Orthognathic Surgery: Enhancing Function & Aesthetics
Orthognathic Surgery for Aesthetic and Functional Outcomes
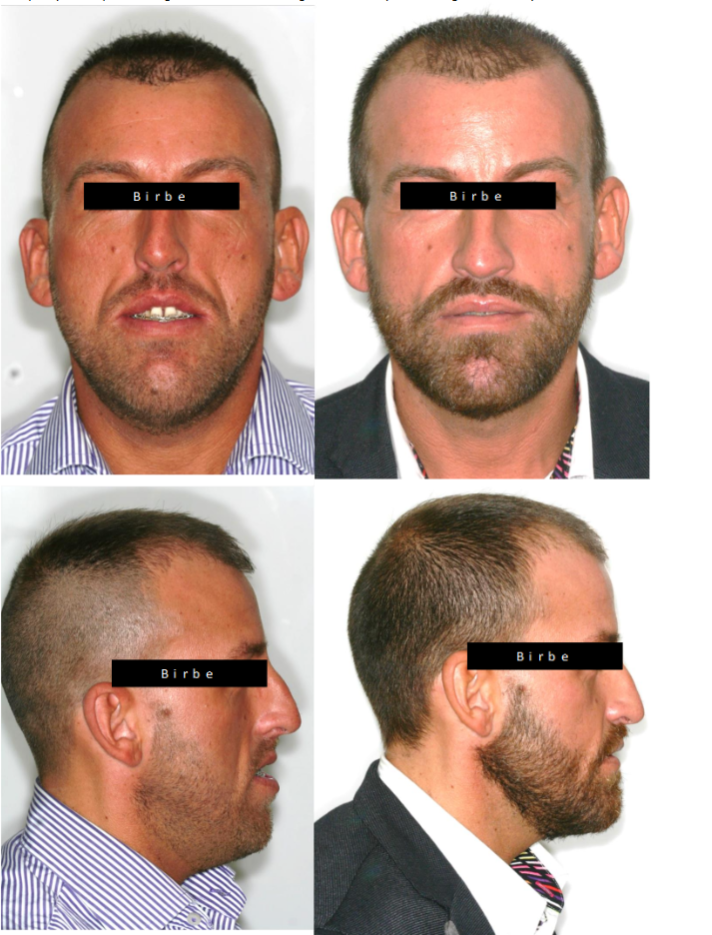
Joan Birbe; MD, DDS, PhD 1
1.Private Practice. Clinica B I R B E, Barcelona, Spain, Maxillofacial and Facial Plastic Surgery
OPEN ACCESS
PUBLISHED: 30 April 2025
CITATION: BIRBE, Joan. Orthognathic Surgery for Aesthetic and Functional Outcomes: A Multidisciplinary Perspective. Medical Research Archives, [S.l.], v. 13, n. 4, apr. 2025. ISSN 2375-1924. Available at: <https://esmed.org/MRA/mra/article/view/6394>.
COPYRIGHT: © 2025 European Society of Medicine. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
DOI: https://doi.org/10.18103/mra.v13i4.6394
ISSN 2375-1924
Abstract
Orthognathic surgery is a cornerstone in the correction of dentofacial discrepancies, offering both functional and aesthetic improvements for patients with skeletal malocclusions and facial asymmetries. This surgical approach requires a multidisciplinary collaboration among orthodontists, maxillofacial surgeons, and rehabilitation specialists to ensure optimal outcomes. This review delves into the comprehensive treatment pathway, beginning with preoperative orthodontic preparation, where dental decompensation and arch coordination play crucial roles. The integration of digital planning tools and virtual surgical simulations has significantly enhanced precision in treatment planning, allowing for customized osteotomies that cater to individual anatomical needs. Beyond skeletal realignment, orthognathic surgery has profound implications for occlusal stability, temporomandibular joint function, airway dynamics, and overall facial aesthetics. The impact of different surgical techniques on obstructive sleep apnea, speech function, and soft tissue response will be explored. Additionally, the review will address postoperative rehabilitation, emphasizing strategies to enhance recovery, minimize complications, and ensure long-term stability. Patient satisfaction remains a critical measure of success, influenced by both objective surgical outcomes and subjective perceptions of facial balance and symmetry. Finally, emerging trends in technology-driven orthognathic surgery, such as artificial intelligence-assisted planning, 3D-printed patient-specific implants, and robotic-assisted osteotomies, will be discussed, providing insight into the future of maxillofacial surgery. By integrating innovative techniques with a patient-centered approach, orthognathic surgery continues to evolve, offering transformative results that extend beyond aesthetics to significantly improve functionality and quality of life.
Keywords
Orthognathic surgery, digital planning, facial aesthetics, temporomandibular joint, airway function, orthofacial surgery
1. Introduction
Orthognathic surgery is a well-established treatment for correcting skeletal discrepancies affecting facial harmony, occlusion, and function. These procedures, which typically involve the maxilla, mandible, and chin, are performed to improve chewing efficiency, speech, airway function, and facial aesthetics.
1.1. HISTORICAL CONTEXT AND EVOLUTION
The origins of orthognathic surgery date back to the early 20th century, but significant advancements in surgical techniques and technology have improved precision, safety, and patient outcomes. Traditional approaches relied on two-dimensional (2D) cephalometric analysis and model surgery, but modern three-dimensional (3D) imaging and virtual surgical planning (VSP) have revolutionized treatment predictability. The Le Fort I osteotomy, introduced as a standard procedure for maxillary repositioning, has undergone modifications to improve skeletal stability and minimize adverse soft tissue effects. Similarly, bilateral sagittal split osteotomy (BSSO) for the mandible has been refined to enhance functional occlusion and TMJ health.
1.2. THE NEED FOR A MULTIDISCIPLINARY APPROACH
Achieving optimal functional and aesthetic outcomes in orthognathic surgery requires a comprehensive, multidisciplinary approach that integrates expertise from various specialists, including orthodontists, maxillofacial surgeons, anesthesiologists, and speech or myofunctional therapists. This collaboration is essential at every stage of treatment, from initial diagnosis to long-term postoperative management, ensuring a harmonized approach that balances skeletal realignment with dental occlusion, soft tissue adaptation, and airway function. One of the fundamental aspects of this interdisciplinary approach is preoperative orthodontic preparation, which ensures that the teeth are properly aligned within their respective arches before surgery. This phase is crucial because it allows the surgeon to reposition the jaws with maximal skeletal and dental harmony, avoiding post-surgical compensations that could compromise long-term stability. Additionally, advancements in digital surgical planning and virtual simulations have revolutionized treatment precision. Through computer-aided design (CAD) and computer-aided manufacturing (CAM) technology, surgeons can predict osteotomy placement, simulate soft tissue responses, and plan three-dimensional (3D) modifications with remarkable accuracy. This digital workflow minimizes intraoperative variability and optimizes patient outcomes by tailoring surgical interventions to individual anatomical needs. Postoperative management is equally important in ensuring long-term stability and patient adaptation. Rehabilitation strategies such as myofunctional therapy and guided physical therapy help retrain the muscles of mastication, the tongue, and the lips, promoting proper function and reducing the risk of relapse. Additionally, continuous follow-up with orthodontists ensures that any minor occlusal refinements can be addressed, enhancing both function and aesthetic balance. The integration of these multifaceted disciplines ultimately enhances the predictability of orthognathic surgery, providing patients with more stable, functional, and aesthetically pleasing results.
