Home > Medical Research Archives > Issue 149 > The John F. Kennedy X-rays: The saga of the largest "Metallic fragment"
Published in the Medical Research Archives
March 2023 Issue
The John F. Kennedy X-rays: The saga of the largest "Metallic fragment"
Published on June 17, 2015
DOI
Abstract
Purpose—To solve the mystery of the 6.5 mm “metallic” object on President John F. Kennedy’s anterior-posterior (AP) skull X-ray. This image was not seen or reported during the official autopsy on November 22, 1963, but first appeared in the historical record in 1968 with the release of the Clark Panel Report.
Methods—On nine separate days, once with Dr. Cyril Wecht (former president of the American Academy of Forensic Science), I examined the John F. Kennedy (JFK) artifacts at the National Archives. Hundreds of optical density measurements were made from the (supposed) original skull X-rays, with a specific focus on the 6.5 mm object that lies within JFK’s right orbit on the AP skull X-ray.
Results—This essay explains (and demonstrates) how X-ray alteration was feasible in 1963, and identifies a candidate for this darkroom work. Hundreds of optical density data points (presented in graphical form here) expose the paradoxes of this 6.5 mm image. In addition, the phantom image (of an authentic bullet fragment), seen inside the 6.5 object, is consistent with a double exposure in the X-ray darkroom.
Discussion/Conclusion—This mysterious 6.5 mm image was (secretly) added to the original X-ray via a second exposure. The alteration of the AP X-ray was likely completed shortly after the autopsy. Its proximate purpose was to implicate Lee Harvey Oswald and his supposed 6.5 mm Mannlicher-Carcano carbine, to the exclusion of any other suspect, and thereby to rule out a possible conspiracy. The ultimate purpose for such a forgery is left to the historians.
Author info
Introduction
Methods
Study Location
The study was conducted at Likuni Mission Hospital in Lilongwe, the capital city of Malawi. The hospital is located in the central region of Malawi. It is affiliated with the Christian Health Association of Malawi (CHAM). This hospital was chosen in consideration of the wide coverage of the people it saves, both urban and peri-urban. It is also one of the institutions in Malawi with proper documentation of patient and clinical data as compared to most government and other private hospitals.
Study design and population
The study was a retrospective cross-sectional survey, of the clinical and social-economic profiles of patients previously diagnosed with COVID-19 at Likuni mission hospital in Lilongwe, Malawi, between January 2021 to January 2022. It involved examination of all records of patients diagnosed with COVID-19 at the mission hospital in the stated period. After clearly examining the records, the clinical presentations, socio-economic data and the covid-19 status were extracted and anonymized with a unique study number to delink it from the patients studied. The retrospective analysis included all patients who tested positive for COVID-19 using DNA PCR as well as rapid test. All patient files that had missing information such as clinical profiles, names and dates of diagnosis were excluded from the study.
Data collection
The Medical records’ data was extracted and stored in a password protected computer. The extracted data included the following, demographic characteristics (age, sex, residence location and occupation), clinical presentation and patient comorbidities. The age was categorized into three strata’s, (<40, >40-<60, >60) The primary outcomes of the study were hospital admission, and mortality. Occupation and area of residence was used as proxy to estimate the social economic status of the studied patients.
Statistical analysis.
The clinical characteristics of COVID-19 positive patient were stratified into patients with comorbidities and those without comorbidities, and
also across various social economic status using twosided t-test for age, and chi-squared test for categorical variables. Categorical measures were presented as percentages and continuous measures were presented as means and standard deviations. The association between age, comorbidity and hospitalization was assessed using unadjusted and adjusted logistic regression models. Results are presented as percentages.
Results
Characteristics of COVID-19 patients.
There was a total of 496 COVID-19 positive patients who were enrolled. The mean age of the patients included in our final study population was 35 with a mode and median of 24 and 32 respectively. The study population was predominantly female (65%, n= 317). In this study,
COVID 19 was also seen more among the group aged less than 40 (67.8%), and predominantly among youth. Table 1; summarizes characteristics of the patients. 108 (22%) cases were among the group aged 40-60 and only 50 (10.2%) affected people aged 60 and above.
