Optimizing TAVR Programs: A Nurse Protocol Approach
Optimization of a Transcatheter Aortic Valve Replacement programme: TAVR nurse protocol
Miryam González-Cebrian, RN, MSN, PhD¹²; Ignacio Cruz-González, MD, PhD¹²; Sara Alonso Meléndez, RN¹; Marta Alonso-Fernández-Gatta MD, PhD¹²; Elena Olaya González Ejido RN¹; Rosa Carreño Sanchez RN¹; Pedro L Sánchez, MD, PhD¹²
- Cardiology Department, University Hospital of Salamanca, Salamanca, Spain. IBSAL.
- CIBER-CV Instituto de Salud Carlos III (ISCIII), Madrid, Spain.
OPEN ACCESS
PUBLISHED: 30 September 2024
CITATION: González-Cebrian, M., Cruz-González, I., et al., 2024. Optimization of a Transcatheter Aortic Valve Replacement programme: TAVR nurse protocol. Medical Research Archives, [online] 12(9).
https://doi.org/10.18103/mra.v12i9.5895
COPYRIGHT: © 2024 European Society of Medicine. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
DOI https://doi.org/10.18103/mra.v12i9.5895
ISSN 2375-1924
Abstract
Transcatheter aortic valve replacement has become the treatment of choice in aortic stenosis for high-risk patients and an effective and safe alternative in intermediate and low-risk cases. The success of the procedure, good outcomes, increasing indications and an ageing population have led to an exponential increase in transcatheter aortic valve replacement procedures, leading to the development of specifics programmes.
Our aim was to redesign our transcatheter aortic valve replacement programme by implementing a nurse role to improve the quality and efficiency in the clinical management of candidate patients. We developed a protocol based on comprehensive, coordinated and patient-centred care, with a multidisciplinary character, reinforcing the nurse role as coordinator-facilitator.
The nurse role was implemented in 2022 in our hospital. We described the responsibilities assumed by the nurse during pre-, intra- and post-transcatheter aortic valve replacement procedure phases. The main pillars were patient and family education, holistic assessment, as well as ensuring continuity of care by accompanying the patient and family throughout the entire process. The transition to a minimalist approach together with the implementation of an early discharge protocol has helped to reduce the hospital stay.
Developing patient-centred programmes and giving importance to information, education, accompaniment and management of patients’ motivations and expectations helped to improve their satisfaction during the process. Monitoring the patient’s perceived experience of the process allowed us to detect areas for improvement in order to move towards quality care.
Keywords
Transcatheter aortic valve replacement, TAVR, nursing, patient care, healthcare management
Introduction
Transcatheter aortic valve replacement (TAVR) has become the treatment of choice for high-risk severe aortic stenosis (AS), as well as an effective and safe alternative for intermediate and low-risk patients, manifesting a paradigm shift in the treatment of valvular heart disease. The success of the procedure, the good clinical results, the expansion of its indications and the ageing of the population have led to an exponential increase in TAVR in recent years.
The Spanish cardiac catheterization and coronary intervention registry of the Spanish Society of Cardiology in 2023 showed this growth with more than 7000 TAVRs in the last year. In our cardiology department of the Complejo Asistencial Universitario de Salamanca (CAUSA), a reference in percutaneous interventionism in structural heart disease, about 160-200 TAVRs are performed annually.
TAVR programmes began to be implemented in Spain in 2008, mainly focused on facilitating the adoption of the technique, supporting professionals during the learning curve, accumulating experience and generating evidence.
After this initial phase, TAVR programmes have evolved to address challenges such as increasing the incidence of AS and the volume of patients to be treated, improving TAVR access by reaching more patients, reducing hospital stays and improving the patient experience throughout the whole process.
There is currently a transition to minimally invasive TAVR procedures that allow a reduction in hospital stay, minimise the use of healthcare resources and optimise final outcomes without increasing complications and mortality.
