMS
- K. G. Lynrah Professor of Medicine, NEIGRIHMS
- S. R. Sharma Professor of neurology, NEIGRIHMS
- Mahendra Thakre Assistant professor of neurology, NEIGRIHMS
- Hum sheer Sethi Senior resident of radiology, NEIGRIHM
- SAyush Jain Senior resident of radiology, NEIGRIHMS; Senior resident of neurology, NEIGRIHMS
- Sanchu T. K. Shreeraj Senior resident of radiology, NEIGRIHMS; Senior resident of neurology, NEIGRIHMS
- Junaid Rashid Dar Senior resident of radiology, NEIGRIHMS; Senior resident of neurology, NEIGRIHMS
OPEN ACCESS
PUBLISHED: 30 June 2025
CITATION: Synmon, B., Tiewsoh, I., et al., 2025. Unrelenting Hiccups as a Clue: Area Postrema Syndrome in Medullary Infarct – Two Case Reports. Medical Research Archives, [online] 13(7). https://doi.org/10.18103/mra.v13i7.6811
DOI https://doi.org/10.18103/mra.v13i7.6811
ISSN 2375-1924
Abstract
Background: The area postrema, a medullary circumventricular organ lacking a blood-brain barrier, plays a key role in autonomic regulation. Ischemic area postrema syndrome (APS) is rare but presents with intractable nausea, vomiting, and hiccups.
Objectives: To highlight ischemic APS through two clinical cases and emphasize diagnostic and therapeutic considerations.
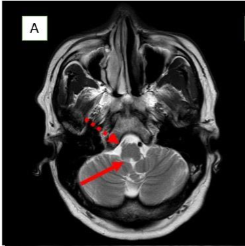
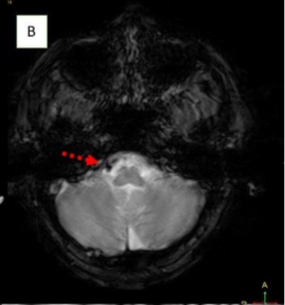
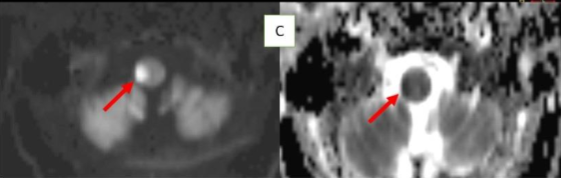
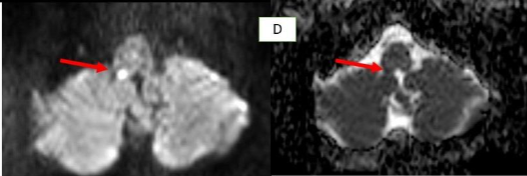
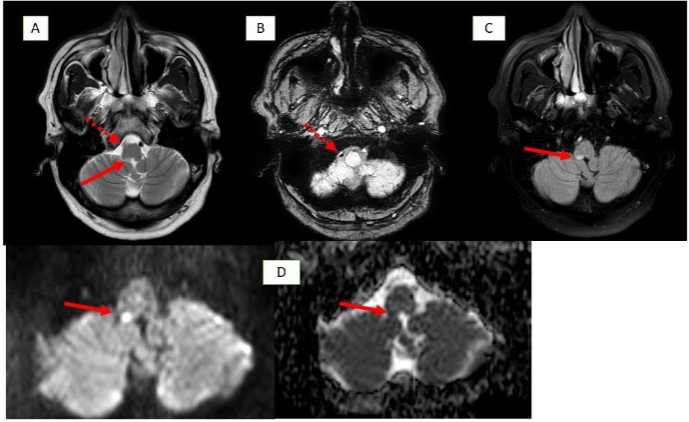
Methods: Two male patients presented with persistent hiccups, nausea, and vomiting. Imaging confirmed lateral medullary infarcts involving the area postrema. Etiological investigations included vascular imaging and thrombophilia workup.
Results: Case 1 had a vertebral artery thrombus and hyperhomocysteinemia. Case 2 showed a similar infarction with protein C and S deficiency. Both were treated conservatively with antiplatelets, vitamins, and symptomatic management, improving clinical outcomes.
