Intertriginous Dermatitis: Causes, Risks, and Management
Intertriginous Dermatitis
Joyce M. Black, PhD, RN, FAAN1
- Florence Niedfelt Professor of Nursing
University of Nebraska Medical Center,
Omaha, Nebraska US
OPEN ACCESS
PUBLISHED: 30 November 2024
CITATION: Black, JM., 2024. Intertriginous Dermatitis Medical Research Archives, [online] 12(11). https://doi.org/10.18103/mra.v12i11.5957
COPYRIGHT © 2024 European Society of Medicine. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
DOI https://doi.org/10.18103/mra.v12i11.5957
ISSN 2375-1924
ABSTRACT
Moisture associated skin damage (MASD) is a label for a spectrum of skin injury from 4 sources: exposure to urine and stool (incontinence associated dermatitis), sweat (intertriginous dermatitis), wound exudate (periwound dermatitis) and stoma exudate (peristomal dermatitis). Intertriginous dermatitis (ITD), also known as intertrigo, is a common inflammatory disorder that occurs due to skin-on-skin friction in the skin folds, because of moisture becoming trapped due to poor air circulation. Intertrigo’s Latin translation, inter (between) and terere (to rub) helps explain the pathophysiology of the condition. The 11th revision of the World Health Organization’s (WHO) International Classification of Diseases (ICD-11) now contains codes for the separate forms of MASD within the EK02 irritant contact dermatitis section. This article provides a general overview of intertriginous dermatitis and outlines its etiology, pathophysiology and offers management techniques. ITD does not have a strong evidence base for practice therefore, practitioners often have to rely on experience.
Keywords
Intertriginous dermatitis, moisture associated skin damage, skin folds, management techniques
Etiology
The main etiology of ITD is friction between opposing skin surfaces. Skin folds and joints have elevated risk for ITD. Flexural surfaces and skin folds have a higher surface temperature compared to other body parts. Mild erythema forms and can progress to more severe forms with open superficial skin wounds, erosions, maceration and crusting. Occlusive clothing also contributes to the skin fold becoming warm and moist.
Obesity is often associated with ITD and creates several additional risk factors for ITD. Obese patients sweat more profusely to control their body temperature. In the obese, large skin folds with thicker layers of subcutaneous fat have increased frictional forces. Increased sweating and reduced ability to clean the skin folds can make it difficult for the person to ensure that these body areas remain clean and dry.
In patients with a Body Mass Index (BMI) over 25, the skin is also more alkaline. Alkaline conditions favor bacterial and fungal growth. Intertriginous areas with a higher pH are particularly vulnerable to candidiasis. When damage to the skin’s barrier function is injured by friction and moisture with or without occlusion the injury leads to the reduction of the protective resident microflora and allows fungal overgrowth, mostly with Candida albicans. Fungi can sense ambient pH and respond by adhering to the skin, multiplying and invading. Their metabolites further increase skin pH resulting in a clinically manifest infection (mycosis).
When the sweat is trapped in the skin fold, the skin macerates. When obese persons are ambulatory, the skin folds are “ventilated” a bit as the person walks, but once the person is confined to bed, one skin fold lies on another and the posterior skin folds are trapped on the bed, so the maceration increases. Because the dark, moist skin fold is a suitable breeding ground for microorganisms, secondary cutaneous bacterial and superficial fungal infections often occur.
The link between obesity and intertrigo is well established, and there is a direct relationship between the degree of obesity and the incidence of intertrigo. This is partly because of the disruption in skin barrier function linked to obesity.
Incidence and prevalence
Incidence and prevalence data on intertriginous dermatitis is becoming somewhat clearer with more recent studies. However, the lack of standard definitions and overlap of definitions remains a problem. For example, “moisture lesions” from exposure to urine as well as sweat exist in the gluteal folds, so the true etiology of the problem may not be clear. Also, there is an overlap in medical taxonomies between intertrigo, dermatomycoses and bacterial skin infections. In the studies reported below, the skin examiners were skin and wound professionals, so the findings can be considered more valid.
Kottner and colleagues examined data of prevalence of intertrigo in hospitals, care homes and home care between 2013 and 2016. The source of data was annual prevalence studies of four years from the Netherlands. The prevalence of ITD was highest in the home, at 9.6%, followed by aged care facilities (6.7%) and lowest in the hospital (2%). Having a high BMI, diabetes mellitus (DM) and being dependent on others for care were highly associated with ITD in all settings. Seventy percent of cases of ITD occurred after admission.