In this context, our centre set the objective of improving the quality and efficiency in the clinical management of patients with aortic valve disease candidates for TAVR and optimising the available resources.
To this end, we aimed to implement a new model of comprehensive, coordinated, person-centred and multidisciplinary care, reinforcing the role of nursing as a facilitator-coordinator of the TAVR programme: TAVR nurse protocol.
Secondary objectives were to measure the impact of the programme, implement an early discharge protocol, establish a post-TAVR rehabilitation circuit, and evaluate and measure the patient’s experience during the TAVR process.
Methods
A multidisciplinary working group was created, consisting of interventional, clinical, and imaging cardiologists together with the team of nurses familiar with the TAVR procedure (TAVR nurse). The purpose of this team was to reach a consensus on the essential aspects to be included in the nursing TAVR assessment protocol and to subsequently validate and implement the protocol. To this end, regular team meetings have been scheduled. A protocol called TAVR nurse was developed for use in our center, including prior nursing assessment, during admission and follow up.
An exhaustive literature review was conducted which, combined with the knowledge and experience of a multidisciplinary team, was key to develop the necessary contents for the TAVR nurse protocol.
TRANSCATHETER AORTIC VALVE REPLACEMENT NURSE PROTOCOL
The role of nursing within multidisciplinary teams is increasingly important. Nurses’ expertise in patient-centred care and clinical pathway development creates new opportunities for leadership to advance patient care.
A clear example is the TAVR nurse role that emerged more than a decade ago. The experience of nurses in Canada, the United States and the United Kingdom has allowed to build evidence for this activity, establishing recommendations to improve clinical nursing practices for patients undergoing TAVR, leading to the implementation of the roles of “TAVR nurse” and “TAVR coordinator”. A TAVR programme were developed describing roles, skills and competencies, highlighting the leadership role of the nurse in the process.
Until recently in Spain there were no standardised competencies or defined activities that were adapted to the reality of our environment, so a national consensus document was drawn up in 2022, through the creation of a expert TAVR nurses working group endorsed by the Spanish Association of Cardiology Nurses. The roles of TAVR nurse were defined and the most up-to-date scientific evidence from pioneering nurses in this field was summarised. This consensus document serves as a guide for the implementation of this activity in national hospitals, a model that was followed by our own hospital, CAUSA.
In Spain, only a few hospitals include TAVR nurse in their programmes, so it is important to highlight its necessity and fight for its inclusion using the example of other countries where TAVR nurse has a well-defined place, given the benefits it can bring to the patient.
The TAVR nurse aims to improve the quality of care and clinical outcomes in patients who are candidates for TAVR.
The main pillars on which it is based are:
- Health education in AS and TAVR to the patient and family, ensuring that they understand the benefits, limitations and risks. Assist in the preparation of the patient, so that they arrive in the best possible condition for the procedure.
- Comprehensive assessment of the patient including clinical and functional evaluation.
- Ensuring continuity of care from referral to discharge including home follow-up. TAVR nurse aims to facilitate, simplify and coordinate the process.
The TAVR nurse competencies described by Hawkley et al. were an important step towards the creation of TAVR nurse figure in other centres, being updated in 2022.