Conclusion: Ischemic APS should be considered in stroke differentials with unexplained emetic symptoms. Early recognition and targeted therapy can improve outcomes, particularly in patients with underlying prothrombotic states.
Keywords: Ischemic area postrema syndrome (APS), hiccups, Medullary infarct
Introduction
Area postrema syndrome (APS) typically manifests as persistent nausea, vomiting, and hiccups. The area postrema, located in the medulla oblongata of the brain stem, is a circumventricular organ with permeable capillaries and sensory neurons that detect bloodborne chemical signals and transmit them as neural inputs. Its proximity to the solitary tract nuclei facilitates autonomic functions like vomiting, thirst, hunger, and blood pressure regulation. Located in the fourth ventricle, this vascular structure is rich in AQP4 receptors, and its lack of a blood-brain barrier permits AQP4-IgG entry, potentially signaling early neuromyelitis optica (NMO), a demyelinating disorder.
Ischemic Area Postrema Syndrome (APS) is a rare neurological condition characterized by persistent nausea, vomiting, and hiccups resulting from an infarction in the area postrema, a highly vascularized, circumventricular structure in the dorsal medulla. Supplied by small perforating branches of the anterior spinal artery or vertebral artery, this chemoreceptor “vomiting center” lacks a typical blood–brain barrier, making it uniquely vulnerable to ischemic injury. Although ischemic stroke is an infrequent cause of APS, case reports—highlighting dorsal medullary infarcts confirmed on thin-slice diffusion-weighted MRI—demonstrate that small, localized ischemic events can disrupt the area’s function and induce classic APS symptoms.
We are hereby reporting two cases presenting with APS and ischemia as its aetiology in table 1.
| Parameter | Case 1 | Case 2 |
|---|---|---|
| Age / Sex | 65-year-old male | 53-year-old male |
| Clinical Presentation | Nausea, vomiting, hiccups, giddiness, tinnitus, and unstable gait for 4 days. BP: 200/100 mmHg, Pulse: 70/min. NIHSS score: 0 with equivocal plantar | Sudden-onset neck pain, radiating symptoms, hiccups, nausea, vomiting for 2 days. BP: 180/100 mmHg, Pulse: 90/min. NIHHS -0 with equivocal plantar |
| CT Findings | Lacunar infarcts in the right frontal and parietal lobes, corona radiata, and bilateral external capsules | Diffuse hypodensity in the periventricular region |
| MRI Findings | Acute lateral medullary infarct (right area postrema), loss of normal flow void in right vertebral artery and PICA → intraluminal thrombus | Infarct in lateral medullary area, thrombus in right vertebral artery, T2 hyperintensities in bilateral cerebral hemispheres perpendicular to corpus callosum |
| Other Investigations | Routine and viral marker:-Normal Carotid Doppler: Bilateral atherosclerosis Echocardiography: Mild LVH, mild AR, Grade I diastolic dysfunction, LVEF 60% Stroke panel-Hyperhomocysteinemia (20.7) | Routine and viral marker -Normal CSF: No abnormalities, oligoclonal bands absent Autoimmune workup (AQP4, ANA): Negative Stroke panel: Protein C and S deficiency |
| Treatment | Antiplatelets, anticoagulants, Vitamin therapy Hiccups: Baclofen and chlorpromazine | Antiplatelet therapy, Vitamin supplementation, Hiccups: Baclofen and metoclopramide |
| Outcome | Symptomatic improvement; discharged | Improved with supportive care; discharged with follow-up |
Discussion
The area postrema (AP) in the medulla oblongata triggers the emetic reflex and lacks blood-brain barrier protection, making it sensitive to circulating toxins. Damage from aquaporin-4 antibodies (AQP4-IgG), as seen in neuromyelitis optica spectrum disorder (NMOSD), can cause nausea, vomiting, and hiccups, a triad known as area postrema syndrome (APS). Similar symptoms can occur in autoimmune diseases like SLE.