1.3. FUNCTIONAL AND AESTHETIC CONSIDERATIONS
Orthognathic surgery is not solely a skeletal intervention; it profoundly affects soft tissue balance, nasal morphology, lip posture, and airway function, making it a critical tool for achieving facial harmony. One of the most noticeable aesthetic effects of jaw repositioning is its impact on nasal shape and structure. For example, maxillary advancement or superior repositioning can alter the nasolabial angle, affect the alar width, and modify the projection of the nasal tip. In some cases, these changes are desirable, but in others, they necessitate concurrent nasal procedures, such as alar cinching or rhinoplasty, to refine the final outcome. Another essential factor is lip position and competence, which directly contribute to facial balance and function. The relationship between the upper and lower lips is influenced by jaw positioning, chin prominence, and muscle tone. Patients with excessive vertical maxillary growth may exhibit lip incompetence, characterized by difficulty in fully closing the lips at rest, leading to strain on the mentalis muscle and an exaggerated gingival display (gummy smile). Conversely, mandibular advancement can enhance lip support and restore a more proportional lower third of the face, improving both aesthetics and oral function. Beyond aesthetics, orthognathic surgery plays a critical role in airway optimization, particularly for patients suffering from obstructive sleep apnea (OSA). Individuals with retrognathia or maxillary hypoplasia often have a narrow airway, predisposing them to airflow obstruction, snoring, and compromised respiratory efficiency. Surgical procedures such as maxillomandibular advancement (MMA) significantly increase airway volume, improving nasal breathing, oxygenation, and overall sleep quality. This functional benefit extends beyond sleep disorders, as improved airway patency enhances daytime energy levels, cognitive function, and cardiovascular health. By addressing both structural and functional considerations, orthognathic surgery serves as a transformative procedure that harmonizes skeletal alignment, enhances soft tissue dynamics, and optimizes airway function, ultimately improving both facial aesthetics and quality of life for patients.
1.4. TECHNOLOGICAL INNOVATIONS AND FUTURE DIRECTIONS
Emerging technologies such as artificial intelligence (AI) in surgical planning, custom patient-specific osteotomy guides, and augmented reality-assisted surgery are shaping the future of orthognathic interventions. By integrating cutting-edge digital tools, enhanced imaging, and minimally invasive techniques, orthognathic surgery continues to evolve, offering patients more predictable and stable outcomes while minimizing complications. Orthognathic surgery is a well-established procedure for correcting skeletal discrepancies affecting facial harmony, occlusion, and function. Traditional surgical planning relied heavily on two-dimensional (2D) cephalometric analysis, but modern advancements in 3D imaging, virtual surgical planning (VSP), and custom osteotomy guides have improved treatment predictability and outcomes. A successful orthognathic treatment requires a multidisciplinary approach, combining orthodontic decompensation, surgical intervention, and postoperative rehabilitation to optimize function and esthetics. This review provides a comprehensive overview of recent innovations, the impact of orthognathic surgery on key functional and aesthetic parameters, and future perspectives.
2. Materials and Methods
This study is a comprehensive literature review based on peer-reviewed journal articles, systematic reviews, and clinical studies obtained from PubMed, Scopus, and Web of Science databases. The search focused on:
- Functional outcomes of orthognathic surgery, including occlusion, TMJ stability, and airway function.
- Aesthetic outcomes related to facial balance, soft tissue adaptation, and gender-affirming modifications.
- Innovations in digital planning, AI-assisted surgical simulations, and long-term stability measures.
Inclusion criteria were:
- Clinical studies published between 2000 and 2024.
- Studies evaluating pre- and post-surgical functional and aesthetic changes.
- Research discussing long-term stability of skeletal modifications.
Exclusion criteria:
- Case reports without sufficient follow-up.
- Studies lacking quantitative or qualitative outcome measures.
Data was analyzed and categorized under functional outcomes, aesthetic implications, and gender-affirming surgical considerations.
MULTIDISCIPLINARY APPROACH IN ORTHOGNATHIC SURGERY
Orthognathic surgery requires a multidisciplinary approach involving orthodontists, maxillofacial surgeons, and other specialists to achieve optimal functional, stable, and aesthetic results. This team must coordinate throughout the three main phases of treatment: pre-surgical orthodontics, surgery, and post-surgical orthodontics.
2.1. PRE-SURGICAL ORTHODONTICS AND INTERDISCIPLINARY PLANNING
Pre-surgical orthodontics plays a fundamental role in preparing the dentition for orthognathic surgery, ensuring that the teeth are properly aligned within their respective skeletal bases. This phase of treatment is essential for achieving optimal occlusion post-surgery, as well as for facilitating precise maxillary and mandibular positioning during the surgical procedure. Traditionally, orthodontic preparation required 12 to 24 months, as it involved correcting dental compensations that had developed to mask underlying skeletal discrepancies. However, advancements in orthodontic techniques and the introduction of the “Surgery First” approach have significantly reduced this timeframe. By prioritizing skeletal correction before orthodontic alignment, this method allows for immediate facial improvement, reduces total treatment duration, and leverages postoperative bone remodeling for accelerated orthodontic movement. The selection of the most appropriate approach depends on the complexity of the case, the severity of skeletal misalignment, and the patient’s specific needs.
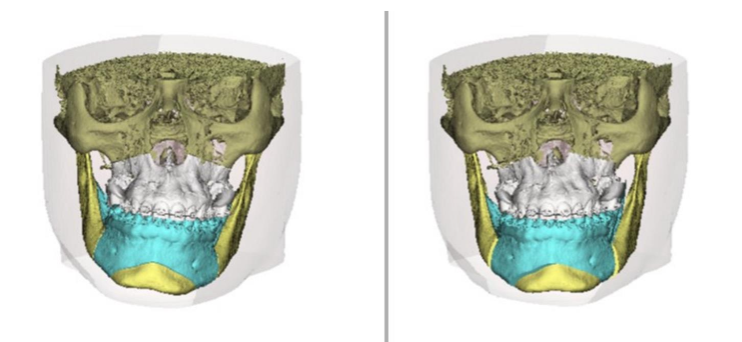
2.1.1. Digital Planning and Computer-Guided Surgery
The integration of cone-beam computed tomography (CBCT) and 3D surgical planning software has revolutionized orthognathic surgery by enhancing diagnostic accuracy and treatment predictability. Unlike traditional methods that relied on two-dimensional cephalometric radiographs and plaster model analysis, digital planning provides a comprehensive three-dimensional view of the craniofacial skeleton, allowing for precise identification of asymmetries, occlusal discrepancies, and airway obstructions. These technologies enable virtual surgical simulations, where osteotomies and bone movements can be planned in a controlled digital environment before being executed in the operating room. One of the key advancements in computer-guided surgery is the use of CAD/CAM (computer-aided design and manufacturing) technology for fabricating surgical splints and patient-specific cutting guides. These tools ensure that bone repositioning is executed with millimetric precision, reducing intraoperative adjustments and improving postoperative stability. Additionally, virtual soft tissue prediction algorithms have improved significantly, allowing both surgeons and patients to visualize the anticipated facial changes before surgery. This level of planning not only enhances surgical accuracy but also increases patient confidence and satisfaction by providing a realistic preview of expected results.