A hospital system in South Carolina in the US reported on the prevalence and incidence of ITD dermatitis over a 3-year period from 2014-2016. The mean prevalence of ITD was 40% at the time of admission to the hospital over the 3-year period, with a variance of 36% to 42%. The mean incidence of hospital-acquired ITD was 33%, with the range 29-39%. The incidence of ITD was highest in patients classified as obese using the body mass index. ITD was most often reported in the gluteal cleft.
In aged care settings in Berlin, Germany in 2014-2015, the prevalence of intertrigo was 16.1%. The submammary fold was most often affected (9.9%), followed by the inguinal region (9.4%), axilla (0.5%) and abdominal region (0.5%). A more recent study of aged people in Berlin examined the prevalence of multiple skin problems, including ITD. Most of the residents had xerosis cutis followed by ITD. More than half of the nursing home residents were affected by two or more skin conditions at the same time.
The most recent study of the prevalence of intertriginous dermatitis was conducted in Germany in aged care in 17 aged care homes. ITD was found in 35% of the residents. The most common locations were the trunk, genital area and the feet. It is noteworthy that the prevalence had increased from earlier studies in aged care in Germany.
Risk Factors
While everyone has skin folds, obese persons are the most commonly affected with intertriginous dermatitis. Some likely correlations to obesity are the inability to clean skin folds and increased heat and moisture in the skin fold. Similarly, increasing age and dependency on others for physical care decrease the ability to fully clean the skin and greater periods of time sitting in a chair or lying in bed, when the skin fold is not ventilated. In the prevalence study by Gabriel and colleagues, increased age was statistically significantly associated with the presence of intertrigo (OR 1.05; 95% CI 1.00 to 1.10). Care dependency in bathing activities and having a longer length of stay (or a longer duration of care) was also associated with intertrigo.
Data from a study conducted on the International Prevalence of Care Quality in the Netherlands, Austria, Switzerland, the United Kingdom and Turkey were examined to determine possible risk factors. Patients with DM are more susceptible to skin infections due to hyperglycemia-induced metabolic and immunological alterations. It has been observed that in these patients, skin pH is higher, promoting bacterial colonization. Fungi are another class of pathogens often involved in skin infections in diabetic patients.
It is important to point out that not all patients with ITD are obese. Patients with spinal cord injury can sweat from autonomic dysreflexia, and that sweating is above the level of injury. However, excessive sweating occurs throughout the body also. Quadriplegic patients can develop ITD in the gluteal fold of the buttocks, when there is no other form of moisture than their sweat.
Pathophysiology
A variety of predisposing factors coincide to promote inflammation within deep skin folds, including humidity, friction, and infection. Rubbing of moist skin against moist skin leads to maceration and denudes the stratum corneum, exposing Langerhans cells to environmental pathogens that stimulate an immune reaction. Fungal or bacterial infection or colonization of the skin may contribute to intertrigo through the initiation of innate or acquired immunity-mediated inflammatory cascades. Candidal infection is common in intertrigo and may exacerbate or induce its development.
Candida albicans, a yeast-type fungus, and a limited number of other Candidal species can cause infections in the skin. But C. albicans and other Candida species are not considered normal skin flora. The organism is found in the natural flora of the mouth, vagina, and intestine. Until recently, C. albicans was responsible for approximately 80-90% of all skin infections caused by the Candida species. However, a more than 50% increase in the incidence of non-albicans Candida species have recently been reported including C. glabrata, C. parapsilosis, C. tropicalis, C. krusei, C. lusitaniae, C. dubliniensis, and C. guilliermondii. Each of these organisms exhibits characteristic virulence potential, antifungal susceptibility, and epidemiology.
Diabetes is an important factor for fungal infections. Wide variances in blood sugar, hypoxia and hypoperfusion may impair the pathogenic ability of the leukocyte. The main pathophysiologic and nutritionally relevant sugars in diabetic patients are glucose and fructose. An in-vitro study examined the effect of glucose concentration on candida growth. They reported that glucose supported C. albicans growth, and fructose did not.
