Beer Protocol for Recurrent Pregnancy Failure Success
The Beer Treatment Protocol for Recurrent Pregnancy Failure: A Retrospective Cohort Analysis
Raphael B. Stricker, MD1, Melissa C. Fesler, DNP, RN, FNP-BC, PHN1
- Alan E. Beer Medical Center for Reproductive Immunology
OPEN ACCESS
PUBLISHED: 30 November 2025
CITATION: Stricker, R.B. and Fesler, M.C., 2025. The Beer Treatment Protocol for Recurrent Pregnancy Failure: A Retrospective Cohort Analysis. Medical Research Archives, [online] 13(11). https://doi.org/10.18103/mra.v13i11.7117
COPYRIGHT: © 2025 European Society of Medicine. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
DOI https://doi.org/10.18103/mra.v13i11.7117
ISSN 2375-1924
ABSTRACT
Background: Over the past 15 years we have learned much about recurrent pregnancy loss (RPL) and recurrent implantation failure (RIF) in otherwise healthy women. These women repeatedly fail to achieve successful pregnancy even when high-grade embryos are produced following in vitro fertilization. We have performed a retrospective cohort analysis to determine whether a careful clinical history, specific laboratory testing and targeted treatment can achieve pregnancy success in these women.
Methods: From 2007-2022, we collected data from 1,414 RPL/RIF patients who were evaluated according to the Beer treatment protocol. The Beer protocol uses a multivariate evaluation tool to identify immunological, metabolic and coagulation abnormalities that contribute to RPL and RIF. We examined 13 factors that may interfere with pregnancy, and we tailored our treatment to address these factors.
Results: The mean patient age was 37.8 ± 4.9 years and the mean number of pregnancy failures was 4.0 ± 2.6. The pregnancy success rate with the Beer protocol was 70% overall and even higher when egg quality issues were eliminated. Women who were age matched and untreated served as historical controls, and their pregnancy success rate was 23%. The difference in pregnancy success between treated versus untreated women was significant (P=0.0001).
Conclusion: The Beer treatment protocol for RPL/RIF was associated with significant pregnancy success in this cohort. Future approaches to improve pregnancy outcomes in women with RPL and RIF warrant investigation.
Keywords
Recurrent Pregnancy Loss, Recurrent Implantation Failure, Beer Treatment Protocol, Immunological Abnormalities, Metabolic Abnormalities, Coagulation Abnormalities
Introduction
Recurrent pregnancy failure, which encompasses recurrent pregnancy loss (RPL) and recurrent implantation failure (RIF), has increased significantly in recent years. As women delay childbearing in Western societies, the increase in RPL/RIF mirrors increasing age in these women. By the time women reach the age of 45 years about three-quarters will miscarry. Although in vitro fertilization (IVF) has been proposed as a way to address this problem, the success rate with IVF in older women decreases, with live birth rates in the 10-20% range for women older than 40 years of age. RPL and RIF are really two sides of the same coin. Both problems occur in similar age groups with similar histories of pregnancy failure and similar immunological, metabolic and coagulation abnormalities, as described below.
This article provides a retrospective cohort analysis of RPL/RIF diagnosis and treatment based on the seminal work of Alan E. Beer, MD, founder of the Alan E. Beer Medical Center for Reproductive Immunology in Los Gatos, CA. Dr. Beer was a pioneer and an innovator up until his untimely death in 2006.
Background
IMMUNOLOGICAL ABNORMALITIES
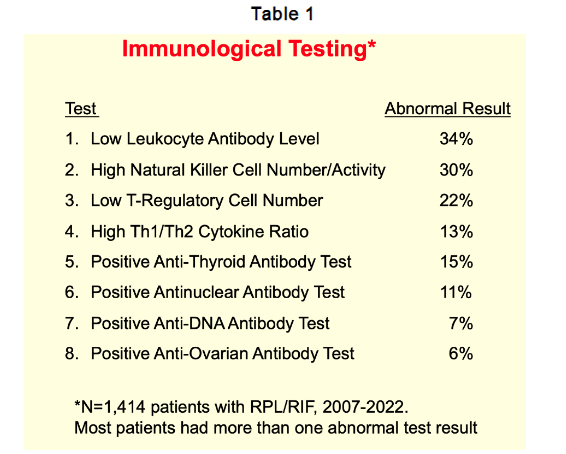
Diagnostic testing has been developed for the most significant immunological abnormalities related to pregnancy, as shown in Table 1. These abnormalities include: (a) low leukocyte antibody levels; (b) high natural killer cell number and activity; (c) low regulatory T-cell numbers (T-reg cells); (d) high TH1/TH2 cytokine ratios; and (e) various autoantibodies that are associated with recurrent pregnancy failure. These findings are based on a cohort of 1,414 patients with RPL/RIF who were screened at the Beer Center over 15 years. A majority of this cohort was found to have more than one abnormal test result.
For leukocyte antibody detection, we measure maternal anti-lymphocyte antibodies to paternal HLA antigens. These are IgG antibodies directed against T cells and B cells, or so-called blocking antibodies that protect the fetus against the mother’s immune system, and these antibodies are detected using flow cytometry. Maternal natural killer (NK) cells are extremely important in pregnancy, and there is a spectrum of normal numbers of CD56 NK cells and normal NK cell activity in successful pregnancy versus high numbers of CD56 NK cells and increased NK cell activity in pregnancy failure.
As their name implies, T-reg cells are responsible for regulating the immune response and play a significant role in RPL/RIF. Winger and Reed noted that the pregnancy success rate was 80% with normal T-reg cells but the success rate dropped to 44% in women with low T-reg cells. Cytokines are immune factors that are also involved in regulating the immune response, including inflammation. The TH1/TH2 cytokine balance is important for pregnancy success, with predominant TH1 cytokines associated with pregnancy failure and predominant TH2 cytokines associated with pregnancy success. Among TH1 cytokines, an increased tumor necrosis factor (TNF) level is the most significant cytokine alteration associated with pregnancy failure. TNF is a pro-inflammatory cytokine that naturally increases with age and pregnancy, and excess TNF production is associated with RPL/RIF.