| COMPETENCIES AND CORE KNOWLEDGE | RESPONSIBILITIES |
|---|---|
| 1. Expertise in cardiovascular care: | 1. Program leadership: |
| • Cardiovascular nursing | • Serves as essential and central member of the Heart Team. |
| • Specialized knowledge of valvular heart disease | • Supports and leads TAVR program development |
| • Specialized knowledge of TAVR. | • Participates in program evaluation and quality improvement to improve outcomes |
| 2. Specialized knowledge of providing care patients with aortic stenosis: | 2. Facilitate of patient-focused processes of care: |
| • Complex heart disease, multiple comorbidities and frailty | • Develops seamless and patient-centred processes and clinical pathways |
| 3. Clinical assessment skills: | • Develops evaluation pathways, including diagnostic testing and functional assessment |
| • Comprehensive cardiovascular assessment | • Conducts clinical triage and wait-list management |
| • Assessment of frailty and functional status. | • Case manages urgent in-patients and interhospital referral |
| 4. Patient and family education: | • Facilitates referrals to subspeciality consultants |
| • Assessment of learning needs to individual teaching | • Facilitates and contributes to multidisciplinary, treatment decision making |
| • Patient and family teaching skills | • Coordination of procedure planning, admission and follow up |
| • Conduct of shared decision making | 3. Development of communication pathways: |
| 5. Coordination of complex processes of care: | • Conducts patient and family education and promotes shared decision making. |
| • Organizational skillset to develop and individualize assessment and procedure planning pathways. | • Leads communication with the Heart Team |
| 6. Clinical leadership: | • Facilitates communication with administration for planning purposes |
Each hospital should adapt these competencies to its center context and protocols, as we have done in our TAVR nurse CAUSA protocol.
| RESPONSIBILITIES | TAVR nurse CAUSA Protocol 2022 2023 2024 |
|---|---|
| Inclusion of patients scheduled for TAVR in TAVR nurse programme | x |
| Comprehensive assessment | x |
| Patient and family health education | x |
| Pre-selection of patients who are candidates for early discharge | x |
| Early detection of cardiac amyloidosis in patients with AS | x |
| Early discharge support | x |
| Point of contact for patient and family during the whole process | x |
| Follow-up coordination | x |
| Communication with TAVR referring physicians | x |
| Evaluation of the patient’s experience during the TAVR process | x |
| Inclusion of hospital admitted and emergency patients in the TAVR programme, in addition to scheduled patients. | x |
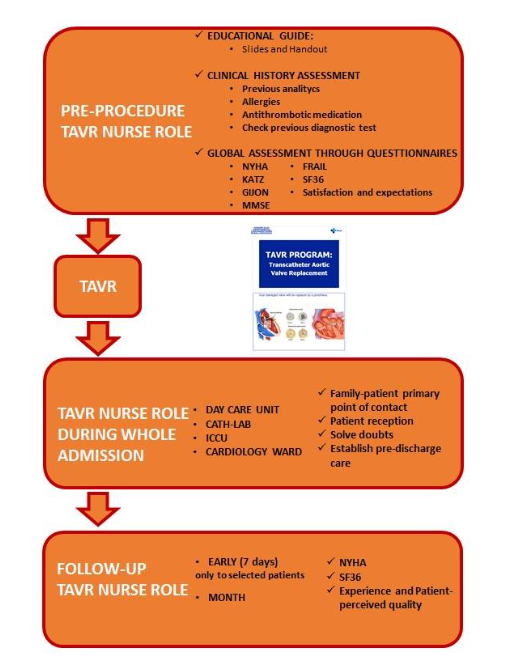
Once TAVR is indicated for a patient with aortic valve disease, the patient is included in the TAVR nurse programme. The TAVR nurse contacts the patient informing him/her that he/she will be the patient’s reference throughout the process. In addition, the TAVR nurse collects data to take a brief medical history. The nurse plays a facilitator-coordinator role managing appointments, complementary tests, waiting list, assesses the patient comprehensively, coordinates the follow-up and educates. The TAVR nurse is the point of contact for the family/patient and for the multidisciplinary team within the programme.
Health education
In the pre-procedure assessment in the TAVR nurse clinic, the nurse starts health education for the patient and caregiver, including information about the aortic valve disease, steps to follow, previous complementary tests and about the procedure itself, resolving any doubts they may have. We included a virtual tour of the center areas involved during admission and the activities carried out in each of them, informing the patient of the necessary preparation.
We also developed an informative brochure with the most important points to remember, which is handed out at the pre-TAVR nurse clinic, in order to avoid the patient forgetting some of the information that we transmit at the consultation.