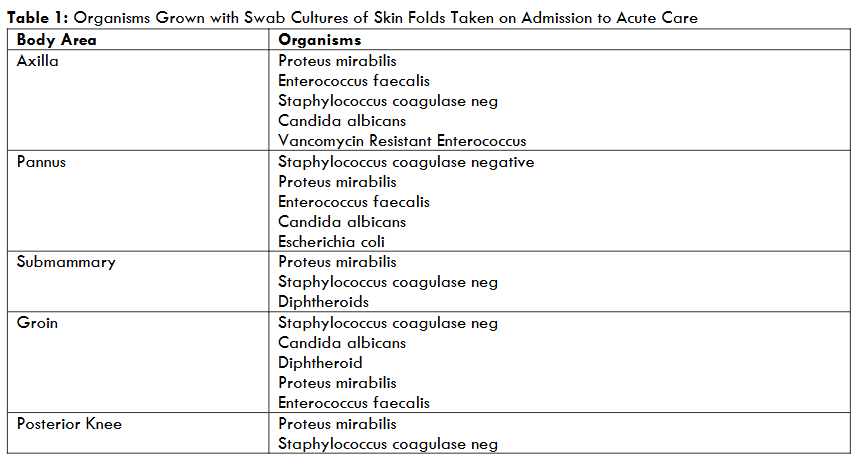
Several years ago, the writer’s facility saw ITD in every patient admitted for weight reduction surgery and were concerned because incisions were going to be near or through a skin fold. Other patients were having vascular bypass operations and groin incisions were especially problematic. A small study was conducted to culture the skin folds of the axilla, breast, abdominal pannus, groin and posterior knee on admission to the hospital to determine if the skin fold was contaminated. Results are shown in Table 1. All skin fold cultures grew coagulase negative staphylococcus aureus and proteus mirabilis. Enterococcus faecalis was cultured from the axilla, pannus and groin. Only 33% of the cultures grew Candida Albicans. These patients were instructed to shower before surgery, yet due to their obesity, it was unlikely that they were able to clean the skin folds.
A few studies have directly reported on the microbiology of toe webspace intertrigo. The study found 101 different bacteria, including Staphylococcus aureus, Streptococcus, Pseudomonas, Proteus, Klebsiella, and a few other gram-negative bacteria. Methicillin-resistant strains were present in 26% of the Staphylococcus species. Interestingly, Rao and colleagues reported multidrug resistance in 25.8% of Staphylococcus isolates and in 9.25% of Gram-negative isolates obtained from patients with intertrigo.
Manifestations
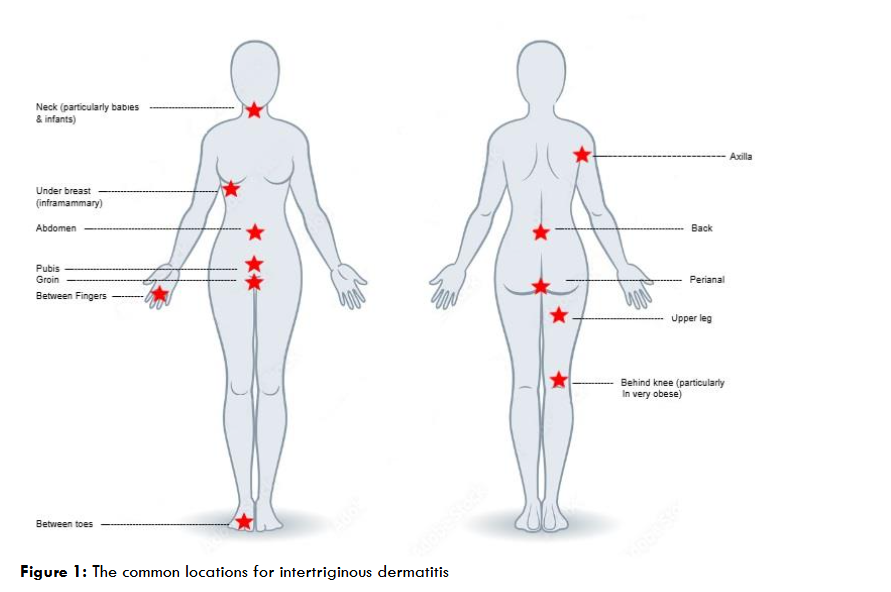
Intertrigo can occur in any area where skin opposes skin. Any skin fold may be involved with intertrigo. ITD mostly develops in the neck, axilla, sub-mammary fold, and perineum, while other sites may also be involved including antecubital, umbilical, perianal, and interdigital areas as well as abdominal folds, eyelids, and behind the ears.
The adults or infants who are obese, skin folds are accentuated, and inflammation may occur under pendulous breasts, abdominal folds, in neck creases, or in popliteal or antecubital fossae.