METABOLIC ABNORMALITIES
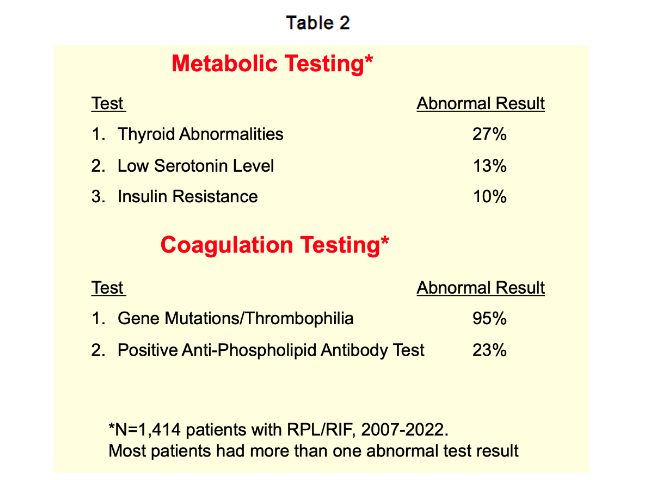
Metabolic abnormalities are important in RPL/RIF, including low thyroid function, low serum serotonin level and insulin resistance. In terms of thyroid disease and pregnancy failure it is well known that the thyroid regulates both fertility and pregnancy outcomes. Serotonin is a key signaling molecule in embryogenesis and the hormone is involved in placental nutrient acquisition and metabolism. In terms of insulin resistance, women who have this metabolic problem have three times the number of miscarriages compared to women who do not.
COAGULATION ABNORMALITIES
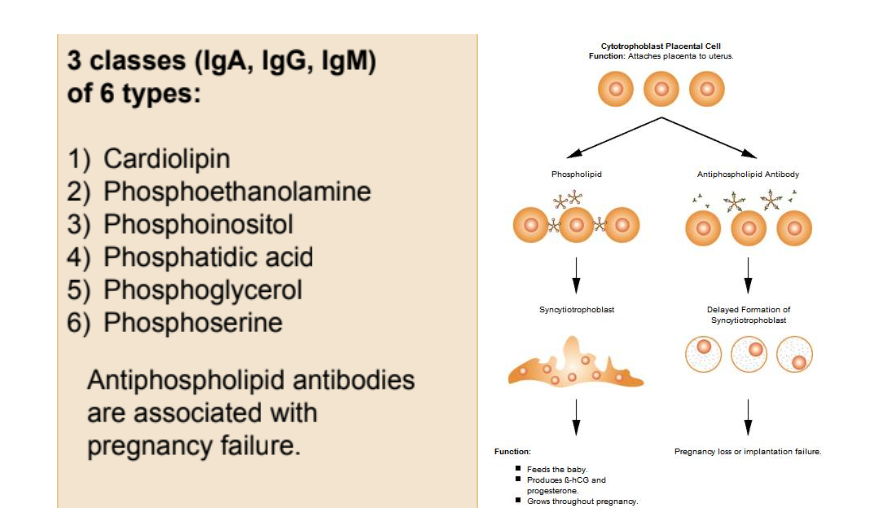
Coagulation abnormalities occur in women with gene mutations associated with inherited thrombophilia. We routinely test for MTHFR, PAI-1, Factor XIII, Factor V Leiden and Prothrombin gene mutations. We consider both homozygous and heterozygous mutations to be significant according to the most recent literature showing that even heterozygous mutations play a role in RPL/RIF. Anti-phospholipid antibodies (APA) are also associated with excess blood clotting. We measure three classes of these antibodies (IgG, IgA and IgM) and six types of APA. APA are associated with delayed formation of the syncytiotrophoblast, resulting in RPL and/or RIF. We consider any of these forms of APA to be significant, and it is important to go beyond the simple screening test for these antibodies and test for individual APA. Without this more granular testing, the presence of APA may be missed.
Antinuclear antibodies and anti-DNA antibodies are useful markers of an overactive immune system that can interfere with pregnancy. Anti-ovarian antibodies are associated with egg quality issues, but the literature describing the significance of these antibodies is inconclusive. Although these autoantibodies are non-specific, their presence indicates that an immune problem is active and needs to be addressed.
TREATMENT OPTIONS
Treatment varies depending on the results discussed above. In general, there is overlap between treatments, and it is important for patients to undergo each of the advised interventions to maximize treatment success. Failure to address any of these issues can result in pregnancy loss/failure and reduced efficacy, as described in the Results section.
IMMUNOLOGICAL TREATMENT
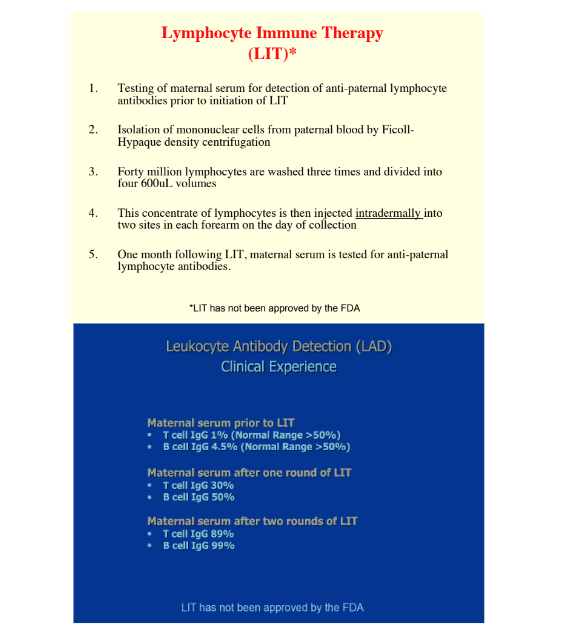
For the immunological problems there are several modalities that have been useful. Lymphocyte immune therapy (LIT) has been used to address decreased leukocyte antibodies and increased natural killer cell number and activity. The proper treatment protocol is very important, so LIT has to be done with fresh paternal lymphocytes injected intradermally into the prospective mother’s arm. There are other ways to do LIT that don’t seem to work as well. The procedure itself is rather straightforward, and results are measured in terms of leukocyte antibody detection. An example is shown in Figure 3. You may start with a maternal serum antibody level of 1-5% prior to LIT with the desired range for pregnancy of greater than 50%. After one round of LIT the level may go to 30-50% so almost there but not quite. After two rounds of LIT generally you get levels of 89-99% and that is optimal for pregnancy.