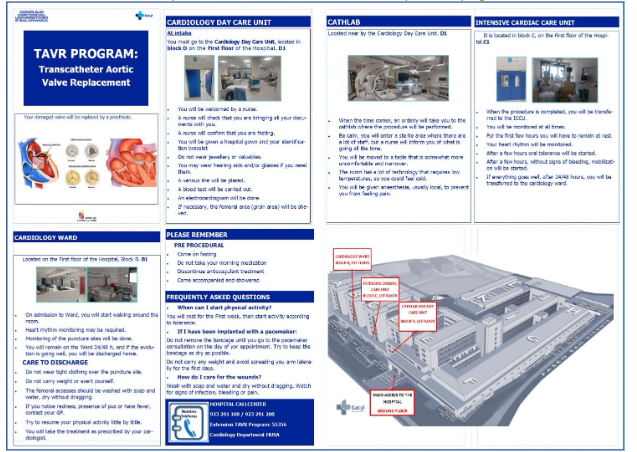
Admission takes place on the day of the TAVR procedure, which reduces hospitalisation time and associated costs. Beforehand, the nurse ensures that test results are included in the patient’s medical history.
Patient and family education is vital to the multidisciplinary team of the TAVR nurse protocol because it allows our patients to become informed patients.
Shared decision making is a pillar of our project and this requires providing good information so that the patient can decide with all the options and weigh up what he or she really needs and wants, because at the end of the day the patient is the centre of the process. TAVR nurse manages the patient’s own motivations and expectations for the procedure, avoiding unfounded expectations, supporting their decisions and planning for early discharge care.
Comprehensive evaluation
The assessment performed by the nurse in the pre-TAVR clinic is holistic. It includes a clinical, functional, psychological and cognitive assessment to determine the suitability of patient selection, facilitate the planning of the TAVR procedure and detect possible sources of complications. The nurse uses validated questionnaires, previously selected by our centre, to assess patient dependence, symptomatology, cognitive function, social and family support, quality of life and frailty. We add self-developed questionnaires on the importance for the patient to be informed, on the patient’s expectations of the treatment and on the early detection of cardiac amyloidosis.
We know that cardiac amyloidosis is frequently associated with AS and results in worse clinical presentation, worse functional capacity and worse survival, leading to a worse prognosis if cardiac amyloidosis is left untreated. Therefore, together with the CAUSA cardiac amyloidosis team, we have designed our own scale for early detection of cardiac amyloidosis in patients with severe AS with indication for TAVR, and if the patient meets the established criteria we refer them to the amyloidosis clinic to confirm or rule out the diagnosis.
The set of clinical and functional results of the multidisciplinary team will be reflected in the TAVR programme report, being the basis for an adequate selection of patients and to reinforce the final decision: TAVR or conservative management. In addition, TAVR nurse collaborates in the management of the waiting list, prioritising the most urgent cases.
| Questionnaires used in the pre-TAVR nurse consultation protocol | Pre TAVR | Post TAVR |
|---|---|---|
| Katz dependency assessment index | x | |
| The New York Heart association NYHA | x | x |
| Gijon social and family support scale | x | |
| Mini mental state examination MMSE | x | |
| Frailty scale Frail | x | |
| EQ5D quality of live scale | x | x |
| Cardiac amyloidosis early detection * | x | |
| Expectations for the procedure * | x | x |
| Importance for the patient of being informed about the process * | x | |
| Check list for pre-selection of patients candidates for early discharge protocol * | x | |
| Patient experience questionnaire on the whole TAVR process * | x |
Abbreviations: TAVR=transcatheter aortic valve replacement.
Admission and follow-up
The TAVR nurse monitors patients from admission to discharge, visiting them in all the care areas where they are treated (cardiology day care unit, catheterisation laboratory, intensive cardiac care unit and hospitalisation unit). The TAVR nurse maintains continuity of care by monitoring the patient’s progress and ensuring ongoing communication with the patient/family as well as the programme team. Prior to discharge, patient and family understanding of medication and discharge care (self-care and symptoms to monitor) is confirmed.