Vascular causes, including strokes in the posterior circulation (e.g., PICA, vertebral artery), can also lead to APS. These strokes may present with isolated vomiting or the full triad, even when lesions lie just outside the AP, suggesting broader neural involvement. While nausea and vomiting are common in posterior strokes due to vestibular nucleus involvement, hiccups are rarer and often overlooked. Persistent hiccups due to the area postrema infarct is a recognized but poorly understood phenomenon. Several mechanisms have been proposed:
- Neural Plasticity: After injury, maladaptive rewiring in the brainstem, particularly between the AP, nucleus tractus solitarius (NTS), and reticular formation, may disrupt excitatory/inhibitory balance in the hiccup reflex arc.
- Reactive Gliosis: Astrocyte and microglial proliferation form a glial scar that, while protective, may impair synaptic signaling and vagal modulation, contributing to hiccup persistence.
- Loss of Inhibitory Control: Damage to GABA-regulated pathways reduces inhibitory tone over the hiccup central pattern generator. Reduced GABAergic activity post-stroke can enhance reflex excitability and prolong symptoms.
Early recognition of APS is crucial for timely diagnosis. In NMOSD, APS can precede MRI findings, warranting early immunotherapy. In contrast to stroke, APS in NMOSD is driven by autoimmune astrocytopathy, where anti-AQP4 IgG binds to astrocytic water channels in the area postrema, triggering complement activation and resulting in astrocyte loss, immunoglobulin/complement deposition, and inflammatory infiltrates. In a stroke, infarction leads to irreversible damage. Ischemic-stroke-induced Area Postrema Syndrome (APS) results from vascular occlusion—typically of perforating branches from the anterior spinal or vertebral arteries—leading to neuronal ischemia, necrosis, and microglial activation within the dorsal medulla, as demonstrated by diffusion-weighted MRI in case reports.
Clinically, NMOSD-related APS may precede other NMOSD signs, often followed by relapsing demyelinating events, while in stroke-related APS, symptoms are abrupt, typically self-limited, and improve once ischemia resolves or is managed.
Further, Table 2 highlights the rarity of ischemic causes of APS compared to its better-known autoimmune aetiology.
| Author (Year) | Patient Symptoms | Imaging | Outcome | |
|---|---|---|---|---|
| Cohen et al. (2020) | 62M, DM, HTN Abdominal pain, nausea, vomiting, gait issues | Right cerebellar infarct; small AP involvement | Good recovery with metoclopramide + ondansetron | |
| Stancu et al. (2025) | 63F, HTN, DM Sudden nausea, vomiting, hiccups post neck manipulation | Small medullary infarct just above left AP | Resolved with ondansetron; hiccups resolved in 1 week | |
| Schlaeger et al. (2010) | 76F, HTN, DM Acute vomiting | Infarct just above AP; vertebrobasilar stenosis | Not reported | |
| Kim et al. (2003) | 130 patients with lateral medullary stroke | Nausea/vomiting (67), hiccups (33) | Lateral medullary infarction | Not detailed |
Conclusion
These cases highlight the importance of recognizing APS as a clinical manifestation of medullary infarction. A high index of suspicion and prompt imaging studies are crucial for early diagnosis and management. Symptomatic relief of intractable hiccups can improve patient comfort and outcomes. Further research is warranted to explore the underlying mechanisms and optimize treatment strategies for APS in stroke patients.
Bibliography
- Mirza M, Das JM. Neuroanatomy, area postrema. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 [cited 2019 Dec 4]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK539823/
- McKinley MJ, Denton DA, Ryan PJ, Yao ST, Stefanidis A, Oldfield BJ. From sensory circumventricular organs to cerebral cortex: Neural pathways controlling thirst and hunger. J Neuroendocrinol. 2019;31(3):e12689.
- Sarnat HB, Flores-Sarnat L, Boltshauser E. Area postrema: fetal maturation, tumors, vomiting center, growth, role in neuromyelitis optica. Pediatr Neurol. 2019;94:21–31.
- Kremer L, Mealy M, Jacob A, et al. Brainstem manifestations in neuromyelitis optica: a multicenter study of 258 patients. Mult Scler. 2014;20(7):843–7.