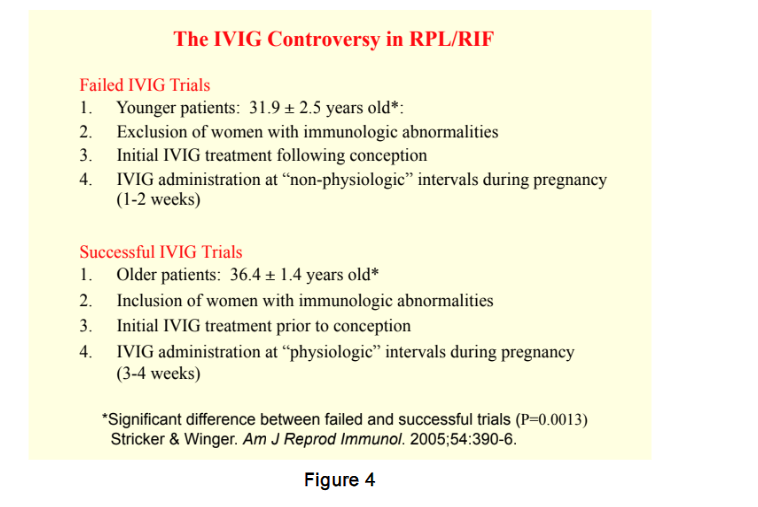
IVIG has been used for decades and it has a number of beneficial effects on the immune system. There is controversy concerning IVIG in terms of failed IVIG trials versus successful IVIG trials in RPL/RIF. Stricker and Winger reviewed these studies and found major differences in patient selection and treatment protocols. In the failed IVIG trials the patients were much younger (mean age 31.9 years), the studies excluded women with immunological abnormalities, the initial IVIG treatment was done following conception, and the IVIG administration was done at non-physiologic intervals (usually every 1-2 weeks during pregnancy). In contrast, the successful IVIG trials were in older patients (mean age 36.4 years), women with immunological abnormalities were included (which makes sense because that is the target population), the initial IVIG treatment was done prior to conception, and IVIG administration was done at physiologic intervals during pregnancy (every 3-4 weeks). Intralipid therapy has been proposed as an alternative to IVIG, but the evidence supporting intralipid therapy is inconsistent.
Dexamethasone has several benefits in RPL/RIF because it stabilizes the clotting system, suppresses natural killer cell function, increases T-reg cells and suppresses autoantibody production, so it is very useful in this situation. The reason that dexamethasone is preferred as opposed to prednisone is that it has less side effects in terms of fluid retention, hyperglycemia and hypertension. Dexamethasone also has a slightly longer half-life than prednisone, which is beneficial in this situation. Adalimumab is a fully human anti-tumor necrosis factor (TNF) monoclonal antibody that has a high affinity for TNF and a long half-life of 12 to 14 days, so it can be dosed every two weeks. The safety of anti-TNF therapy has been a concern but we use this treatment well before conception or embryo transfer to eliminate any fetal exposure to the drug. A short treatment course (usually over one month) avoids the risk of lymphoid malignancy that has been seen with chronic use of anti-TNF therapy. Although adalimumab therapy has been expensive in the past, the recent approval of adalimumab biosimilars (generic versions of the biologic product) has decreased the cost of this treatment. Other immune modulators such as hydroxychloroquine, tacrolimus and filgrastim have had mixed results in treating pregnancy failure.
METABOLIC TREATMENT
Metabolic treatments involve generic medications that are usually covered by insurance. For thyroid abnormalities we use thyroid hormone with immunosuppressive therapy if there are autoantibodies to the thyroid. The goal is to keep the thyroid stimulating hormone level at 1.5 or less. For low serum serotonin levels we use a selective serotonin uptake inhibitor (SSRI) to increase serotonin levels. Interestingly, a meta-analysis shows that SSRIs can decrease TNF levels. Although it is a minor decrease, no other antidepressants have a suppressive effect on TNF. For insulin resistance, metformin is the standard of care for women attempting pregnancy. Insulin resistance may be associated with polycystic ovarian syndrome (PCOS), and if PCOS is present, metformin therapy may be helpful to regulate menstrual cycles and support ovulation prior to conception. Progesterone is another hormonal treatment that is usually prescribed by a reproductive endocrinologist.
ANTICOAGULATION TREATMENT
For treatment of the thrombophilia gene mutations we use a standard approach of baby aspirin, enoxaparin and dexamethasone. Methylfolate is added for patients with the MTHFR mutation who tend to underutilize folic acid. Recent research demonstrates that methylfolate works better than folic acid for this purpose. For antiphospholipid antibodies we use the same backbone plus IVIG. Heparin and enoxaparin interestingly can improve implantation according to studies in the medical literature. For women with heparin intolerance including heparin-induced thrombocytopenia, parenteral fondaparinux (a direct Factor Xa inhibitor) may be a safer alternative. For direct oral anticoagulants (DOACs), the safety and efficacy are not well defined in pregnancy because published randomized controlled trials of these products have largely excluded pregnant women.
Methods
A total of 1,414 RPL/RIF patients seen at the Alan E. Beer Medical Center for Reproductive Immunology were included in this retrospective cohort analysis. Immunological blood testing was performed at ReproSource Fertility Diagnostics Laboratory, Marlborough, MA. Routine coagulation and metabolic blood testing was performed through regional clinical laboratories. Blood work was performed prior to pregnancy and monthly thereafter as needed, and patients were followed throughout pregnancy. Data was collected from 2007 through 2022. All patient information was deidentified and maintained in strict confidence. Once deidentified, patient data was examined, cleaned, and analyzed using Microsoft Excel. Four groups were selected for analysis: (a) women with normal cytokines using their own eggs; (b) women with high cytokines using their own eggs; (c) women using donor eggs; and (d) women returning for a second baby in the program. Each group was compared to a No Treatment group using a Fisher’s 2-Tailed Exact Test. The controls were age matched accordingly.