Intertriginous dermatitis generally has an insidious onset with symptoms such as itching, pain, burning, or prickling sensations in skinfold areas. Initially it presents itself as mildly erythematous papillae or plaques, quickly developing into exudative erosion, fissures, macerations, and crusts. The presentation of ITD is often inflammation on both sides of a skin fold – a mirror appearance. When Candida species are suspected, satellite papules and pustules are pathognomic.

Over time, the erythematous patch can develop erosions, macerations, fissures, crust, and weeping from the site. If a pustule, crust, or vesicle is visible, a secondary infection should be considered.
The moist damaged skin can become secondarily infected by bacteria or yeast and fungi. Since the open skin fissures are frequently colonized or secondarily infected, secondary cutaneous infections and acute cellulitis are threats to occur. Considering the findings in the skin fold cultures, the practitioner should be aware that secondary cutaneous infections can be caused by a variety of gram-positive or gram-negative bacteria or fungi, including yeasts. A bluish-green tint can indicate infection with Pseudomonas. An infectious intertrigo may result in serious cellulitis, especially in patients who are diabetic. Additionally, skin fissuring and ulceration can occur, possibly hidden in the deep skin folds of people who are obese, which can lead to pain, disability, and, potentially, sepsis.
Bacterial intertrigo tends to weep and is an intensely erythematous and potentially tender lesion. In cases of inguinal and perianal intertrigo, which are often associated with incontinence, gut bacteria can also be involved, such as enterococci or Escherichia coli. The presence of ‘fiery’ red lesions, exudate and foul odor often suggest bacterial rather than fungal infection. ITD should not be considered a superficial skin disorder; if left untreated, severe skin infections can occur. Systemic candidiasis is associated with a high crude mortality rate, even with first line antifungal therapy.

There are many reasons that ITD, even if effectively managed, can progress into more serious soft tissue infections such as cellulitis, candidemia, and sepsis. Therefore, if there is no sign of improvement after starting treatment plan, or if the intertrigo appears to get worse, referral to a specialist should be done as soon as possible.
Diagnosis
Take a focused history of the problem and the history of skin fold problems, asking what symptoms are present now, such as pain, itching, and burning. Ask how long the skin issue has been present and what other treatments have been tried. Ask about the use antibiotics which alter the biome and favor overgrowth of Candida. Obtain a medication history to determine if cutaneous drug reactions may be occurring. Ask about incontinence and use of incontinence products which keep the perineal skin moist and contribute to incontinence associated dermatitis. ITD is most commonly found on the skin folds of the neck breasts, abdomen, abdominal pannus, pubic pannus, groin, axilla, folds in the back, gluteal fold, gluteal cleft, folds in the posterior thigh, behind the knee and between the fingers and toes.
A full body examination of the patient is important. Some patients can assist with holding the skin folds apart and this will reduce their pain. The skin fold must be opened until the entire skin can be inspected. The depth of the skin fold should be fully examined as candidal infections are often associated with fissures, particularly in patients with existing skin disease, such as psoriasis. The examiner will require help to inspect the skinfolds of a bedbound patient. In morbidly obese patients, this examination will often require additional people to hold the skin folds up and apart. When obese patients are admitted to the hospital for possible sepsis or with burns, it is imperative that the skin folds be examined before fluid resuscitation is over. The skin folds become extremely edematous and cannot be lifted to inspect the base of the fold.

Differential diagnoses
Although intertriginous dermatitis is a common skin disease in adults, and obesity and diabetes are also common, it is not the only skin disease seen. The examiner must consider other causes of skin problems. See Table 2 for a list of differential diagnoses. While this list includes single diagnoses, patients do present with several problems.

Prevention
Little is found in the literature on prevention of ITD. Skin fold hygiene is important. Keeping skin folds dry with breathable fabrics between the skin folds and wearing loose nonsynthetic clothing will allow ventilation of the skin. Bathing with a pH-balanced soap rather than soap that is alkaline with maintain the acidic nature of the skin. Inspection of the skin fold is advisable to find ITD early and use of textiles to keep it dry is beneficial.
Prevention also should address why ITD is occurring. If possible, the patient should be encouraged to loss weight and to remain active so that the skin fold can ventilate. Neither of these interventions can be done instantly, weight loss is a major lifestyle change and being active generally causes back and leg pain. Referral to therapists for weight loss and exercise may be beneficial. If the patient is diabetic, improving glycemic control will also help with reducing the risk of Candidiasis. Exercise and dietary adjustments go hand in hand with diabetic management.