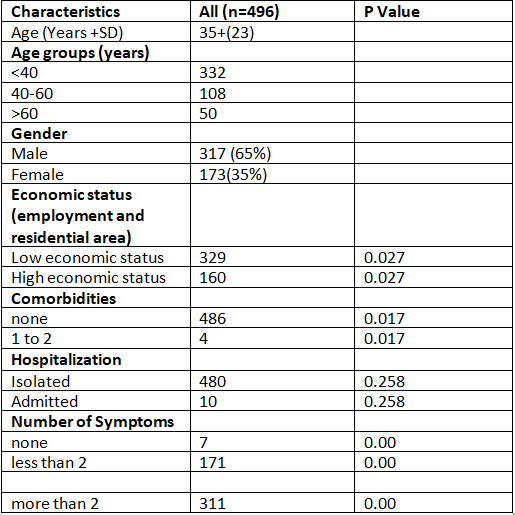
Table 1. Clinical characteristics and outcomes of patient’s diagnosis with COVID-19
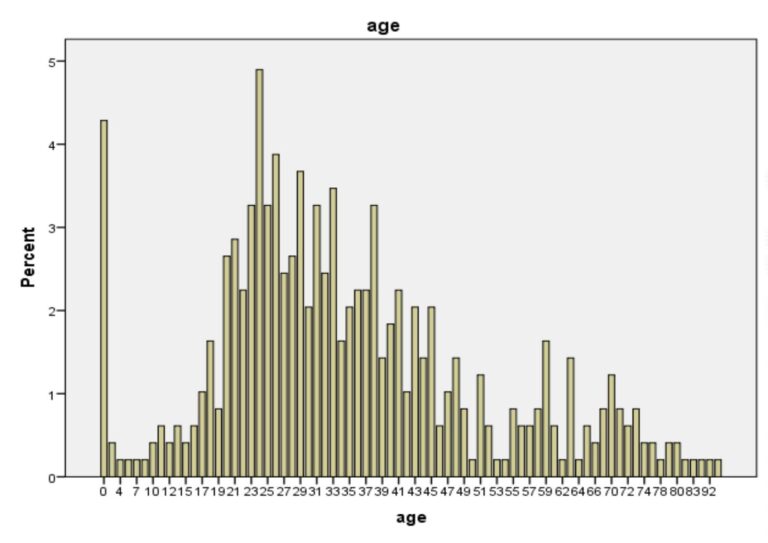
Figure 1: Histogram of COVID-19 patients across various age groups.
Clinical presentation and comorbidity
Most of the patients presented with more than 3 symptoms most of which were fever, cough, chest pains, headache, shortness of breath, and general body weakness. In addition, some patients presented with anosmia, sore throat; vomiting, chills, diarrhoea, loss of appetite, and joint pains. The majority of our patients didn’t have any comorbidity indicated in the clinical notes. Only 2 patients had known diagnosis of hypertension and another two were known asthmatic patients.
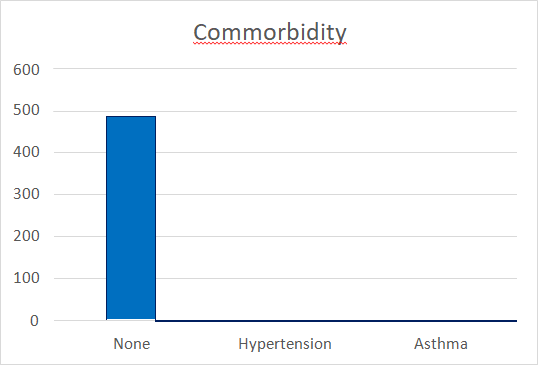
Figure 2. Patient distribution by comorbidity.
Social economic status based on employment status and area of residence
In our study, most of the people that were COVID-19 positive were from low social economic status (329 of 496), representing 67% of the total population. This result was statistically significant (P=0.0258)
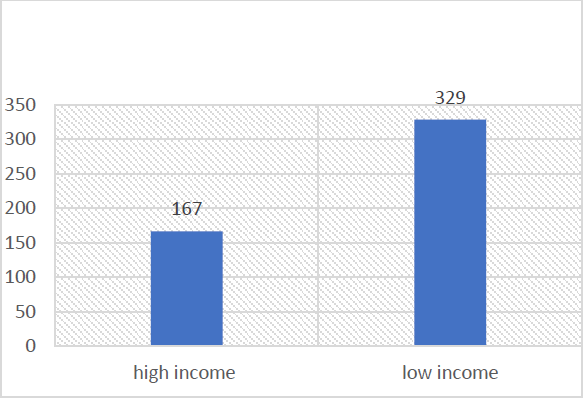
Figure 3: Patient distribution by economic status based on area of residence and occupation
Travel and Contact history
There was no record of recent foreign travel to for all our cases. Only 25 ((5.1%) of 490 patients reported being contact with a patient with a previously confirmed COVID-19. Majority of the patients (87%) did not have any documented positive contact history. They were all reported as index cases.