Results
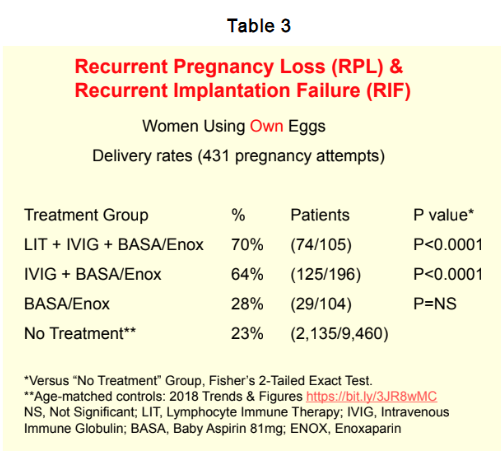
Our treatment results for the overall population screened at the Beer Center over 15 years is shown in Table 3. We had a total of 1,414 patients with an average age at conception of 37.8 years. The mean number of prior live births was very low (0.5) and mean number of pregnancy failures was 4.0 for women using their own eggs. We used a control group from the medical literature of women who were eligible for IVF which basically is this entire group, and the live-birth success rate with IVF alone was 23%. With the addition of baby aspirin and enoxaparin the pregnancy success rate went to 28%, which was not significantly better, but adding IVIG plus anticoagulation the rate went to 64%. When we add LIT plus IVIG plus anticoagulation we get a 70% success rate which was highly significant (P=0.0001).
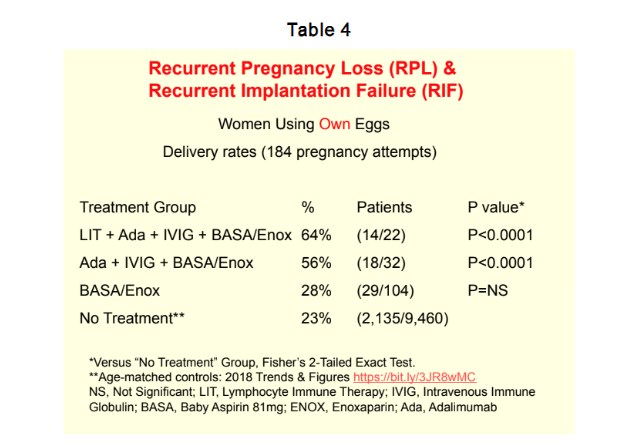
For women with high cytokine levels who were eligible for adalimumab treatment, the success rate improved not quite as much as patients without these high cytokines but we still manage to get rates of 56% with IVIG and 64% with LIT plus IVIG which were significantly better than controls.
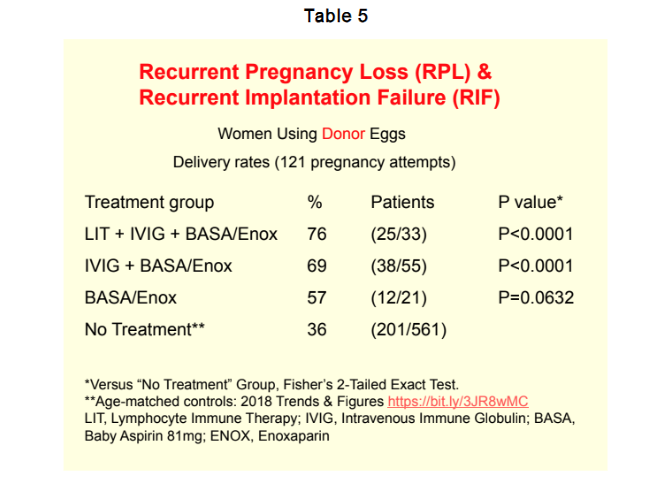
In women using donor eggs the age of conception was significantly older (43.6 years) and the mean number of prior live births was also very low (0.5). The mean number of pregnancy failures was very high (5.2). Again, the live-birth success rate with IVF alone was 23%. In women using donor eggs the success rate was 36% using baby aspirin and enoxaparin, and that rate went to 57% which is not quite significant. With IVIG plus anticoagulation the rate went to 69%, and adding LIT to IVIG and anticoagulation produced a 76% success rate in these older women, and that rate was a highly significant improvement.
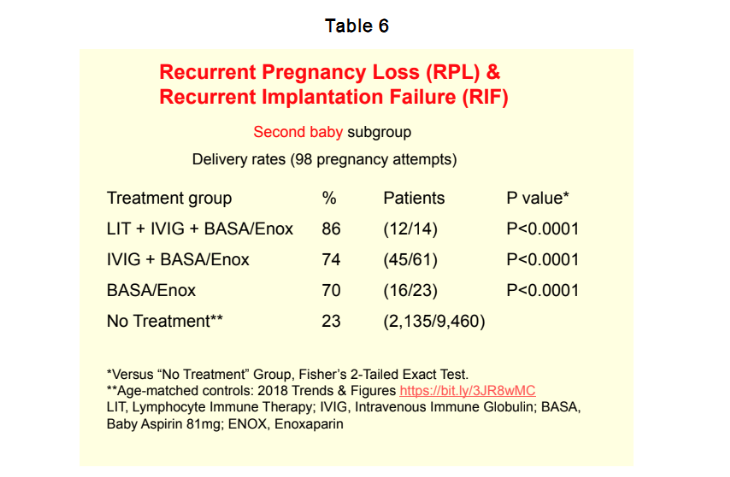
One interesting group is women going for second babies in the program, and we had a number of those with an average age of 37.6 years. The mean number of prior live births was 1.2 and the mean number of prior pregnancy failures was 5.5. When we looked at this group again even with just baby aspirin and enoxaparin the success rate went to 70% in these women and then with IVIG to 74% and with LIT plus IVIG plus anticoagulation to 86 percent. This group did very well with second pregnancies even with minimal treatment of their abnormalities.
Discussion
The classic view of immune balance in pregnancy involves the TH1 and TH2 type immune responses. However, this model does not capture the true complexity of pregnancy, and a number of factors contributing to RPL/RIF have been identified in recent years. Based on this complexity, a diagnostic and treatment protocol must address a triad of issues including immunological, metabolic and coagulation abnormalities that contribute to RPL/RIF. The aim of this analysis was to determine the pregnancy success rate with implementation of the Beer treatment protocol. We found that the Beer protocol significantly improved the pregnancy success rate in our retrospective cohort study.