Treatment
Practices aimed at minimizing moisture and friction in the involved area and reducing susceptibility to intertrigo are the mainstays of treatment. In general, structured skin care regimens are needed to prevent and treat intertrigo in this population.
In ambulatory patients, intertriginous skin should be cleansed daily with a mild pH-balanced cleanser followed by drying of affected area with a hair dryer on a cool setting. Some skin folds, such as the groin and posterior gluteal areas, cannot be reached without help by obese patients, so the provider must ask about support in the home. If the person is living in a care home, hair dryers may not be available, and the patient or family may have to provide them.
pH-balanced skin care products should be used to restore an acidic mantle to the skin. No-rinse cleansers and moisture barriers should also be used. The use of skin barrier products to protect the skin from moisture and reduce friction are recommended, but these are often difficult for patients to apply and remove effectively themselves. Talc powder should be avoided. There is no evidence for its use and it clumps when wet. Depending on the location of the ITD, the patient may need help to reach the skin fold. Bathing in a tub should be avoided because bacteria from the perineum will reach the skin folds and may not be removed by towel drying. Showering is preferred.
Table 2: Differential Diagnoses for Intertriginous Dermatitis
| Differential diagnoses | Distinguishing Features |
|---|---|
| Allergic/irritant contact dermatitis | Prior use of toileting wipes or antiperspirants in the body area/ Confirm by patch test |
| Cutaneous drug reactions | Bright red, well demarcated lesions on the buttocks, intertriginous areas and flexor areas. Often associated with the use of non-beta-lactam antibiotics, especially amoxicillin |
| Erythrasma | Infection of the skin fold from Corynebacterium, commonly in the foot. If in the groin, presents as sharply marginated pink or brown patches with scaling. No hyphae in skin scraping |
| Hidradenitis suppurativa | Begins at puberty, more common in females. Chronic recurrent inflammatory nodules, cysts, and abscesses. Resolves with scar formation with the skin folds |
| Hailey-Hailey disease (benign familial pemphigus) | Rare genetic disease of compromised adhesion between epidermal keratinocytes. Manifests as epidermal blistering with flaccid vesicles and bullous lesions mainly in the flexural areas, which develop into erosions and crusts. Often a history of this disease in family members |
| Inverse psoriasis | Erythematous plaques with shiny/glazed appearance in skin folds. Lesions are less scaly than psoriasis. |
| Incontinence associated dermatitis | Red, denuded skin of the perineum and folds of the skin. History of incontinence or wearing briefs. |
| Perianal streptococcal cellulitis | Causes pain and bright red erythema solely on perianal skin and lacks fluorescence on Wood light examination. |
| Toxic erythema of chemotherapy | Painful erythema and edema of the intertriginous areas following chemotherapy |
| Tinea curis | Dermatophyte infection involving the groin, proximal medial thighs, perineum, or buttocks. The classic presentation consists of a centrifugally expanding, erythematous patch with partial central clearing and a slightly elevated, sharply demarcated border |
Based on expert consensus opinion, moisture-wicking textiles specifically designed for skin-fold management are now recommended for the prevention of intertrigo in high-risk patients. These have been used in North America for more than a decade and are now available in the UK. The textile is designed to lie in the skin folds, wick moisture away and allow it to evaporate, keeping the skin fold dry. They also reduce skin-on-skin friction and contain broad-spectrum antimicrobial silver threads.
Nurses often place bed linen in the skin fold. Linen absorbs the sweat and remains a wet cloth, keeping the skin fold damp. This practice must be stopped.

In bedridden patients, intertriginous skin should also be cleansed daily with a mild pH-balanced cleanser followed by drying of affected area with a hair dryer on a cool setting. This procedure can be completed with daily skin care. After the cleansing, the patient should be positioned, so that the skin fold can remain ventilated. Side lying positions are ideal with the upper leg lifted from the lower leg to keep the groin dry. Wicking fabrics exist that can aid in keeping skin folds dry. These fabrics are placed in the skin fold with a portion of the fabric outside of the skin fold, the sweat is drawn from the skin to the environment and evaporates.
In chairbound patients or patients who sit in recliners most of the time, the skin fold will not stay dry. It is important that several times per day, the resident gets out of the chair to the toilet or stand. If the resident cannot stand and is mechanically lifted to the chair, when she/he returns to bed, they must be positioned on the left or right side to ventilate the skin. Wicking fabrics can help these patients also.