2.2. ORTHOGNATHIC SURGERY: COORDINATION BETWEEN SPECIALISTS
Orthognathic surgery is a highly specialized intervention that requires seamless coordination between orthodontists and maxillofacial surgeons to achieve both functional correction and facial harmony. Unlike conventional dental treatments that focus solely on occlusion, orthognathic procedures reshape the entire facial framework, impacting not only the skeletal structure but also soft tissue dynamics, airway function, and overall aesthetics. The success of the surgery relies on a well-structured preoperative plan, where specialists must collaborate to determine the most appropriate osteotomies, expected skeletal movements, and necessary adjunctive procedures, such as genioplasty or alar base management. This teamwork ensures that both dental occlusion and facial proportions are optimized, providing patients with stable, long-lasting, and natural-looking results.
2.2.1. Modern Surgical Techniques and Their Functional Impact
Contemporary orthognathic procedures employ a range of advanced osteotomies that allow for precise repositioning of the maxilla, mandible, and chin, directly influencing facial form and function. One of the most commonly performed techniques is the Le Fort I osteotomy, which repositions the maxilla to correct vertical, anteroposterior, and transverse discrepancies. This procedure not only restores proper occlusion but also alters nasal morphology, affecting the nasolabial angle, alar width, and nasal tip projection. For mandibular corrections, the Bilateral Sagittal Split Osteotomy (BSSO) is the gold standard for repositioning the lower jaw in cases of Class II or Class III malocclusions. This technique allows for advancement or setback of the mandible, improving jaw projection, bite function, and facial balance. When performed in combination with maxillary surgery, BSSO helps achieve harmonized skeletal relationships, optimizing both functionality and aesthetic appeal. In cases where additional facial contouring is required, genioplasty is frequently incorporated into orthognathic treatment plans. Adjusting the chin’s position—whether through advancement, setback, vertical reduction, or lateral contouring—enhances facial profile symmetry and lower third balance. Genioplasty is particularly useful in refining jawline definition and improving lip competence, which contributes to a more proportionate and natural facial appearance. By integrating advanced surgical techniques with precise interdisciplinary coordination, orthognathic surgery has evolved into a highly customized treatment modality, providing patients with exceptional functional and aesthetic transformations. In many cases, orthognathic surgery is combined with septoplasty or functional rhinoplasty to improve breathing and nasal aesthetics.
2.2.2. Accelerated Orthognathic Surgery and the “Surgery First” Approach
The “Surgery First” protocol represents a major advancement in orthognathic treatment, allowing for immediate surgical correction of skeletal discrepancies without the traditional pre-surgical orthodontic phase. Historically, orthodontic decompensation before surgery required 12 to 24 months, often worsening facial aesthetics in the interim. By contrast, the “Surgery First” approach prioritizes early skeletal correction, followed by post-surgical orthodontic refinement, significantly reducing the total treatment duration from 2-3 years to approximately 12-18 months. A key advantage of this approach is the immediate improvement in facial aesthetics, as patients do not need to undergo the decompensation phase, which can exacerbate occlusal disharmonies. Additionally, post-surgical bone remodeling stimulates accelerated dental movement, facilitating faster orthodontic correction due to the biologic response of the healing period. However, this protocol is not suitable for all cases. Patients with severe occlusal canting, significant transverse discrepancies, or complex asymmetries may still require pre-surgical orthodontic alignment. The success of the “Surgery First” approach depends on advanced digital planning, including precise 3D simulations of skeletal and occlusal relationships, ensuring that skeletal movements are accurately anticipated before surgery.
2.3. POST-SURGICAL ORTHODONTICS AND FUNCTIONAL REHABILITATION
The post-surgical phase plays a vital role in stabilizing occlusion, optimizing function, and refining facial aesthetics. Once skeletal realignment has been achieved, orthodontic intervention is required to ensure proper intercuspation, occlusal harmony, and long-term stability. One of the most widely used methods during this phase is the application of intermaxillary elastics, which help guide jaw positioning and fine-tune occlusion postoperatively. These elastics are crucial in ensuring proper adaptation of soft tissues to the new skeletal structure, reducing the likelihood of relapse. Beyond orthodontic refinement, myofunctional therapy is essential in rehabilitating orofacial muscles, tongue posture, and masticatory function. This is particularly important for patients with severe Class II or Class III discrepancies, where pre-existing muscle imbalances may lead to relapse. Additionally, airway evaluation is necessary for patients treated for obstructive sleep apnea (OSA), ensuring that the surgical intervention has adequately improved airway patency and breathing efficiency. In some cases, complementary procedures, such as nasal surgery or adjustments to CPAP therapy, may be required to further enhance respiratory outcomes. Ultimately, a well-structured post-surgical orthodontic retention protocol is key to maintaining long-term results and preventing relapse.
2.4. THE FUTURE OF THE MULTIDISCIPLINARY APPROACH IN ORTHOGNATHIC SURGERY
The field of orthognathic surgery is undergoing rapid transformation, driven by technological innovations, artificial intelligence (AI), and minimally invasive techniques. The integration of AI-driven diagnostics and predictive modeling is revolutionizing treatment planning, allowing for highly customized surgical protocols that are tailored to individual patient anatomy. AI-based analysis can assess skeletal asymmetries, occlusal relationships, and soft tissue interactions, providing accurate virtual simulations of post-surgical outcomes before the procedure takes place. Additionally, temporary anchorage devices (TADs) and corticotomy-assisted orthodontics are being used to accelerate post-surgical tooth movement, further reducing total treatment time. The development of robotic-assisted surgery and intraoperative navigation is also improving surgical precision, allowing for millimeter-level accuracy in osteotomy execution and reducing intraoperative complications. As digitalization and minimally invasive approaches continue to evolve, the future of orthognathic surgery will become more predictable, efficient, and patient-centered, enhancing both surgical outcomes and patient experience.