With the increase in older women undergoing pregnancy, clinicians must be prepared to encounter RPL/RIF. Incorporating the principles of reproductive immunology into standard obstetrical care will improve outcomes for these women. Unfortunately, access to specific treatments remains limited. For example, LIT is not approved by the Food and Drug Administration (FDA) so the treatment is not available in the USA. In failing to approve the treatment, the FDA relied on a study using poor technique. No subsequent LIT studies have been performed in the USA, although numerous studies in other countries have demonstrated the safety and efficacy of LIT. The FDA needs to approve LIT, which is available in Mexico, Canada, Brazil, England, Germany, Greece, India, China, the Philippines, Australia and even Iran, but not in the USA. Additionally, there is a significant cost burden associated with treatment of RPL/RIF for patients who may have already received multiple rounds of embryo retrievals and transfers through IVF clinics. IVIG remains quite expensive, and reliable insurance coverage would significantly reduce the financial burden of this treatment. Improved immunotherapy for natural killer cell activity would also be helpful. Oral anticoagulants could replace parenteral enoxaparin along the lines of milvexian, which is an oral enoxaparin equivalent but not approved for use in pregnancy. Finally, greater recognition and enhanced therapy of immunological factors in RPL/RIF would benefit the many women who continue to struggle with pregnancy failure.
Strengths and Limitations
The strengths of this retrospective cohort analysis are related to the single-center study design, uniform testing protocol and targeted treatment approach for all patients. Limitations include use of a historical control group that may have differed from our patient population despite age matching, but the overall pregnancy success rate in our treated cohort (70%) was significantly better than historical controls (23%). The retrospective nature of the cohort study may have influenced outcome measures in terms of missed data, but the comprehensive follow-up of patients would have compensated for this problem. Although treatment was prescribed based on test results, not all patients adhered to the treatment protocols. The pregnancy success rate in our treated cohort was greatly improved, however, implying that results of the study are accurate.
Conclusion
In conclusion, recurrent pregnancy loss and recurring implantation failure are significant problems in older women attempting pregnancy. The Beer treatment protocol addresses immunological, metabolic and coagulation abnormalities associated with RPL and RIF. Treatment of these abnormalities is associated with a significant increase in pregnancy success. Further studies are needed to evaluate the diverse components of the Beer protocol.
Acknowledgement:
We would like to acknowledge the many people who have worked with the Beer Center over the years, in particular the late Dr. Jerry Trobough who kept the home fires burning after Dr. Beer left us; the nurses at the Beer Center including Chris Sanow, Barbara Pease, Brandi Dominguez and Giselle Lopez; our office manager Khanhly Nguyen; our clinical research associate Jane Reed who performed statistical analysis on our patient data, and Dr Ed Winger who was involved with the practice for a number of years; at ReproSource Dr. Benjamin Leader and Charles Jenkins; and the Reproductive Immunology support group of about 68,000 people who were involved in the program. We would also like to thank Dr. David Clark and Dr. Dobri Kiprov for their early work with treatment of RPL/RIF and the numerous practitioners who have referred patients to us. We are deeply grateful for your support.
Conflict of Interest:
RBS and MCF have no conflicts of interest to declare.
Funding:
No funding was received.
Supplementary Materials A
Lymphocyte Immunization Therapy (LIT) studies
- Kling C, Steinmann J, Westphal E, Magez J, Kabelitz D. Adverse effects of intradermal allogeneic lymphocyte immunotherapy: acute reactions and role of autoimmunity. Hum Reprod. 2006 Feb;21(2):429-35.
- Nonaka T, Takakuwa K, Ooki I, Akashi M, Yokoo T, Kikuchi A, Tanaka K. Results of immunotherapy for patients with unexplained primary recurrent abortions prospective non-randomized cohort study. Am J Reprod Immunol. 2007 Dec;58(6):530-6.
- Liu Z, Xu H, Kang X, Wang T, He L, Zhao A. Allogenic lymphocyte immunotherapy for unexplained recurrent spontaneous abortion: A meta-analysis. Am J Reprod Immunol. 2016 Dec;76(6):443-453.
- Cavalcante MB, Sarno M, Araujo Júnior E, Da Silva Costa F, Barini R. Lymphocyte immunotherapy in the treatment of recurrent miscarriage: systematic review and meta-analysis. Arch Gynecol Obstet. 2017 Feb;295(2):511-518.
- Hajipour H, Nejabati HR, Latifi Z, Hamdi K, Bahrami-Asl Z, Fattahi A, Nouri M. Lymphocytes immunotherapy for preserving pregnancy: Mechanisms and challenges. Am J Reprod Immunol. 2018 Sep;80(3):e12853.
- Raut MK, Raut MM. Role of lymphocyte immunization therapy (LIT) in repeated miscarriages – A review. Am J Reprod Immunol. 2023 Feb;89(2):e13629.
Th1/Th2/Anti-TNF studies
- Wu H, You Q, Jiang Y, Mu F. Tumor necrosis factor inhibitors as therapeutic agents for recurrent spontaneous abortion (Review). Mol Med Rep. 2021 Dec;24(6):847.
- Clark DA. Anti-TNFalpha therapy in immune-mediated subfertility: state of the art. J Reprod Immunol. 2010 May;85(1):15-24.
- Gharesi-Fard B, Zolghadri J, Kamali-Sarvestani E. Effect of leukocyte therapy on tumor necrosis factor-alpha and interferon-gamma production in patients with recurrent spontaneous abortion. Am J Reprod Immunol. 2008 Mar;59(3):242-50.
- Kwak-Kim JY, Chung-Bang HS, Ng SC, et al. Increased T helper 1 cytokine responses by circulating T cells are present in women with recurrent pregnancy losses and in infertile women with multiple implantation failures after IVF. Hum Reprod. 2003 Apr;18(4):767-73.
- Ahmadi M, Abdolmohammadi-Vahid S, Ghaebi M, et al. Effect of Intravenous immunoglobulin on Th1 and Th2 lymphocytes and improvement of pregnancy outcome in recurrent pregnancy loss (RPL). Biomed Pharmacother. 2017 Aug;92:1095-1102.