The use of absorbent material or clothing, such as bed linen, towels, cotton or merino wool, to separate skin in folds is often used. These products absorb sweat and often keep the skin fold wet. If commercial skin fabrics to dry the skin are not available, many forms of athletic clothing are “breathable” and can be used. The fabric should be partially outside of the skin fold. Daily application of drying powders, such as powders composed of microporous cellulose can be used if it is sprinkled into the skin fold and not allowed to cake. Talcum powder to dry the skin fold should not be used; it has been associated with cancer. Other powders often cake together and create a mass of powder and a source of pressure ulcers.
Treatments to reduce overgrowth of Candida albicans
General clinical recommendations are to use topical miconazole as a first line treatment because it does have some gram-positive bacteriostatic action. Another common clinical recommendation is to reserve topical corticosteroid therapy for patients with marked pruritus due to the risk of skin atrophy associated with long-term topical corticosteroid use in intertriginous areas. When there is no improvement in the skin, the practitioner must consider that other bacterial infections may be growing within the ITD areas. Bacterial infection can be treated with antiseptics or antibiotics. However, the current climate of antimicrobial resistance should be considered.
This combination of skin care measures and topical therapy usually leads to marked improvement in both signs and symptoms of intertrigo within a few weeks. The same regimen can be repeated for recurrences.
Based on several case study reports, moisture wicking textiles containing silver also appear to have a role in treating complicated ITD. Cases have been reported in the US and European conferences. Treatment of intertrigo with Candidiasis is designed to improve symptoms and minimize risk for complications related to secondary infection.
Because evidence-based practice is increasingly important, a review of the evidence is included. A recent evidence-based review by Taudorf and colleagues reported that 44 studies were investigated on systemic or topical therapies for cutaneous candidiasis, of which only half had a diagnosis verified by microscopy and/or culture. Clotrimazole, nystatin and miconazole were the most studied topical drugs and demonstrated similar efficacy with complete cure rates of 73%-100%. Single-drug therapy was as effective as combinations of antifungal, antibacterial and topical corticosteroid. Adverse effects were generally mild and similar for all drugs. Thus, many drugs may be used to treat cutaneous candidiasis, while convincing evidence is lacking for most of them.
An earlier review by Mistiaen and Halm-Walters concluded that few randomized trials had been performed. Those studies which were available had methodological flaws and considerable risk of bias. Their conclusion was that there was insufficient evidence to confirm efficacy to show benefit of systemic was any better than topical therapy with antifungals and steroids. A small randomized controlled trial comparing an absorbent lotion (EZZERA liquid talc) using topical corticosteroids was conducted by Leeyaphan and colleagues. At week 2, the adsorbent lotion showed higher complete cure rates for color, partial epidermal loss, papules/pustules/vesicles/patches, dryness, and scaling than the corticosteroid without statistical significance. (Of note, this was liquid talc, not talcum powder.)
SURGERY
There are some patients with macromastia and recurrent ITD who benefit from reduction mammoplasty. Nguyen et al (2013) reporting a long-term improvement in intertrigo following breast reduction surgery of 88.6%. Another group of patients are those patients who have undergone bariatric surgery and now have large aprons of skin in the abdomen, arms and legs. This skin is usually quite moveable and to date there is no evidence that ITD develops under these skin folds. Various surgical techniques are available, such as abdominoplasty, brachioplasty and medial thigh lift. Elander and colleagues reported on 200 obese patients who underwent bariatric surgery. Abdominoplasty was requested by 70% of the patients.
TREATMENT OF CONCURRENT INCONTINENCE
Patients with incontinence-associated dermatitis and ITD often improve with the use of barrier creams to protect against the contact irritancy of urine and liquid stool. The use of incontinence briefs should be limited to times when the person is ambulating for dignity. When the person is in a chair or in bed, the incontinence brief should not be closed. The occlusive nature of the brief increases the heat and worsens the skin health.
TREATMENT OF COMORBID DISEASES
Efforts to control obesity should be made. The dermatologist is seldom an expert in nutritional care but can extend an offer to the patient to assist with referrals to nutritional services. At times surgical reduction of large breasts can help submammary ITD. Generally, belt lipectomy is performed after weight loss surgery.
Control of glycemia is also generally not managed by dermatologists, but rather internists. However, it is important to explain to the patient that efforts to control blood glucose will help reduce the severity of the ITD.
PREVENTION OF RECURRENCE
Data on recurrence or prevention of recurrence are lacking. With the high prevalence rates of ITD especially in patients and residents in care homes, it appears that research is needed to guide practice to reduce this disease.