3. Functional Considerations in Orthognathic Surgery
Beyond aesthetics, orthognathic surgery plays a critical role in restoring masticatory function, optimizing airway efficiency, and addressing temporomandibular joint (TMJ) disorders. Patients with severe skeletal malocclusions often experience functional impairments, including difficulty in chewing, speech articulation, and proper breathing mechanics. Malocclusions such as Class II and Class III discrepancies can lead to excessive muscular strain, resulting in temporomandibular disorders (TMDs), chronic headaches, and orofacial pain. Additionally, mandibular retrognathia and maxillary deficiency contribute to obstructive sleep apnea (OSA) by restricting pharyngeal airway space. Understanding the functional impact of orthognathic surgery is crucial for developing comprehensive, patient-centered treatment plans that extend beyond cosmetic improvements.
3.1. OCCLUSION AND TEMPOROMANDIBULAR JOINT (TMJ) STABILITY
3.1.1. Relationship Between Dentofacial Deformities and TMD
Patients with dentofacial deformities (DFDs) often suffer from TMJ dysfunction, presenting with joint clicking, pain, limited mandibular mobility, and muscle fatigue. Certain malocclusions are particularly associated with TMD symptoms, including Class II, Division 2 malocclusions, which can lead to condylar compression and increased tension on retrodiscal tissues. Class III malocclusions with anterior interferences place excessive functional stress on the TMJ, while deep overbites and skeletal asymmetries are associated with higher risks of disc displacement and degenerative joint disease.
3.1.2. Impact of Orthognathic Surgery on TMJ Function
The relationship between orthognathic surgery and TMJ dysfunction remains a subject of ongoing debate. While some studies suggest that correcting dentofacial asymmetries and occlusal discrepancies can alleviate TMD symptoms, others indicate that condylar repositioning during surgery may introduce new functional challenges. The specific osteotomy technique used plays a critical role in determining postoperative TMJ function. For instance, the Le Fort I osteotomy, which repositions the maxilla, has minimal direct impact on the TMJ. However, the Bilateral Sagittal Split Osteotomy (BSSO), commonly used for mandibular repositioning, modifies condylar positioning, potentially affecting joint loading. In contrast, the Intraoral Vertical Ramus Osteotomy (IVRO) has been associated with a lower risk of condylar displacement, making it the preferred technique for patients with preoperative TMD. The postoperative adaptation of the muscles of mastication and occlusal refinement are critical factors in determining long-term TMJ function and stability.
3.2. AIRWAY FUNCTION AND SLEEP APNEA MANAGEMENT
3.2.1. Relationship Between Dentofacial Deformities and Obstructive Sleep Apnea (OSA)
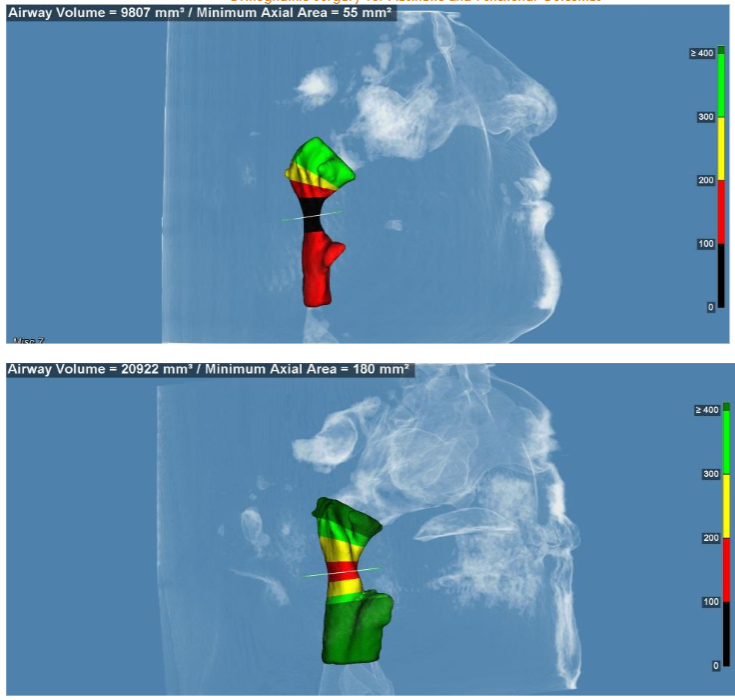
Skeletal discrepancies, particularly maxillary and mandibular retrognathia, have a direct impact on pharyngeal airway space, significantly increasing the risk of obstructive sleep apnea (OSA). When the mandible is positioned posteriorly, the tongue and soft tissues collapse into the airway, causing intermittent airflow obstruction and nocturnal hypoxia. Studies have demonstrated that bimaxillary orthognathic surgery with mandibular advancement effectively expands the upper airway, resulting in a substantial reduction in the apnea-hypopnea index (AHI) and improved oxygen saturation levels.
3.2.2. Maxillomandibular Advancement (MMA) as an OSA Treatment
MMA is considered the gold standard surgical treatment for OSA when CPAP therapy fails. The procedure increases airway volume by repositioning the mandible, maxilla, and associated soft tissues, leading to:
- Expansion of the retropalatal and retroglossal airways.
- Reduction in airway collapse during sleep.
- Improved daytime wakefulness and cognitive function.
- Patients with mandibular deficiency, short face syndrome, and chronic obstructive nasal breathing (CONB) have the highest risk of silent OSA.
3.2.3. Long-Term Outcomes of MMA for OSA
- 91% of patients report no excessive daytime sleepiness (EDS) after surgery.
- Significant reductions in snoring, fatigue, and sleep fragmentation.
- Higher success rates compared to uvulopalatopharyngoplasty (UPPP).
Orthognathic surgery not only improves aesthetics but also enhances airway function, making it an essential intervention for select OSA patients.
3.3. SOFT TISSUE AND NEUROMUSCULAR ADAPTATION
Orthognathic surgery profoundly affects the peri-oral musculature, soft tissue dynamics, and neuromuscular feedback mechanisms, requiring a period of postoperative adaptation. One of the most significant functional changes occurs in tongue posture and movement, particularly after mandibular advancement procedures. When the mandible is repositioned forward, the tongue, which was previously restricted due to skeletal deficiency, must adapt to a new resting position within the oral cavity. This adaptation is crucial not only for speech and swallowing function but also for long-term occlusal stability, as improper tongue posture can contribute to relapse or unintended dental movement. Lip function is also directly impacted by surgical repositioning of the maxilla and mandible, often requiring myofunctional therapy to restore lip competence and muscular equilibrium. Patients undergoing maxillary impaction or mandibular advancements may experience changes in labial seal, which can affect both aesthetic and functional outcomes. Structured rehabilitation programs that include orofacial muscle retraining help mitigate these effects by reinforcing muscle memory and adaptive responses, ensuring a smoother transition to the new skeletal framework. Another important consideration in postoperative adaptation is neurosensory disturbances, particularly in procedures involving the inferior alveolar nerve during mandibular osteotomies. Patients frequently report temporary or permanent alterations in sensation, including paresthesia, hypoesthesia, or dysesthesia, especially in the lower lip, chin, and gingival tissues. The degree of neurosensory recovery depends on nerve handling during surgery, patient-specific healing responses, and the extent of nerve stretching or injury. Over time, many patients experience partial or full sensory recovery, although some may require long-term compensatory strategies to adapt to persistent changes. Ultimately, the success of neuromuscular adaptation after orthognathic surgery relies on muscle memory, occlusal stability, and targeted rehabilitation strategies. Comprehensive post-surgical care, including physiotherapy, orthodontic refinement, and guided muscle re-education, plays a crucial role in ensuring optimal long-term outcomes.