After discharge, the TAVR nurse coordinates the follow-up clinics of patients, combining face-to-face and telephone visits. TAVR nurse schedules post-procedure consultations. Patients who have been part of the early discharge protocol are evaluated in person one week after the procedure. All patients in the programme are scheduled for consultations one month after discharge and after 6 months. The programme was designed with face-to-face consultations, but the patients themselves suggested the possibility of a telephone visit at 6 months if there were no complications, and we have been doing so for more than a year.
Evaluation of patient experience and perceived quality of life in the transcatheter aortic valve replacement procedures.
We assess and measure patient experience throughout the entire process. To this end, we have designed our own experience questionnaire based on patient reported experiences measures (PREMs) and patient reported outcomes measures (PROMs) specific to the TAVR process, which has involved nursing and medical professionals who are experts in the TAVR procedure, in experience questionnaires and in quality of care. Most importantly, the design of this questionnaire has been carried out in co-creation with the contributions of the patient himself, incorporating in our project an active role for the patient, giving importance to public awareness and participation and the need for patient expertise.
The questionnaire takes into account the different stages of the TAVR process to be evaluated: pre-procedure, intra-procedure, post-procedure and follow-up; assessing the treatment received, hospital facilities, shared decision-making process, physical and psychological support, decision-making capacity, information received, communication, considerations with relatives, and continuity of care. Incorporating PREMS and PROMS specific to TAVR allows to quantify the patient’s perspective and how the disease and healthcare impact on the patient. It could allow to evaluate and subsequently improve the quality of care, its effectiveness and cost, help patient follow-up and improve patient experience, empowering the patient in the control of their health. It could have a direct improvement component in healthcare, as it systematises the incorporation by design of the patient’s perspective and voice in the healthcare process and in the healthcare organisation. Taking into account the patient’s experience, therefore, could favour the provision of value for the patient and their family and eliminate that which does not provide value, contributing to the sustainability of the healthcare system.
According to this questionnaire, our patients’ satisfaction was very high in relation to all the evaluated aspects of the TAVR process.
Early discharge
Within the reorganisation of our TAVR programme, an early discharge circuit has also been implemented. The implementation of fast-track TAVR protocols combining minimalist procedure and early post-procedural discharge has shown advantages over traditional models, without being associated with increased readmissions or mortality during follow-up. The increasingly minimally invasive approach of the TAVR procedure, avoiding the use of general anaesthesia, invasive lines, transesophageal echocardiography or endocavitary electrocatheter, has demonstrated a significant reduction in hospital stay, with proven safety and efficacy of early discharge at 24-48 hours post-TAVR. Our FAST TRACK TAVR CAUSA protocol includes inclusion and exclusion criteria, management of selected patients during admission, as well as specific follow-up and outcome measurement. The TAVR nurse is responsible for the pre-selection of patients who are candidates for early discharge through a checklist designed by the team itself and applied by the nurse in the pre-procedural clinic.
Cardiac rehabilitation
As part of the project, we are currently conducting a study on cardiac rehabilitation in patients with severe aortic valve disease undergoing TAVR. The TAVR nurse will perform a screening using a specific scale designed to identify and refer to cardiac rehabilitation programme those patients who will benefit the most, as achieving optimal functional capacity post-procedure is essential.
Benefits of incorporating TAVR nurse role
The TAVR nurse protocol started in our hospital in March 2022. This programme puts the patient at the centre of the process. The TAVR nurse is the point of contact with the patient and family throughout the patient journey, through a facilitator-coordinator role within the multidisciplinary team.
Not all improvements in our project can be attributed to the implementation of this role, but also to the changes and work of the multidisciplinary group. However, the existence of the TAVR nurse figure has a more significant impact on aspects such as how patients perceive the improvement in their quality of life, the importance of education and information, the accompaniment of patients and carers, the doubts resolution, as well as the improvement in the follow-up, their satisfaction and experience of the process.