TREATMENT OF ITD IN THE ACUTELY ILL
There is very little published on how to treat ITD in the acutely ill patient. Obese patients are hospitalized often and once bedridden, their skin folds become very difficult to offload. Tammel and colleagues presented 4 cases of obese patients with ITD that was called a “novel treatment” with acetic acid soaks for control of ITD during hospitalizations. Acetic acid lowers the pH of the wound and promotes healing. It was not a novel treatment but was the resurrection of an old-time treatment of skin disease! Hypochlorous acid is readily avoidable today is also an acidic skin cleanser that can be used on open skin. It is imperative that research be done in acute care to help care for patients who are admitted with existing ITD or develop ITD while hospitalized. Offloading large abdominal pannus is a major hurdle in acute care.
Conclusion
Intertriginous dermatitis is a common inflammatory skin disease, especially in the obese diabetic patient. All practitioners should be skillful at treating the skin fold by ventilating it, using topical miconazole and using wicking fabrics. However, not all skin fold dermatitis is due to Candida albicans, an increasing number of cases of skin loss are due to other bacteria, including methicillin-resistant staphylococcus aureus and gram-negative rods. When the skin fold does not improve within a week, consider cultures to confirm the offending organisms.
References
- Romanelli M. The diagnosis, management and prevention of intertrigo in adults: a review. J Wound Care, 2023, 32 (7): 411-419.
- World Health Organization. ICD-11. International Classification of Diseases 11th revision. Geneva: WHO; 2019. https://icd.who.int/en Accessed November 3, 2024
- Voegeli D. Intertrigo: causes, prevention and management. Brit J Nurs, 2020; 39 (12). https://doi.org/10.12968/bjon.2020.29.12.S16
- Waldman RA, Kettler AH. Dermatologic manifestations of obesity: part I mechanical causes. J Obes Weight-Loss Med. 2016;2: 010.
- Shareef AR, Prasad PVS, Kaviarasan PK. Cutaneous markers of obesity. Int J Res Med Sci. 2018;6(11):3562. https://doi.org/10.18203/2320-6012.ijrms20184243
- Rippke F, Berardesca E, Weber TM. pH and Microbial Infections. Curr Prob Dermatol. 2018:54:87-94. doi: 10.1159/000489522.
- Tüzün Y, Wolf R, Engin B, et al. Bacterial infections of the folds (intertriginous areas). Clin Dermatol; 2015, 33: (4), 420-428. https://doi.org/10.1016/j.clindermatol.2015.04.003
- Mori S, Shiraishi A, Epplen K, et al. Characterization of skin function associated with obesity and specific correlation to local/systemic parameters in American women. Lipids Health Dis. 2017;16(1):214. https://doi.org/10.1186/s12944-017-0608-9
- Yosipovitch G, DeVore A, Dawn A. Obesity and the skin: skin physiology and skin manifestations of obesity. J Am Acad Dermatol 2007; 56(6):901–916. https://doi.org/10.1016/j.jaad.2006.12.004
- Boza JC, Trindade EN, Peruzzo J, et al. Skin manifestations of obesity: a comparative study. J Eur Acad Dermatol Vener 2012; 26(10):1220–1223. https://doi.org/10.1111/j.1468-3083.2011.04265.x
- Kottner J, Everlink, I, van Haastregt J, et al. Prevalence of intertrigo and associated factors: A secondary data analysis of four annual multicenter prevalence studies in the Netherlands. Int J Nurs Stud 2020 (104): 103437
- Arnold-Long M. Johnson E. Epidemiology of incontinence-associated dermatitis and intertriginous dermatitis (intertrigo) in an acute care facility. J Wound Ostomy Continence Nurs, 2019, 46 (3): 201-206.
- Gabriel S. Hahnel E, Blume-Peytavi U, Kottner J. Prevalence and associated factors of intertrigo in aged nursing home residents: a multi-center cross-sectional prevalence study. BMC Geriatr; 2019, 19 (1): 105. doi.org/10.1186/s12877-019-1100-8
- Everink IHK, Kottner J, van Haaastrgt JCM, Halfrens R, Schols, JMGA. Skin areas, clinical severity, duration and risk factors of intertrigo: A secondary data analysis. J Tissue Viability; 2021 30,:102-107
- Volzer B, Genedy-Kalyoncu M, Fastner A, et al. Prevalence and associations of xerosis cutis, incontinence associated dermatitis, skin tears, pressure ulcers and intertrigo in aged nursing home residents: A representative prevalence study. Int J Nurs Stud, 2023, 141, 104472
- Metin A, Dilek N, Bilgili S. Recurrent candidal intertrigo: challenges and solutions. Clin Cosmet Investig Dermatol. 2018; 11: 175–185.