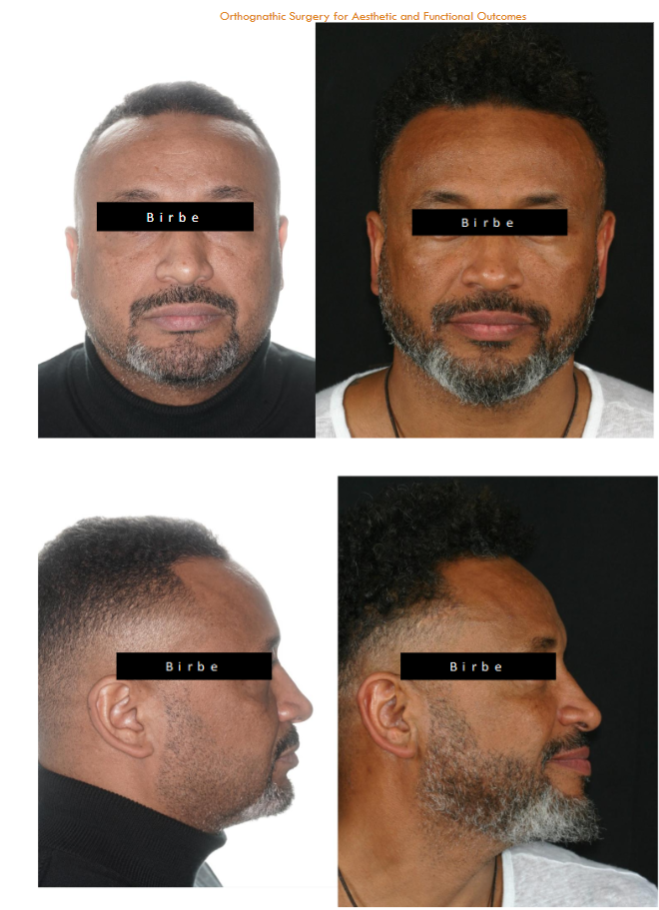
4. Aesthetic Impact of Orthognathic Surgery
Orthognathic surgery extends far beyond skeletal correction, playing a pivotal role in facial aesthetics. The balance of facial proportions, the harmony between soft and hard tissues, and the perception of beauty must be carefully evaluated when planning surgical interventions. Modern volumetric orthofacial surgery focuses on a holistic approach, integrating both skeletal modifications and soft tissue responses to achieve ideal facial balance. Facial aesthetics are not solely determined by bone structure, but rather by the interaction between skeletal movements and soft tissue adaptation. This means that predicting and controlling soft tissue behavior postoperatively is just as crucial as planning the underlying osteotomies. The use of 3D virtual simulations, soft tissue prediction models, and AI-assisted planning has greatly improved the ability to anticipate how the skin, muscles, and fat compartments will respond to surgical changes, enhancing both functional and aesthetic outcomes.
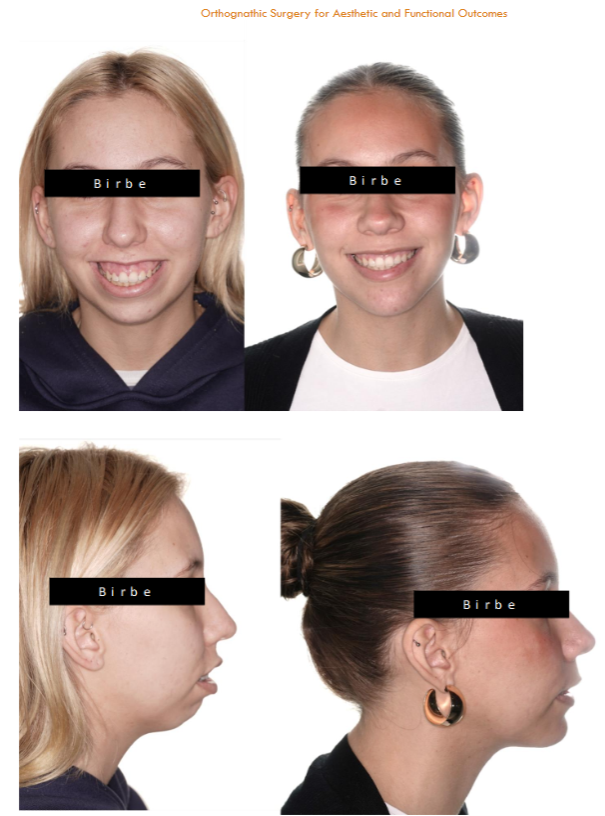
4.1. FACIAL AESTHETICS AND SOFT TISSUE CHANGES
The interaction between skeletal movements and soft tissue adaptation is one of the key factors in achieving harmonious and natural-looking facial results after orthognathic surgery. Various studies have demonstrated predictable soft tissue responses following skeletal repositioning, highlighting the importance of precise planning and individualized treatment approaches. Maxillary advancement, for example, not only improves occlusion and midface projection but also affects the upper lip’s position and nasolabial angle. The forward movement of the maxilla can increase upper lip projection, enhance subnasal support, and influence nasal tip rotation. Since maxillary advancement can also lead to widening of the nasal base, adjunctive procedures such as alar cinch sutures or simultaneous rhinoplasty may be required to prevent undesirable nasal changes. Similarly, mandibular advancements and setbacks directly impact chin prominence and lower lip positioning, with a general 0.6:1 soft-to-hard tissue movement ratio. This means that for every 1 mm of skeletal movement, the overlying soft tissues shift approximately 0.6 mm, although individual variability exists based on skin elasticity, age, and muscle tone. Mandibular setbacks, in particular, must be planned cautiously to avoid excessive soft tissue laxity in the submental region, which can lead to aesthetic concerns such as double chin formation or loss of jawline definition. Vertical maxillary impaction is another procedure with significant aesthetic and functional implications, as it effectively reduces excessive gingival display (gummy smile) while simultaneously improving lip competence and resting posture. However, due to its effect on chin projection and lower facial height, it is often combined with genioplasty to ensure optimal lower-third facial balance. The Le Fort I osteotomy, a common maxillary procedure, can also influence alar base width and nasal appearance. Without proper planning, maxillary movements may result in nasal flaring or excessive widening of the nostrils. To mitigate these effects, techniques such as alar cinch sutures and V-Y closures are employed to preserve the natural proportions of the nasal base. In some cases, a simultaneous rhinoplasty is recommended to achieve ideal nasal aesthetics in conjunction with skeletal modifications. Given the complexity of soft tissue response to orthognathic surgery, meticulous preoperative analysis using 3D virtual simulations and AI-assisted planning is essential to ensure precise aesthetic outcomes. These advancements allow surgeons to predict, control, and refine post-surgical facial changes, providing patients with enhanced facial balance, symmetry, and overall satisfaction.