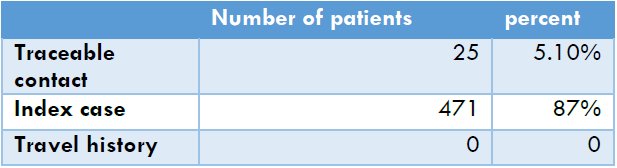
Table 2: Distribution of patient according to contact and travel history.
Isolation versus Admitted
Majority of our patient required no hospitalization (98%, 480 of 490), while only 2 percent suffered a severe disease and required hospitalization, (10 of 480).
Age versus Admission
There was a close association between advanced age and being admitted at the hospital. Almost all patients that were admitted were about the age of 60 and the results were statistically significant (p= < 0.001). All patient that suffered a severe disease survived and were discharged from the hospital.
Discussion
In our retrospective cross-sectional survey of COVID-19 patients at Likuni mission hospital. majority of our patients were females (67%). The
typical clinical presentations were fever, cough, chest pains, headache, shortness of breath, and general body weakness. Even though the COVID-19 pandemic had varying clinical picture across various regions, most of the symptoms were similar. The finding from this study, are also reflected in other studies done across the world.15 The similarity in clinical presentation has a huge significance to public health information, prevention and control of the disease. Whilst the clinical presentation was similar to studies done in other settings, there were huge differences in demographic characteristics such as age. Our population was predominantly younger, with a mean age of 35. This reflects the demographic variations that exist across various nation.
Most of developing countries, including Malawi, have predominantly younger population16. Nearly half of the population is below the age of 50, and majority of them are youth16. This demographic variation, explains why most of the people affected were in their 20’s. This is also the group that has high level of social mobility and interactions, leading to higher rate of positive contacts and increased rate of spread of the disease.
While clinical comorbidities such as diabetes, hypertension, dyslipidemias and chronic lung conditions have clearly been documented to affect the outcomes of patients, diagnosed with COVID-19, in this present study, it did not appear as a major factor. Contrary to the findings in studies done across Europe and Asia, where the prevalence of comorbidity amongst patients diagnosed with COVID-19 was as high as 50%15, our present study demonstrated very low percentage of patients who had comorbidities. Only 2% (n=4) had known diagnosed hypertension and asthma. This may reflect limitations in diagnostic capability across various developing countries. While WHO recommends screening for non-communicable diseases in routine practice, most developing countries lack diagnostic capacity and have
inadequate human resource to cater for integrated disease. It is an undisputable fact, that there is an epidemiological transition in Africa. Most countries are suffering from dual burden of NCDs and infectious diseases and Malawi is not an exception.17 The prevalence of non-communicable diseases has been increasing in Malawi, with hypertensive disorders being the predominant disease18.
Despite that being the case, many people still live with chronic conditions, but they are largely unaware of it due to poor health seeking behaviour and limited screening for comorbidities during routine care. This could partially explain the low levels of comorbidity among our patients. There is also a strong link between age and development of chronic conditions. Advanced age has been closely associated with increased risk of developing chronic conditions such as hypertension and atherosclerotic disorders18. The predominantly younger population could have led to low levels of comorbidity among our patients as compared to studies done in other regions, which the population is predominantly aged. This demographic variation plays a significant role in the differences in comorbidities seen across the world.
In our study we also observed that most of the patient presented with more than 3 symptoms but did not suffer a severe disease that needed hospitalization. Most of them self-reported to the hospital and were sent to self-isolation as they didn’t require advanced respiratory support. Only 10 out of 490 required hospitalizations, and all were above the age of 60. There was a closer association between advanced age and needing hospitalization and the results were statically significant. Unlike in studies done in other settings, nearly all our patients survived and were discharged from the hospital without need of follow up. This is contrary to the findings in other settings,
where all-cause mortality was particularly high probably owing to the advanced patient age and high prevalence of comorbid conditions15.