Regarding the results we have obtained on the benefits of incorporating the TAVR nurse role, we have observed that it improves the patient’s expectations, making them more realistic thanks to a better understanding of their disease and procedure due to the information received. The patient’s experience and satisfaction is very high, the patient reports arriving at the procedure more relaxed, informed and prepared, which helps to reduce anxiety. We are their point of contact pre and post TAVI and this helps them to raise and resolve doubts and provides them with coping strategies. Related to the process and outcomes of the TAVR procedure, our sistematised and multidisciplinary project could help an early detection and prevent complications, reduce readmissions, provide quality and continuity of care, facilitate early discharge, and improve post TAVR patient follow up.
Conclusions
Because the healthcare system is a complex and changing environment, with exponential growth in healthcare expenditure and new technologies, it is necessary to adapt our healthcare to the current situation of population ageing and the increase in chronic diseases, but above all, to the need for person-centred care to make the system sustainable. We must commit to a change in the way we work to improve processes and change the way we relate to patients. At this time of change, a new patient profile has emerged, the “proactive patient”, who wants to participate in their care and their decisions. We must take this advantage to implement patient-centred care models, giving value to the experience of the patient and family, health outcomes and continuity of care, thus responding to the complexity of the patient and their needs. Implementing a culture evaluating results from the patient’s point of view will help us improve quality of care in the TAVR process.
Nursing leadership is a fundamental ingredient to transform and promote initiatives to improve the quality of care. The nurse is present throughout the different phases of the program and interacts with patients and family members, as well as with the rest of the multidisciplinary team involved, so she has a holistic vision, which is essential for improving the TAVR process.
Nurses are at the heart of many multidisciplinary teams and we have to make our nursing work visible and promote it.
Funding Sources
Miryam Gonzalez-Cebrian is funded by a GRS 2860/A1/2023 by Gerencia Regional de Salud of Castilla y León (Spain).
Disclosures
ICG is proctor for Medtronic. The rest of the authors have no conflicts of interest to declare.
Bibliography
- Leon MB, Smith CR, Mack M, et al. Transcatheter aortic-valve implantation for aortic stenosis in patients who cannot undergo surgery. N Engl J Med. 2010;363(17):1597–607. doi: 10.1056/NEJMoa1008232
- Smith CR, Leon MB, Mack MJ, et al. Transcatheter versus surgical aortic-valve replacement in high-risk patients. N Engl J Med. 2011;364(23):2187–98. doi:10.1056/NEJMoa1103510
- Leon MB, Smith CR, Mack MJ, et al Transcatheter or Surgical Aortic-Valve Replacement in Intermediate-Risk Patients. N Engl J Med. 2016;374(17):1609–20. doi: 10.1056/NEJMoa1514616
- Mack MJ, Leon MB, Thourani VH, et al. Transcatheter Aortic-Valve Replacement with a Balloon-Expandable Valve in Low-Risk Patients. N Engl J Med. 2019;380(18):1695–705. doi: 10.1056/NEJMoa1814052
- Reardon MJ, Van Mieghem NM, Popma JJ, et al. Surgical or Transcatheter Aortic-Valve Replacement in Intermediate-Risk Patients. N Engl J Med. 2017;376(14):1321–31. doi: 10.1056/NEJMoa1700456
- Popma JJ, Deeb GM, Yakubov SJ, et al. Transcatheter Aortic-Valve Replacement with a Self-Expanding Valve in Low-Risk Patients. N Engl J Med. 2019;380(18):1706–15. doi: 10.1056/NEJMoa1816885
- Dworakowski R, MacCarthy PA, Monaghan M, et al. Transcatheter aortic valve implantation for severe aortic stenosis-A new paradigm for multidisciplinary intervention: a prospective cohort study. Am Heart J. 2010;160(2):237–43. doi: 10.1016/j.ahj.2010.05.014.
- Thonghong T, De Backer O, Søndergaard L. Comprehensive update on the new indications for transcatheter aortic valve replacement in the latest 2017 European guidelines for the management of valvular heart disease. Open Heart. 2018;5(1):e000753. doi: 10.1136/openhrt-2017-000753.