- Cohen DT, Craven C, Bragin I. Ischemic stroke induced area postrema syndrome with intractable nausea, vomiting, and hiccups. Cureus. 2020 Jun 15;12(6):e8630.
- Wang TJ, Lee NY, Young RJ. An unusual cause of isolated vomiting. Neurology. 2012 Jan 3;78(1):72-3. doi: 10.1212/WNL.0b013e3182420613. PMID: 22201113.
- MacDougall MR, Sharma S. Physiology, chemoreceptor trigger zone. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020
- Shosha E, Dubey D, Palace J, et al. Area postrema syndrome: frequency, criteria, and severity in AQP4-IgG-positive NMOSD. Neurology. 2018;91:e1642–51.
- Vassallo J. Area postrema syndrome secondary to lupus neuroinflammation. J Pediatr Ophthalmol Strabismus. 2019;56(5):340.
- Mortazavi MM, Tubbs RS, Harmon D, Oakes WJ. Chronic emesis due to compression of the area postrema by the posterior inferior cerebellar artery: resolution following microvascular decompression. J Neurosurg Pediatr. 2010;6(6):583–5.
- Stancu P, Sanda N, Lovblad KO, Guinand N, Kleinschmidt A, Escribano Paredes JB. Area postrema syndrome as the only sign of medullary infarction adjacent to area postrema. eNeurologicalSci. 2025;100563.
- Tao WD, Liu M, Fisher M, Wang DR, Li J, Furie KL, et al. Posterior versus anterior circulation infarction: how different are the neurological deficits? Stroke. 2012;43(8):2060–5.
- Misu, T.; Fujihara, K.; Kakita, A.; Konno, H.; Nakamura, M.; Watanabe, S.; Takahashi, T.; Nakashima, I.; Takahashi, H.; Itoyama, Y. Loss of aquaporin 4 in lesions of neuromyelitis optica: Distinction from multiple sclerosis. Brain 2007, 130, 1224–1234
- Papadopoulos MC, Verkman AS. Aquaporin 4 and neuromyelitis optica. Lancet Neurol. 2012 Jun;11(6):535-44. doi: 10.1016/S1474-4422(12)70133-3.
- Jarius S, et al. Mechanisms of disease: aquaporin-4 antibodies in neuromyelitis optica. Nat Clin Pract Neurol. 2008;4:202–214. doi:10.1038/ncpneuro0764
- Ratelade J, Bennett JL, Verkman AS (2011) Intravenous neuromyelitis optica autoantibody in mice targets aquaporin‐4 in peripheral organs and area postrema. PLoS ONE 6:e27412.
- Carnero Contentti, E., Correale, J. Neuromyelitis optica spectrum disorders: from pathophysiology to therapeutic strategies. J Neuroinflammation 18, 208 (2021). https://doi.org/10.1186/s12974-021-02249-1
- Tatjana Vlašković et al Anatomic and MRI bases for medullary infarctions with patients’ presentation Journal of Stroke & Cerebrovascular Disease , Volume 31, Issue 10106730October 2022
- Lekic T, Zhang JH. Posterior circulation stroke and animal models. Front Biosci. 2008 Jan 1;13(13):1827-44.
- Schlaeger R, Sollberger M. An unusual cause of isolated vomiting. Neurology. 2010 Oct 5;75(14):1303.
- Kim JS. Pure lateral medullary infarction: clinical-radiological correlation of 130 acute, consecutive patients. Brain. 2003 Aug;126(Pt 8):1864-72.
- Huang L, Wu ZB, Zhuge Q, Zheng W, Shao B, Wang B, Sun F, Jin K. Glial scar formation occurs in the human brain after ischemic stroke. Int J Med Sci. 2014 Feb 11;11(4):344-8. doi: 10.7150/ijms.8140.
- Oshima T, Sakamoto M, Tatsuta H, Arita H. GABAergic inhibition of hiccup-like reflex induced by electrical stimulation in medulla of cats. Neurosci Res. 1998 Apr;30(4):287-93.