67% percent of our population lived in suburbs and depended on piece works for day to living. The population was predominantly of low socioeconomic status and lived in overcrowded areas. These areas had high COVID-19 transmission rates, but fortunately the case fatality rate was extremely low. Our findings also agree with studies done across the country, where densely populated areas had high transmission rates and most people barely lived below the poverty level. Also, studies done in other countries, demonstrated that people from low social economic status, were more likely to be affected from the disease15. Adherence to COVID- 19 preventive measures requires access to safe and clean water, and other preventive equipment such as mask. Most people in low socio-economic status don’t have access to these items. This led to challenges in adherence to COVI-19 preventive measures and increased spread of the disease. Our results clearly demonstrates that various disparities exist among patients diagnosed with COVID-19. The differences in socio-demographic
profiles between different regions of the world, has read to different patterns of the disease as it is clearly demonstrated in this study. While most of our patients were young and didn’t have any comorbidity, the situation was so different in other parts of the world. This, therefore calls for localized policies and guidelines across various regions to mitigate the spread of the disease.
Conclusion
In urban Malawian hospital, fever, cough, chest pains, headache, shortness of breath, and general body weakness were the most common clinical presentation of the patients diagnosed with COVID-19. Females were more susceptible to the disease as compared to males, and the disease predominantly affect the younger population. Advanced age is a risk factor for severe disease requiring hospitalization. Transmission of the disease is concluded to be more by virtue of local spread as compared to travel to other countries. Majority of the people affected with the disease in the study, recovered without requiring hospital admission or advanced respiratory support. Being of low social economic status, wasn’t seen as an independent risk factor for the COVID-19 disease. All cases didn’t have recent travel history from another country.
Declarations
Ethics approval and consent to participate
The study was approved by the College of Medicine Research and Ethics Committee (COMREC) before the commencement of data collection (U.06/22/3660). Permission to conduct the study was provided by the Admistrator of Likuni mission hospital. The study didn’t involve direct contact with the patients, so there was no need to get informed consent from the patients. However, data was handled in accordance with the principles of confidentiality. All the records were de-identified and stored on a password-protected computer. Hard-copy records were stored in a locked filing cabinet.
Consent for publication
Written consent for the study participation and potential publication of results was sought from Likuni hospital before commencement of data collection.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author upon reasonable request.
Conflict of interest
The authors have no conflicts of interest to declare.
Funding
This study was partly funded by Clinical Research, Education and Management Services Ltd (CREAMS) under the student training package. The funding only covered processing ethics committee processing fee and data collection expenditure, and the total funding amounted to 350 US dollars.
Author Contribution
AFL: Concept and design of the study, prepared first draft of the Manuscript, Interpreted result and literature review. AL: Data analysis, Literature review. DN: Data collection, GKK: Data Collection, VM: project supervision, GMP, LMN and EM: Provided factual-check from Christian Health Association of Malawi. TN: Concept suggestion, project supervision and final manuscript editing
Acknowledgement
We would like to acknowledge CREAMS for their support toward the project and also Likuni mission hospital for authorising us to conduct a study in their hospital.
References
- Adams J, Mackenzie MJ, Amegah AK, et al. The conundrum of low COVID-19 mortality burden in sub-Saharan Africa: myth or reality? Glob Health Sci Pract. 2021;9(3):433-443.
- World health organization, (2022, January 17). A report about Coronavirus. Retrieved from https://covid19.who.int/
- African Union, African CDC, Africa Identifies First Case of Coronavirus Disease: Statement by the Director of Africa CD0C. Retrieved from https://africacdc.org/news- item/africaidentifies- first-case-of-coronavirus-diseasestatement- by-the-director-of-africa-cdc/
- African renewal, (December, 2016-March 2017). Health care systems: Time for a rethink. Retrieved from; https://www.un.org/africarenewal/
- D Maher, L Smeeth & J Sekajugo. Health transition in Africa: practical policy proposals for primary care. Bull World Health Organ. 2010 Dec 1;88(12):943-8.