Natural Killer cell studies
- Beer AE, Kwak JY, Ruiz JE. Immunophenotypic profiles of peripheral blood lymphocytes in women with recurrent pregnancy losses and in infertile women with multiple failed in vitro fertilization cycles. Am J Reprod Immunol. 1996 Apr;35(4):376-82.
- King K, Smith S, Chapman M, Sacks G. Detailed analysis of peripheral blood natural killer (NK) cells in women with recurrent miscarriage. Hum Reprod. 2010 Jan;25(1):52-8.
- Thum MY, Bhaskaran S, Abdalla HI, Ford B, Sumar N, Shehata H, Bansal AS. An increase in the absolute count of CD56dimCD16+CD69+ NK cells in the peripheral blood is associated with a poorer IVF treatment and pregnancy outcome. Hum Reprod. 2004 Oct;19(10):2395-400.
- Ntrivalas EI, Kwak-Kim JY, Gilman-Sachs A, Chung-Bang H, Ng SC, Beaman KD, Mantouvalos HP, Beer AE. Status of peripheral blood natural killer cells in women with recurrent spontaneous abortions and infertility of unknown aetiology. Hum Reprod. 2001 May;16(5):855-61.
- Emmer PM, Nelen WL, Steegers EA, Hendriks JC, Veerhoek M, Joosten I. Peripheral natural killer cytotoxicity and CD56(pos)CD16(pos) cells increase during early pregnancy in women with a history of recurrent spontaneous abortion. Hum Reprod. 2000 May;15(5):1163-9.
Autoantibody/Corticosteroid studies
- Bramham K, Thomas M, Nelson-Piercy C, Khamashta M, Hunt BJ. First-trimester low-dose prednisolone in refractory antiphospholipid antibody-related pregnancy loss. Blood. 2011 Jun 23;117(25):6948-51.
- Vinatier D, Dufour P, Cosson M, Houpeau JL. Antiphospholipid syndrome and recurrent miscarriages. Eur J Obstet Gynecol Reprod Biol. 2001 May;96(1):37-50.
- Dai YF, Lin LZ, Lin N, et al. APA scoring system: a novel predictive model based on risk factors of pregnancy loss for recurrent spontaneous abortion patients. J Obstet Gynaecol. 2022 Jan 20:1-6.
T regulatory cell studies
- Saito S, Shima T, Nakashima A, Shiozaki A, Ito M, Sasaki Y. What is the role of regulatory T cells in the success of implantation and early pregnancy? J Assist Reprod Genet. 2007 Sep;24(9):379-86. Review.
- Guerin LR, Prins JR, Robertson SA. Regulatory T-cells and immune tolerance in pregnancy: a new target for infertility treatment? Hum Reprod Update. 2009 Sep-Oct;15(5):517-35.
- Tang C, Hu W. The role of Th17 and Treg cells in normal pregnancy and unexplained recurrent spontaneous abortion (URSA): New insights into immune mechanisms. Placenta. 2023 Oct;142:18-26.
IVIG studies
- Clark DA, Coulam CB, Stricker RB. Is intravenous immunoglobulins (IVIG) efficacious in early pregnancy failure? A critical review and meta-analysis for patients who fail in vitro fertilization and embryo transfer (IVF). J Assist Reprod Genet. 2006 Jan;23(1):1-13.
- Jafarzadeh S, Ahmadi M, Dolati S, et al. Intravenous immunoglobulin G treatment increases live birth rate in women with recurrent miscarriage and modulates regulatory and exhausted regulatory T cells frequency and function. J Cell Biochem. 2019 Apr;120(4):5424-5434.
- Habets DHJ, Pelzner K, Wieten L, Spaanderman MEA, Villamor E, Al-Nasiry S. Intravenous immunoglobulins improve live birth rate among women with underlying immune conditions and recurrent pregnancy loss: a systematic review and meta-analysis. Allergy Asthma Clin Immunol. 2022 Mar 11;18(1):23.
- Muyayalo KP, Li ZH, Mor G, Liao AH. Modulatory effect of intravenous immunoglobulin on Th17/Treg cell balance in women with unexplained recurrent spontaneous abortion. Am J Reprod Immunol. 2018 Oct;80(4):e13018.
- Yuan X, Zhang W, Wang T, Jiang P, Wang ZK, Li CQ. Use of intravenous immunoglobulin in antiphospholipid antibody positive patients with high risk of miscarriage: a systematic review and meta-analysis. PeerJ. 2024 Oct 31;12:e18419.
Anticoagulation studies
- Mak A, Cheung MW, Cheak AA, Ho RC. Combination of heparin and aspirin is superior to aspirin alone in enhancing live births in patients with recurrent pregnancy loss and positive anti-phospholipid antibodies: a meta-analysis of randomized controlled trials and meta-regression. Rheumatology (Oxford). 2010 Feb;49(2):281-8.
- Yu X, He L. Aspirin and heparin in the treatment of recurrent spontaneous abortion associated with antiphospholipid antibody syndrome: A systematic review and meta-analysis. Exp Ther Med. 2021 Jan;21(1):57.
- Huang W, Yu Y, Chen L, Tang X, Fang X, Ou X, Du X. Comparative effectiveness of low molecular weight heparin on live birth for recurrent spontaneous abortion: systematic review and network meta-analysis. Am J Obstet Gynecol MFM. 2025;7:101572.
Thrombophilia Gene Mutations
- Barut MU, Bozkurt M, Kahraman M, Yıldırım E, Imirzalioğlu N, Kubar A, Sak S, Ağaçayak E, Aksu T, Çoksüer H. Thrombophilia and recurrent pregnancy loss: The enigma continues. Med Sci Monit. 2018;24:4288-4294.
- Joksic I, Mikovic Z, Filimonovic D, Munjas J, Karadzov ON, Egic A, Joksic G. Combined presence of coagulation factor XIII V34L and plasminogen activator inhibitor 1 4G/5G gene polymorphisms significantly contribute to recurrent pregnancy loss in Serbian population. J Med Biochem. 2020;39:199-207.
