Personalized Rehabilitation for Severely Compromised Dentition
Reconstruction of a Severely Compromised Dentition: A Personalized Approach to Restoring Function, Stability, and Esthetics
Ahmad Soolari, DMD, MS 1 and Amin Soolari, DDS, FAGD 2
- Dental consultant: Soolari Dentistry, 11251 Lockwood Dr., Silver Spring, MD 20901
- Postgraduate Periodontics Department, University of Florida, Gainesville, Forida, USA
OPEN ACCESS
PUBLISHED: 30 September 2025
CITATION: Soolari, A., and Soolari, A., 2025. Reconstruction of a Severely Compromised Dentition: A Personalized Approach to Restoring Function, Stability, and Esthetics. Medical Research Archives, [online] 13(9). https://doi.org/10.18103/mra.v13i9.6881
COPYRIGHT: © 2025 European Society of Medicine. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
DOI https://doi.org/10.18103/mra.v13i9.6881
ISSN 2375-1924
ABSTRACT
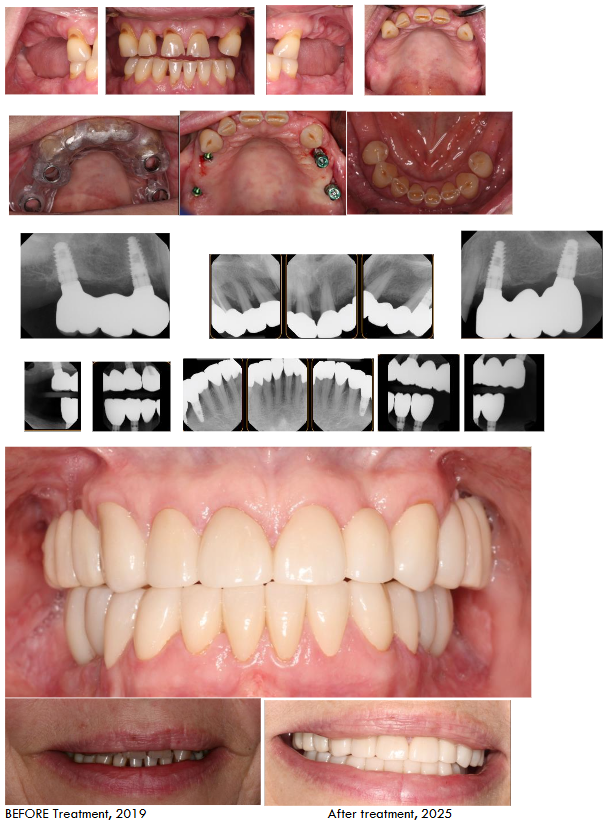
This case report details the successful rehabilitation of a 53-year-old female patient presenting with a severely compromised dentition due to advanced periodontal disease, posterior bite collapse, and dental neglect. A personalized treatment plan, deviating from the classic “All-on-4” approach, was implemented. The strategy focused on patient education, bacterial load reduction, ridge augmentation, strategically placed implants, and retention of select natural teeth in the mandible and maxilla. This approach prioritized long-term stability, function, and esthetics, resulting in significant improvements in the patient’s oral health, overall well-being, and self-confidence. Five years of post-treatment, the patient remains highly satisfied with the outcome.
Keywords: Severe Periodontal Disease, Implant-Supported Prosthesis, Personalized Dentistry, Full Mouth Rehabilitation
Introduction
A severely compromised dentition includes but not limited to severe worn-out dentition, periodontal disease, endodontic involvement, carious lesions, unreplaced missing teeth, migration of teeth, ridge deformity, gingival deformity, infected teeth, loss of vertical dimension, defective/ failing restorations, shrinking jawbones, teeth mobility, pathological migration of teeth and occlusal disharmony. The aim of treatment is formulating a personalized treatment planning, to address full-mouth reconstruction (FMR) to restore function, stability, speech and esthetics. Producing stable long-term results requires a thorough review of medical and dental history to reduce systemic impact on oral health such as diabetes, xerostomia, smoking, cancer treatment, osteoporosis and drug abuse.