4.2. Volumetric Orthofacial Surgery: A New Paradigm
The concept of volumetric orthofacial surgery represents a shift beyond traditional cephalometric analysis, emphasizing a global approach to facial balance and proportion. Unlike conventional orthognathic planning, which primarily focuses on skeletal repositioning and occlusal correction, this paradigm considers soft tissue dynamics, facial expressions, and overall three-dimensional harmony. A crucial component of volumetric orthofacial surgery is comprehensive facial analysis, which involves evaluating both static and dynamic aspects of facial movement. This approach considers how soft tissues respond to skeletal modifications, ensuring that adjustments made to the jaw and midface do not create disharmony in surrounding structures. By incorporating dynamic assessments of facial expressions, lip function, and perioral muscle behavior, surgeons can predict postoperative soft tissue adaptation more accurately and refine their treatment plans accordingly. Furthermore, volumetric orthofacial surgery integrates aesthetic adjunctive procedures alongside traditional orthognathic techniques. Procedures such as genioplasty, malar augmentation, and autologous fat grafting (lipofilling) allow for a more customized approach to facial harmony, ensuring that patients achieve not only skeletal correction but also an enhanced aesthetic contour. The use of 3D imaging and digital planning has become essential in this approach, as it enables surgeons to simulate soft tissue responses in real-time and tailor the surgical plan to each patient’s unique anatomy. This integration of advanced imaging, digital simulations, and combined skeletal-soft tissue procedures marks a new era in orthofacial surgery, where achieving natural and harmonious results takes precedence over traditional hard tissue-focused planning.
4.3. NASAL AESTHETICS AND RHINOPLASTY CONSIDERATIONS
Changes in nasal shape and function are common after orthognathic surgery, particularly when maxillary repositioning is involved. The close anatomical relationship between the nasal base, maxilla, and surrounding soft tissues means that modifications in maxillary position can significantly alter nasal projection, width, and airway function. One of the most frequently observed nasal changes is nasal tip rotation and increased columellar show following maxillary impaction. As the maxilla is repositioned superiorly, the nasal tip often tilts upward, resulting in a more pronounced columellar display and potential changes in nasal dorsum contour. This effect must be anticipated in preoperative planning, as excessive nasal tip rotation can create an unnatural aesthetic outcome, sometimes requiring complementary tip-plasty or dorsal contouring. Similarly, maxillary advancements can lead to alar base widening, which may result in a broader nasal appearance. To mitigate this, surgeons often employ alar cinch sutures during surgery to maintain the natural width of the nasal base and prevent excessive lateralization of the nostrils. These suturing techniques, combined with careful nasal base management, are essential in preventing undesirable postoperative nasal flaring. Beyond aesthetics, orthognathic surgery has significant implications for nasal airway function. When combined with functional septoplasty or rhinoplasty, maxillary repositioning can help correct nasal obstructions, improve airflow, and optimize breathing efficiency. Patients with pre-existing nasal deviations, septal spurs, or valve collapse may benefit from simultaneous airway interventions, ensuring that both functional and aesthetic outcomes are maximized. Pre-surgical nasal assessment is crucial in these cases, allowing for a comprehensive, integrated approach that aligns skeletal and nasal modifications for the best possible results.
4.4. THE ROLE OF GENIOPLASTY IN FACIAL AESTHETICS
Genioplasty is a critical adjunctive procedure in orthognathic surgery, as it significantly impacts lower facial aesthetics and balance. The chin serves as a key structural element in determining facial proportion, harmony, and profile alignment, making genioplasty an essential tool in refining surgical outcomes when mandibular repositioning alone is insufficient. One of the most common indications for genioplasty is enhancing chin projection, particularly in cases of mandibular advancement. Patients with retruded mandibles often exhibit microgenia, where the chin remains underdeveloped despite skeletal advancement. By performing a sliding genioplasty, the chin can be advanced independently, ensuring a balanced lower-third facial contour that aligns with the repositioned mandible. In addition to sagittal modifications, genioplasty is frequently used to correct vertical facial imbalances. Patients with vertical maxillary excess or lower facial height discrepancies may require chin augmentation or reduction to restore ideal proportions. Vertical chin lengthening or shortening plays a crucial role in defining the labio-mental angle, influencing soft tissue tension, lip competence, and overall perioral aesthetics. Another significant benefit of genioplasty is its ability to refine the transition between the chin and surrounding soft tissues, particularly in cases where soft tissue laxity is a concern. A well-planned genioplasty can enhance jawline definition, improve cervico-mental angles, and provide structural support to the lower face, contributing to long-term aesthetic and functional stability. Sliding genioplasty offers stable and predictable results, making it the preferred technique for achieving lower facial harmony while maintaining natural soft tissue draping and proportional symmetry.
4.5. THE ROLE OF ORTHOGNATHIC SURGERY IN FACIAL GENDER-AFFIRMING SURGERY
Orthognathic surgery plays a fundamental role in facial gender-affirming surgery, enabling transgender and gender-diverse individuals to achieve facial harmony aligned with their gender identity. For many patients undergoing gender-affirming treatments, skeletal modifications through orthognathic surgery provide permanent and transformative changes, often reducing the need for additional soft tissue procedures.
4.5.1. Feminization Through Orthognathic Surgery
Facial feminization surgery (FFS) often involves modifications to the maxilla, mandible, and chin to create softer, more traditionally feminine contours. The goal is to enhance delicate facial features, reduce angularity, and optimize proportional harmony. Several key surgical techniques contribute to this feminization process: One of the primary interventions in FFS-focused orthognathic surgery is reduction of the mandibular gonial angle, which helps achieve a narrower and more tapered jawline. This is particularly beneficial for transfeminine patients seeking to soften the angularity of the lower face, creating a more slender and oval appearance. Genioplasty also plays a crucial role in facial feminization, as the chin’s shape and projection significantly influence facial aesthetics. In many cases, chin width and height are reduced to achieve a more delicate lower face, enhancing overall facial proportions. Sliding genioplasty or chin narrowing techniques help refine labio-mental curvature and perioral support, contributing to a softer, more elegant facial contour. Additionally, high Le Fort I osteotomy is frequently employed in transfeminine patients to increase anterior malar projection, restoring the feminine ogee curve—a hallmark of high cheekbone prominence and soft midface transitions. This technique helps enhance cheek definition, providing a youthful and balanced aesthetic. Finally, adjusting incisor display and nasolabial angle is a critical step in feminization planning. Properly positioning the maxilla and upper lip ensures a more aesthetically pleasing smile, increasing upper incisor visibility and refining delicate facial expressions. By integrating these skeletal modifications into gender-affirming treatment plans, orthognathic surgery offers lasting, natural feminization, minimizing the reliance on soft tissue contouring or implants.