- Teresa Bastante, Dabit Arzamendi, Javier Martín-Moreiras, et al. Registro español de hemodinámica y cardiología intervencionista. XXXIII informe oficial de la Asociación de Cardiología Intervencionista de la Sociedad Española de Cardiología (1990-2023). Rev Esp Cardiología.2024, ISSN 0300-8932. doi.org/10.1016/j.recesp.2024.07.005.
- Sabaté M, Cánovas S, García E, et al. Colaboradores del Grupo Nacional TAVI. Predictores de mortalidad intrahospitalaria y a medio plazo tras el implante percutáneo de válvula aórtica: datos del Registro Nacional TAVI 2010-2011. Rev Esp Cardiol (Ed. Inglesa) . 2013; 66 : 949–958. doi: 10.1016/j.rec.2013.07.003.
- Núñez-Gil IJ, Elola J, García-Márquez M, et al. TAVI in the learning curve in Spain. In-hospital results compared with aortic valve replacement. REC: CardioClinics. 2021;56(4):242-9.
- Jimenez-Quevedo P, Munoz-Garcia A, Trillo-Nouche R, et al. Time trend in transcatheter aortic valve implantation:an analysis of the Spanish TAVI registry. REC Interv Cardiol. 2020;2:98-105.
- Íñiguez-Romo A, Javier Zueco-Gil J, Álvarez-Bartolomé M, et al. Outcomes of transcatheter aortic valve implantation in Spain through the Activity Registry of Specialized Health Care. REC Interv Cardiol. 2022;4:123-131
- Bohmann K, Burgdorf C, Zeus T, et al. The COORDINATE Pilot Study: Impact of a Transcatheter Aortic Valve Coordinator Program on Hospital and Patient Outcomes. J Clin Med. 2022;11(5):1205.
- De Ronde-Tillmans MJAG, Goudzwaard JA, El Faquir N, et al. TAVI Care and Cure, the Rotterdam multidisciplinary program for patients undergoing transcatheter aortic valve implantation: Design and rationale. Int J Cardiol. 2020;302:36-41. doi:10.1016/j.ijcard.2019.12.005
- McCalmont G, Durand E, Lauck S, et al. Setting a benchmark for resource utilization and quality of care in patients undergoing transcatheter aortic valve implantation in Europe-rationale and design of the international BENCHMARK registry. Clin Cardiol.2021;44:1344–53. doi.org/10.1002/clc.23711
- Wood DA, Lauck SB, Cairns JA, et al. The Vancouver 3M (Multidisciplinary, Multimodality, But Minimalist) Clinical Pathway Facilitates Safe Next-Day Discharge Home at Low-, Medium-, and High-Volume Transfemoral Transcatheter Aortic Valve Replacement Centers: The 3M TAVR Study. JACC Cardiovasc Interv. 2019;12(5):459-469. doi:10.1016/j.jcin.2018.12.020
- Lauck SB, Wood DA, Baumbusch J, et al. Vancouver Transcatheter Aortic Valve Replacement Clinical Pathway: Minimalist Approach, Standardized Care, and Discharge Criteria to Reduce Length of Stay. Circ Cardiovasc Qual Outcomes. 2016;9(3):312-321. doi:10.1161/CIRCOUTCOMES.115.002541
- Lauck SB, Sathananthan J, Park J, et al. Post-procedure protocol to facilitate next-day discharge: Results of the multidisciplinary, multimodality but minimalist TAVR study. Catheter Cardiovasc Interv. 2020;96(2):450-458. doi:10.1002/ccd.28617
- González-Cebrian M, Valverde Bernal J, Bajo Arambarri E, et al. Documento de consenso de la figura de la TAVI Nurse del Grupo de Trabajo de Hemodinámica de la Asociación Española de Enfermería en Cardiología. Enferm Cardiol. 2022;29(86): 5-13.