- Rao MR, Vasimalli VK, Gowda RS, et al. A Bacteriological Study of Intertrigo. J Pure Appl Micro 2018: 12 (4), 1839-1844 http://dx.doi.org/10.22207/JPAM.12.4.18
- Rasoulpoor S, Shohaimi S, Salari N, et al. Candida albicans skin infection in patients with type 2 diabetes: a systematic review and meta-analysis. J Diabetes Metab Disord. 2021 Apr 19;20(1):665-672. doi: 10.1007/s40200-021-00797-0.
- Man A, Ciurea CN, Pasaroiu D, et al. New perspectives on the nutritional factors influencing growth rate of Candida albicans in diabetics. An in vitro study. Mem Inst Oswaldo Cruz. 2017 Sep;112(9):587-592. doi: 10.1590/0074-02760170098.
- Kalkan G, Duygu F, Bas Y. Greenish-blue staining of underclothing due to Pseudomonas aeruginosa infection of intertriginous dermatitis. J Pak Med Assoc. 2013 Sep;63(9):1192-4.
- Cunliffe T. Intertrigo. Rickmansworth: Primary Care Dermatological Society. 2018. http://www.pcds.org.uk/clinical-guidance/intertrigo. Accessed October 12, 2024
- Voegell D. Intertrigo: causes, prevention and management. Brit J Nurs 2020, 29 (12) S16-22
- Black J, Gray M, Bliss, D, et al. Incontinence-Associated Dermatitis and Intertriginous Dermatitis: A Consensus. J Wound, Ostomy Continence Nurs, 2011; 38 (4), 359-372.
- Kalra MG, Higgins KE, Kinney BS. Intertrigo and secondary skin infections. Am Fam Physician. 2014;89(7):569–573
- Sibbald RG, Kelley J, Kennedy-Evans K-L, Labrecque C, Waters N. A practical approach to the prevention and management of intertrigo, or moisture-associated skin damage, due to perspiration: expert consensus on best practice. Wound Care Canada. 2013;11(2):36-43
- Armstrong AW, Bukhalo M, Blauvelt A. A clinician’s guide to the diagnosis and treatment of candidiasis in patients with psoriasis. Am J Clin Dermatol. 2016;17(4):329–336. https://doi.org/10.1007/s40257-016-0206-4
- Ely JW, Rosenfeld S, Seabury Stone M. Diagnosis and management of tinea infections. Am Fam Physician. 2014;90(10):702–710
- Taudorf EH, Jemec GBE, Hay RJ, Saunte DML. Cutaneous candidiasis – an evidence-based review of topical and systemic treatments to inform clinical practice. Eurp Acad Dermatol Vener 2019 33: 1863-1873. Doi: 10.1111/jdv.15782
- Mistiaen P, van Halm-Walters M. Prevention and treatment of intertrigo in large skin folds of adults: a systematic review. BioMed Central Nurs. 2010 9, http://www.biomedcentral.com/1472-6955/9/12
- Leeyaphan C, Varathai S, Trakanwittayarak S, et al. A randomized controlled trial to compare the effectiveness and safety of absorbent lotion containing tapioca starch, spent grain wax, Butyrospermum parkii extract, argania spinosa kernel oil, aloe barbadensis, rosehip oil, and allantoin with a low-potency topical corticosteroid in the treatment of intertrigo. J Cosmet Dermatol 2022; (21): 679-688.
- Nguyen JT, Palladino H, Sonnema AJ, Petty PM. Long-term satisfaction of reduction mammaplasty for bilateral symptomatic macromastia in younger patients. J Adolesc Health. 2013;53(1):112–117. https://doi.org/10.1016/j.jadohealth.2013.01.025
- Elander A, Biörserud C, Fagevik Olsén M. Excess skin after weight loss following bariatric surgery: focus on the abdomen. Surg Obes Relat Dis. 2021 May;17(5):986-993. Doi:10.1016/j.soard.2021.01.005.
- Tammel K, Benike D, Sievers B. A novel approach to treating moderate to severe incontinence-associated dermatitis and intertriginous dermatitis. J Wound Ostomy Nurs, 2019; 46(5):446-452.