4.5.2. Masculinization Through Orthognathic Surgery
For transgender men and nonbinary individuals seeking facial masculinization, orthognathic surgery plays a key role in enhancing stronger, more defined skeletal features. Masculinization focuses on reinforcing angularity, increasing jawline definition, and establishing a proportionally dominant lower third of the face. Since facial structure is one of the most defining elements of gender perception, orthognathic procedures can significantly enhance masculine characteristics, complementing hormonal therapy and additional gender-affirming procedures. One of the most important modifications in masculinization surgery is mandibular advancement, which not only improves occlusion and airway function but also contributes to a stronger, more projected jawline. This is often combined with increasing gonial angle prominence, which helps create a square, well-defined mandibular contour—a key feature of traditionally masculine facial aesthetics. By enhancing gonial flare and lateral projection, surgeons can accentuate the width and strength of the jaw, reinforcing masculine proportions. Genioplasty also plays a crucial role in facial masculinization, as the chin is a defining structure in the lower face. Chin augmentation procedures aim to create a broader and more pronounced lower third, often through horizontal advancement and transverse widening. This contrasts with feminization genioplasty, which typically involves narrowing and reducing chin height. A well-executed masculinization genioplasty enhances the vertical height and anterior projection of the chin, reinforcing a strong lower facial profile. Another key adjustment in masculinization-focused orthognathic surgery is maxillary repositioning, particularly in cases where excessive incisor display creates a more delicate, traditionally feminine appearance. Reducing upper incisor exposure helps achieve a more balanced, proportional midface, shifting the aesthetic focus toward the lower third of the face. Additionally, counterclockwise rotation of the occlusal plane is frequently employed to establish stronger lower face dominance, emphasizing jaw projection and angularity. By integrating these structural modifications, orthognathic surgery provides a durable and natural masculinization effect, often reducing the need for extensive soft tissue procedures. When combined with forehead contouring, rhinoplasty, and jawline augmentation, these changes contribute to a cohesive, masculinized facial profile.
4.5.3. The Importance of Personalized Gender-Affirming Planning
With approximately 5.1% of young adults undergoing orthodontic treatment identifying as gender diverse, the need for inclusive, patient-centered planning in orthognathic surgery is more important than ever. Gender-affirming orthognathic surgery requires a highly individualized approach, as each patient has unique facial aesthetic goals that align with their gender identity. To achieve the most natural and satisfying results, surgeons must engage in comprehensive discussions with patients about their expectations, ensuring that both functional and aesthetic needs are met. One of the most significant advancements in gender-affirming facial surgery is the use of 3D planning and AI-assisted modeling, which allows both surgeons and patients to visualize potential post-surgical outcomes before committing to a specific treatment plan. Digital simulations help predict skeletal changes, soft tissue adaptation, and overall facial balance, providing greater precision and patient involvement in the decision-making process. These technologies have revolutionized facial gender-affirming surgery, allowing for a customized approach that considers individual anatomical differences and gendered aesthetic preferences. Beyond skeletal modifications, integrating both hard and soft tissue procedures is essential for achieving optimal facial harmony. While orthognathic surgery provides structural changes to the jaw, chin, and midface, complementary soft tissue refinements such as fat grafting, lip contouring, or soft tissue augmentation can further enhance gender-specific facial features. The combination of skeletal repositioning and soft tissue procedures ensures a holistic transformation, helping patients achieve a facial structure that aligns seamlessly with their identity.
4.6. THE FUTURE OF AESTHETIC ORTHOGNATHIC SURGERY
The field of aesthetic orthognathic surgery is evolving rapidly due to technological advancements, including 3D imaging, AI-driven surgical planning, and minimally invasive techniques. These innovations are redefining treatment precision, surgical efficiency, and aesthetic predictability, ensuring that patients achieve highly customized and stable results. One of the most promising developments is automated AI analysis, which assists in aesthetic treatment planning by identifying ideal facial proportions, skeletal asymmetries, and soft tissue behavior. AI-driven algorithms can suggest optimal jaw positioning, occlusal plane orientation, and chin augmentation techniques, helping surgeons refine their preoperative strategies. Additionally, the introduction of 3D-printed patient-specific implants has allowed for customized skeletal modifications, enhancing postoperative stability and contour refinement. Another transformative trend is the incorporation of augmented reality (AR)-assisted surgery, which enhances soft tissue management and surgical execution. Surgeons can use real-time AR overlays to visualize underlying anatomical structures, improving precision during osteotomies and soft tissue repositioning. These technological advancements are setting a new standard for orthognathic surgery, enabling more accurate predictions of post-surgical outcomes and significantly enhancing patient satisfaction and long-term aesthetic stability.
4.7. SELF-ESTEEM AND PERSONALITY CHANGES AFTER ORTHOGNATHIC SURGERY
Orthognathic surgery has been shown to produce profound psychological benefits, particularly in self-esteem, self-confidence, and social perception. Since facial appearance plays a crucial role in social interactions, changes in facial structure and harmony can have a significant impact on mental well-being. Research has demonstrated that patients who undergo bimaxillary or chin orthognathic surgery often experience positive shifts in personality perception, with observers rating them as more trustworthy, friendly, intelligent, and attractive. A study conducted by Posnick and Kinard used crowdsourced evaluations of preoperative and postoperative facial images, revealing that patients were perceived as happier and more approachable after surgery. There was a marked reduction in negative facial expressions, with patients appearing less angry, sad, or afraid, reinforcing the psychosocial benefits of facial harmony. Furthermore, patients frequently reported an increase in social confidence and a greater sense of self-assurance in interpersonal interactions, demonstrating the emotional impact of orthognathic procedures beyond their physical transformations. These findings underscore the importance of a holistic approach in orthognathic surgery, where both functional and psychological aspects are taken into account during treatment planning. By prioritizing patient expectations, facial balance, and natural aesthetic outcomes, orthognathic surgery can achieve not only anatomical correction but also meaningful improvements in quality of life.