- Chibwana MG, Jere KC, Kamng R, Mandolo J, Katunga-Phiri V, Tembo D, … Jambo KC. High SARS-CoV-2 seroprevalence in health care
workers but relatively low numbers of deaths in urban Malawi [version 1; peer review: awaiting peer review]. Wellcome Open Research
2020;5(199):1-8. doi: - World meters. Corona virus in Malawi. https://www.worldometers.info/coronavirus/c ountry/malawi/. Access, January 17, 2022.
- United nation development program (UNDP). Study on Socio-economic impact of Covid-19 pandemic in Malawi. Retrieved from; https://www.mw.undp.org/content/malawi/en /home/library/studv-on-socio-economicimpact- of-covid-19-pandemic-in-malawi-.html
- UNICEF Malawi. Health budget brief 2020; Improving Public Investments in the Health Sector in the context of COVID-19. Accessed
from https://www.google.com/url?sa=t&rct=i&q= &esrc=s&source=web&cd=&ved=2ahUKEwj8 zOHEprv1AhVRi0HHXRiBiEQFnoECAQQAQ&u rl=https%3A%2F%2Fwww.unicef.org%2Fesa %2Fmedia%2F8991%2Ffile%2FUNICEFMalawi- 2020-2021-Health-Budget- Brief.pdf&usg=AOvVaw1uAwEzZwrbie8mzzl UYSXM - International Monetory fund report (29, May 2017). Malawi economic development. Accessed from: https://www.google.com/url?sa=t&rct=i&q= &esrc=s&source=web&cd=&cad=ria&uact=8 &ved=2ahUKEwiepbrLp7v1 AhWL7rsIHQH1BiY QFnoECAcQAw&url=https%3 A%2F%2Fwww.imf.org%2F~%2Fmedia%2FFi les%2FPublications%2R%2F2017%2Fcr1 7184.ashx&usg=AOvVaw1slJi4Sfd4x4cfnDIFf qwo
- The Ministry of health, Government of Malawi; Health sector strategic plan II. Accessed from https://www.google.com/url?sa=t&rct=i&q= &esrc=s&source=web&cd=&cad=ria&uact=8 &ved=2ahUKEwiBquHrqLv1AhUrh 0HHZ1- C0QFnoECAUQAQ&url=https%3A%2F%2Fw ww.healthdatacollaborative.org%2Ffileadmin %2Fuploads%2Fhdc%2FDocuments%2FCountr y documents%2FHSSP II FinalHQ complete =File.pdf.pdf&usg=AOvVawQfgakr1q15t9Bk RriAened.
- Jethro Banda et al. Knowledge, risk perceptions, and behaviours related to the COVID-19 pandemic in Malawi.
https://www.demographicresearch.org/Volumes/Vol44/20/ DOI: 10.4054/DemRes.2021.44.20 - Master R.O. Chisale, Billy W. Nyambalo, Collins Mitambo et.al. Comparative characterization of COVID-19 patients with hypertension
comorbidity in Malawi: a 1:2 matched retrospective case-control study. - Irawaty DJaharuddin Sitti Munawwarah et al. Comorbidities and mortality in COVID-19 patients.
- Siva Prasad Reddy Basava, Aruna Rani Behera, Sangeeta Panigrahy, Pradeep Vegi, Samatha P, Balachandrasekhar P, & Sai Saileshkumar Goothy. (2022). Socioeconomic, demographic, and clinical profile of COVID patients in north coastal districts of Andhra Pradesh. Asian Journal of Medical Sciences, 13(8), 1–7. https://doi.org/10.3126/ajms.v13i8.43950
- Malawi National statistical office; Malawi Fifth Integrated Household Survey (IHS5) 2019- 2020; Accessed from; https://microdata.worldbank.org/index.php/c atalog/3818/download/49047
- Islam, S.M.S., Purnat, T.D., Phuong, N.T.A. et al. Non‐Communicable Diseases (NCDs) in developing countries: a symposium report.
Global Health 10, 81 (2014). https://doi.org/10.1186/s12992-014-0081- 9. - Msyamboza KP, Kathyola D, Dzowela T, Bowie C. The burden of hypertension and its risk factors in Malawi: nationwide population based STEPS survey. Int Health. 2012 Dec;4(4):246-52. doi: 10.1016/j.inhe.2012.09.005. PMID: 24029670.
Author Area
Have an article to submit?
Submission Guidelines
Submit a manuscript
Become a member