- Wen Y, He H, Zhao K. Thrombophilic gene polymorphisms and recurrent pregnancy loss: a systematic review and meta-analysis. J Assist Reprod Genet. 2023;40:1533-1558.
Supplementary Materials B
Beer Center Publications
- Fesler MC, Sanow MC, Mantle DL, Trobough GE, Nasseri-Nik N, Stricker RB. Chronic histiocytic intervillositis: Successful treatment of recurrent miscarriage with anticoagulation and immunotherapy. Am J Reprod Immunol 2021;85 (Suppl.):69
- Reed JL. Winger EE. IVIg therapy increases delivery birthweight in babies born to women with preconception proportion of peripheral blood NK cells greater than twelve percent. Clin Exp Obstet Gynecol. 2017;44:384-91.
- Winger EE, Reed JL, Ashoush S, El-Toukhy T, Ahuja S, Taranissi M. Elevated preconception CD56(+) 16(+) and/or Th1:Th2 levels predict benefit from IVIG therapy in subfertile women undergoing IVF. Am J Reprod Immunol. 2011;66:394-403
- Winger EE, Reed JL. Low Circulating CD4(+)CD25(+)Foxp3(+) T Regulatory cell levels predict miscarriage risk in newly pregnant women with a history of failure. Am J Reprod Immunol. 2011;66:320-8
- Winger EE, Reed JL:A retrospective analysis of fondaparinux versus enoxaparin treatment in women with infertility or pregnancy loss. Am J Reprod Immunol 2009;62:253-60.
- Winger EE, Reed JL, Ashoush S, Sapna A, El-Toukhy T, Taranissi M. Treatment with adalimumab (Humira) and intravenous immunoglobulin (IVIG) improves pregnancy rates in women undergoing IVF. Am J Reprod Immunol. 2009;61:113-20.
- Winger EE, Reed JL: Treatment with tumor necrosis factor inhibitors and intravenous immunoglobulin improves live birth rates in women with recurrent spontaneous abortion. Am J Reprod Immunol. 2008;60:8-16.
- Stricker RB, Winger EE. Update on treatment of immunologic abortion with low-dose intravenous immunoglobulin. Am J Reprod Immunol. 2005;54:390-6.
- Stricker RB, Steinleitner A, Winger EE: Intravenous immunoglogulin (IVIG) therapy for immunologic abortion. Clin Applied Immunol Rev. 2002;2:187-99.
- Stricker RB, Steinleitner A, Bookoff CN, Weckstein LN, Winger EE. Successful treatment of immunologic abortion with low-dose intravenous immunoglobulin. Fertil Steril. 2000;73:536-40.
References:
- Nybo Andersen AM, Wohlfahrt J, Christens P, Olsen J, Melbye M. Maternal age and fetal loss: population based register linkage study. BMJ. 2000;320(7251):1708-12.
- Centers for Disease Control and Prevention. 2018 Assisted Reproductive Technology National Summary Report. US Dept of Health and Human Services. 2021;1-16. Available at https://archive.cdc.gov/www_cdc_gov/art/pdf/2018-report/ART-2018-national-summary-508.pdf . Accessed November 17, 2025.
- Bashiri A, Halper KI, Orvieto R. Recurrent implantation failure-update overview on etiology, diagnosis, treatment and future directions. Reprod Biol Endocrinol 2018;16:121.
- Mekinian A, Cohen J, Alijotas-Reig J, Carbillon L, Nicaise-Roland P, Kayem G, Daraï E, Fain O, Bornes M. Unexplained recurrent miscarriage and recurrent implantation failure: Is there a place for immunomodulation? Am J Reprod Immunol. 2016; 76:8-28.
- Busnelli A, Somigliana E, Cirillo F, Baggiani A, Levi-Setti PE. Efficacy of therapies and interventions for repeated embryo implantation failure: a systematic review and meta-analysis. Sci Rep. 2021;11:1747.
- Carp H. Immunotherapy for recurrent pregnancy loss. Best Pract Res Clin Obstet Gynaecol. 2019; 60:77-86.
- Kling C, Steinmann J, Westphal E, Magez J, Kabelitz D. Adverse effects of intradermal allogeneic lymphocyte immunotherapy: acute reactions and role of autoimmunity. Hum Reprod. 2006;21:429-35.
- Nonaka T, Takakuwa K, Ooki I, et al. Results of immunotherapy for patients with unexplained primary recurrent abortions prospective non-randomized cohort study. Am J Reprod Immunol. 2007;58:530-6.
- Liu Z, Xu H, Kang X, Wang T, He L, Zhao A. Allogenic lymphocyte immunotherapy for unexplained recurrent spontaneous abortion: A meta-analysis. Am J Reprod Immunol. 2016;76:443-453.
- Cavalcante MB, Sarno M, Araujo Júnior E, Da Silva Costa F, Barini R. Lymphocyte immunotherapy in the treatment of recurrent miscarriage: systematic review and meta-analysis. Arch Gynecol Obstet. 2017;295:511-518.
- Hajipour H, Nejabati HR, Latifi Z, et al. Lymphocytes immunotherapy for preserving pregnancy: Mechanisms and challenges. Am J Reprod Immunol. 2018;80:e12853.
- Raut MK, Raut MM. Role of lymphocyte immunization therapy (LIT) in repeated miscarriages – A review. Am J Reprod Immunol. 2023;89:e13629.
- Wu H, You Q, Jiang Y, Mu F. Tumor necrosis factor inhibitors as therapeutic agents for recurrent spontaneous abortion (Review). Mol Med Rep. 2021;24:847.
- Clark DA. Anti-TNFalpha therapy in immune-mediated subfertility: state of the art. J Reprod Immunol. 2010;85:15-24.
- Gharesi-Fard B, Zolghadri J, Kamali-Sarvestani E. Effect of leukocyte therapy on tumor necrosis factor-alpha and interferon-gamma production in patients with recurrent spontaneous abortion. Am J Reprod Immunol. 2008;59:242-50.
- Kwak-Kim JY, Chung-Bang HS, Ng SC, et al. Increased T helper 1 cytokine responses by circulating T cells are present in women with recurrent pregnancy losses and in infertile women with multiple implantation failures after IVF. Hum Reprod. 2003;18:767-73.