5. Conclusion
Orthognathic surgery is a transformative intervention that enhances both function and aesthetics by correcting skeletal malocclusions, airway deficiencies, and facial disharmony. Over the years, advancements in digital planning, 3D imaging, and AI-assisted surgical simulations have significantly improved the predictability and precision of these procedures. The integration of volumetric orthofacial surgery ensures a holistic approach, balancing skeletal corrections with soft tissue adaptations to achieve natural and harmonious facial aesthetics. Additionally, incorporating genioplasty, rhinoplasty principles, and alar base management into orthognathic planning has allowed for more comprehensive facial optimization. Beyond aesthetics, orthognathic surgery plays a crucial role in airway optimization, particularly for patients with obstructive sleep apnea (OSA). Maxillomandibular advancement (MMA) has been proven to enhance nasal airflow, increase airway volume, and reduce reliance on CPAP therapy, improving overall quality of life. By addressing skeletal factors contributing to airway obstruction, orthognathic surgery has emerged as a key intervention in preventative medicine, reducing risks associated with cardiovascular disease, metabolic disorders, and chronic fatigue. Long-term stability has also improved due to rigid internal fixation (RIF), AI-driven predictive modeling, and innovative orthodontic protocols, reducing relapse rates and ensuring sustainable functional outcomes. The future of orthognathic surgery lies in continued technological innovation and personalized treatment. AI-driven diagnostics, bioactive implants, and minimally invasive techniques are shaping the next generation of procedures, prioritizing precision, faster recovery, and long-term stability. The shift toward preventive and airway-centric surgery underscores the expanding role of orthognathic procedures beyond aesthetics, reinforcing their impact on overall health and wellness. As the field embraces patient-centered innovations and interdisciplinary collaboration, orthognathic surgery will continue to push boundaries, offering life-changing results through enhanced function, facial harmony, and improved well-being.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Birbe J. Classical planning in orthognathic surgery. Rev Esp Cir Oral Maxilofac. 2012.
- Birbe J, Serra Serrat M. Orthodontics in orthognathic surgery. RCOE. 2006;11(5-6):547-557.
- Posnick JC. Orthognathic Surgery: Principles and Practice. St. Louis, MO: Elsevier; 2014.
- Wang Y, Lee Y, Baek SH. Surgery-first approach in Class III treatment: Systematic review of outcomes. Am J Orthod Dentofac Orthop. 2015;148(3):401-415.
- Miloro M, Han MD, Kwon TG, Xi T, Borba AM, Reyneke JP, Caminiti M. Predicting the future focus of orthognathic surgery: Outcome-driven planning and treatment with function, aesthetics, and occlusion as key indicators. J Oral Maxillofac Surg. 2024;82(6):1329-1335.
- Raffaini M, Cocconi R, Spinelli G. Simultaneous rhinoseptoplasty and orthognathic surgery: outcome analysis of 250 consecutive patients using a modified Le Fort I osteotomy. Aesthetic Plast Surg. 2018;42(5):1090-1100.
- Villegas, C. U. F. S., Uribe, F., Sugawara, J., & Nanda, R. (2010). Expedited correction of significant dentofacial asymmetry using a “surgery first” approach. J Clin Orthod, 44(2), 97-103.
- Nordblom NF, Büttner M, Schwendicke F. Artificial intelligence in orthodontics: critical review. J Dent Res. 2024;103(6):577-584.
- Nadershah M, Mehra P. Orthognathic surgery in the presence of temporomandibular dysfunction: what happens next? Oral Maxillofac Surg Clin North Am. 2015 Feb;27(1):11-26.
- Birbe J, Costa de la Higuera C. Orthognathic surgery and its influence in the temporomandibular joint. Rev Esp Ortod. 2011;41:133-142.
- Goodday R. Diagnosis, treatment planning, and surgical correction of obstructive sleep apnea. J Oral Maxillofac Surg. 2009;67:2183-2196.
- Posnick JC, Adachie A, Singh N, Choi E. Silent sleep apnea in dentofacial deformities and prevalence of daytime sleepiness after orthognathic and intranasal surgery. J Oral Maxillofac Surg. 2018;76:833-843.
- O’Ryan F, Lassetter J. Optimizing Facial Esthetics in Orthognathic Surgery Patients. J Oral Maxillofac Surg. 2011;69:702-715.
- Ruggiero F, Borghi A, Bevini M. Soft tissue prediction in orthognathic surgery: improving accuracy by means of anatomical details. PLoS ONE. 2023;18(11):e0294640.
- DeSesa CR, Metzler P, Sawh-Martinez R, Steinbacher DM. Three-dimensional nasolabial morphologic alterations following Le Fort I. Plast Reconstr Surg Glob Open. 2016;4(8):e848.
- Sun AH, Steinbacher DM. Orthognathic surgery and rhinoplasty: simultaneous or staged? Plast Reconstr Surg. 2018;141(2):322-329.
- Posnick JC. Sequencing of Orthognathic Procedures: Step-by-Step Approach. In: Orthognathic Surgery: Principles and Practice. Elsevier; 2014:441-448.
- Joan Birbe Foraster, Barbara Anento Moreno, Enric Bardalet Casals, Teresa Flores Fraile, Emilio Macias Escalada. Dysplasies faciales verticales: diagnostic, plan de traitement et thérapeutique. L’Orthodontie Française. 2010;81(4):301-314. doi:10.1051/orthodfr/2010027.
- Fisher EL, Morrison S, Susarla SM, Ettinger R. Planning the Cut: Gender-Affirming Considerations in Orthognathic Surgery. J Oral Maxillofac Surg. 2024 Nov;82(11):1343-1346. doi: 10.1016/j.joms.2024.07.017.
- Farkas LG, Munro IR (eds): Anthropometric facial proportions in medicine. Charles C Thomas, 1987, p 344.
- Raffaini M, Perello R, Tremolada C, Agostini T. Evolution of Full Facial Feminization Surgery: Creating the Gendered Face With an All-in-one Procedure. J Craniofac Surg. 2019 Jul;30(5):1419-1424.
- Liebregts J, Xi T, Schreurs R. Three-dimensional virtual simulation of alar width changes. Int J Oral Maxillofac Surg. 2016;45(10):1315-21.
- Posnick JC, Kinard BE. Orthognathic surgery has a significant positive effect on perceived personality traits and perceived emotional expressions in long face patients. J Oral Maxillofac Surg. 2019;77(3):408.e1-408.e10.
- Posnick JC, Kinard BE. Orthognathic surgery and perceived personality changes. J Oral Maxillofac Surg. 2019;77(3):408.e1-408.e10.
- Brandtner C, Hachleitner J, Rippel C, Krenkel C, Gaggl A. Long-term skeletal and dental stability after orthognathic surgery of the maxillo-mandibular complex in Class II patients with transverse discrepancies. J Craniomaxillofac Surg. 2015 Oct;43(8):1516-21. doi: 10.1016/j.jcms.2015.07.007. Epub 2015 Jul 26. PMID: 26293193.