- Ahmadi M, Abdolmohammadi-Vahid S, Ghaebi M, et al. Effect of Intravenous immunoglobulin on Th1 and Th2 lymphocytes and improvement of pregnancy outcome in recurrent pregnancy loss (RPL). Biomed Pharmacother. 2017;92:1095-1102.
- Beer AE, Kwak JY, Ruiz JE. Immunophenotypic profiles of peripheral blood lymphocytes in women with recurrent pregnancy losses and in infertile women with multiple failed in vitro fertilization cycles. Am J Reprod Immunol. 1996;35:376-82.
- King K, Smith S, Chapman M, Sacks G. Detailed analysis of peripheral blood natural killer (NK) cells in women with recurrent miscarriage. Hum Reprod. 2010;25:52-8.
- Thum MY, Bhaskaran S, Abdalla HI, et al. An increase in the absolute count of CD56dimCD16+CD69+ NK cells in the peripheral blood is associated with a poorer IVF treatment and pregnancy outcome. Hum Reprod. 2004;19:2395-400.
- Ntrivalas EI, Kwak-Kim JY, Gilman-Sachs A, et al. Status of peripheral blood natural killer cells in women with recurrent spontaneous abortions and infertility of unknown aetiology. Hum Reprod. 2001;16:855-61.
- Emmer PM, Nelen WL, Steegers EA, Hendriks JC, Veerhoek M, Joosten I. Peripheral natural killer cytotoxicity and CD56(pos)CD16(pos) cells increase during early pregnancy in women with a history of recurrent spontaneous abortion. Hum Reprod. 2000;15:1163-9.
- Hao F, Zhou X, Jin L. Natural killer cells: functional differences in recurrent spontaneous abortion. Biol Reprod. 2020;102:524-531.
- Kwak-Kim J, Gilman-Sachs A. Clinical implication of natural killer cells and reproduction. Am J Reprod Immunol. 2008;59:388-400.
- Bramham K, Thomas M, Nelson-Piercy C, Khamashta M, Hunt BJ. First-trimester low-dose prednisolone in refractory antiphospholipid antibody-related pregnancy loss. Blood. 2011;117:6948-51.
- Vinatier D, Dufour P, Cosson M, Houpeau JL. Antiphospholipid syndrome and recurrent miscarriages. Eur J Obstet Gynecol Reprod Biol. 2001;96:37-50.
- Dai YF, Lin LZ, Lin N, et al. APA scoring system: a novel predictive model based on risk factors of pregnancy loss for recurrent spontaneous abortion patients. J Obstet Gynaecol. 2022;42:2069-2074.
- Saito S, Shima T, Nakashima A, et al. What is the role of regulatory T cells in the success of implantation and early pregnancy? J Assist Reprod Genet. 2007;24:379-86.
- Guerin LR, Prins JR, Robertson SA. Regulatory T-cells and immune tolerance in pregnancy: a new target for infertility treatment? Hum Reprod Update. 2009;15:517-35.
- Tang C, Hu W. The role of Th17 and Treg cells in normal pregnancy and unexplained recurrent spontaneous abortion (URSA): New insights into immune mechanisms. Placenta. 2023;142:18-26.
- Clark DA, Coulam CB, Stricker RB. Is intravenous immunoglobulins (IVIG) efficacious in early pregnancy failure? A critical review and meta-analysis for patients who fail in vitro fertilization and embryo transfer (IVF). J Assist Reprod Genet. 2006;23:1-13.
- Jafarzadeh S, Ahmadi M, Dolati S, et al. Intravenous immunoglobulin G treatment increases live birth rate in women with recurrent miscarriage and modulates regulatory and exhausted regulatory T cells frequency and function. J Cell Biochem. 2019;120:5424-5434.
- Habets DHJ, Pelzner K, Wieten L, Spaanderman MEA, Villamor E, Al-Nasiry S. Intravenous immunoglobulins improve live birth rate among women with underlying immune conditions and recurrent pregnancy loss: a systematic review and meta-analysis. Allergy Asthma Clin Immunol. 2022;18:23.
- Muyayalo KP, Li ZH, Mor G, Liao AH. Modulatory effect of intravenous immunoglobulin on Th17/Treg cell balance in women with unexplained recurrent spontaneous abortion. Am J Reprod Immunol. 2018;80:e13018.
- Yuan X, Zhang W, Wang T, Jiang P, Wang ZK, Li CQ. Use of intravenous immunoglobulin in antiphospholipid antibody positive patients with high risk of miscarriage: a systematic review and meta-analysis. PeerJ. 2024;12:e18419.
- Mak A, Cheung MW, Cheak AA, Ho RC. Combination of heparin and aspirin is superior to aspirin alone in enhancing live births in patients with recurrent pregnancy loss and positive anti-phospholipid antibodies: a meta-analysis of randomized controlled trials and meta-regression. Rheumatology (Oxford). 2010;49:281-8.
- Yu X, He L. Aspirin and heparin in the treatment of recurrent spontaneous abortion associated with antiphospholipid antibody syndrome: A systematic review and meta-analysis. Exp Ther Med. 2021;21:57.
- Huang W, Yu Y, Chen L, Tang X, Fang X, Ou X, Du X. Comparative effectiveness of low molecular weight heparin on live birth for recurrent spontaneous abortion: systematic review and network meta-analysis. Am J Obstet Gynecol MFM. 2025;7:101572.
- Barut MU, Bozkurt M, Kahraman M, Yıldırım E, Imirzalioğlu N, Kubar A, Sak S, Ağaçayak E, Aksu T, Çoksüer H. Thrombophilia and recurrent pregnancy loss: The enigma continues. Med Sci Monit. 2018;24:4288-4294.
- Joksic I, Mikovic Z, Filimonovic D, Munjas J, Karadzov ON, Egic A, Joksic G. Combined presence of coagulation factor XIII V34L and plasminogen activator inhibitor 1 4G/5G gene polymorphisms significantly contribute to recurrent pregnancy loss in Serbian population. J Med Biochem. 2020;39:199-207.
- Wen Y, He H, Zhao K. Thrombophilic gene polymorphisms and recurrent pregnancy loss: a systematic review and meta-analysis. J Assist Reprod Genet. 2023;40:1533-1558.