Severe periodontal disease can lead to significant functional and esthetic impairment, impacting a patient’s quality of life. Rehabilitation of such cases requires a comprehensive approach addressing not only the immediate dental issues but also contributing factors such as patient education, systemic health considerations, and psychological well-being. While the “All-on-4” concept offers a streamlined approach for full-arch rehabilitation, it may not always be the optimal solution for every patient. This case report presents an alternative, personalized treatment strategy for a patient with a severely compromised dentition, emphasizing long-term stability, preservation of natural tooth structure where possible, and patient satisfaction.
Case Presentation
A 53-year-old Caucasian female presented with a chief complaint of difficulty smiling, chewing, and speaking. Clinical examination revealed severe generalized periodontitis, posterior bite collapse, and multiple failing teeth. Radiographic evaluation confirmed significant alveolar bone loss and compromised tooth support. The patient’s medical history included vaping, anxiety, arthritis, osteopenia, and headaches. This complex medical history, coupled with the patient’s dental neglect, highlighted the need for a multidisciplinary approach involving collaboration with the patient’s physician and a focus on mitigating risk factors.
Treatment Planning and Execution
A comprehensive treatment plan was developed in consultation with the patient and her physician. The initial phase focused on patient education regarding the etiology and progression of periodontal disease, emphasizing the crucial role of oral hygiene and smoking cessation. Non-surgical periodontal therapy, including scaling and root planning utilizing the Parkell Turbo Sensor, was initiated to reduce the bacterial load and improve periodontal health. Due to the extent of periodontal involvement, most posterior teeth and several maxillary anterior teeth were deemed non-restorable and carefully extracted. Simultaneous ridge augmentation procedures using particulate bone (OraGraft, mineralized cortical Bone from the LifeNet) and membrane (Renovix-Plus from the Salvin) were used to optimize the bone volume for future implant placement followed by flap closure with 4.0 monofilament sutures (Salvin FS-3 Cyto Surge).
Transitional removable prostheses were delivered to restore immediate function and esthetics during the healing phase.
Four months later, after adequate healing and bone consolidation, 3D imaging taken by CareStream 9300 and surgical stent made by 3D Diagnostix Inc) used for strategically placing implant to support a fixed prosthesis (Implant Direct Legacy 2). Critically, in the mandible, the anterior teeth, while exhibiting some bone loss, demonstrated sufficient structural integrity and clinical attachment after thorough periodontal treatment. Therefore, a decision was made to retain these teeth, deviating from the “All-on-4” concept. This conservative approach aimed to preserve natural tooth structure, proprioception, and potentially improve the long-term stability of her teeth. The treatment sequence also considered the patient’s osteopenia and arthritis, favoring a less invasive approach where clinically justified.
Prosthetic Rehabilitation
Following implant osseointegration in the maxilla, final impressions were taken (Paradigm VPS Impression Materials from Darby Dental), for fabrication of implant-supported fixed prostheses. For conventional crown and bridges followed the zirconia guidelines and provisional prepared by lab. Prep done using course tapered diamond bur at high speed. Cemented crown and bridges using permanent cement (RMGI Nexus Cement).
The mandibular anterior teeth were incorporated into the overall treatment plan and meticulously monitored for periodontal stability throughout the treatment and follow-up periods. The prostheses were designed to provide optimal function, esthetics, and comfort, while also facilitating effective oral hygiene practices. The patient received comprehensive oral hygiene instruction, emphasizing the importance of meticulous plaque control around both implants and natural teeth for long-term success.
Post-Treatment Follow-up and Outcome
The patient has been followed up for five years post-treatment. She has expressed high satisfaction with the functional and esthetic outcomes. She reports significant improvement in chewing ability, enhanced self-confidence, and a renewed ability to smile comfortably. Importantly, she has successfully discontinued vaping, demonstrating a commitment to improving her overall health. Her arthritis and osteopenia are being actively managed by her physician. The retained teeth have remained stable with regular periodontal maintenance, showing no signs of progressive bone loss or attachment loss. No biological or technical complications related to the implants or prostheses have been observed except for lower terminal implants in the third-year post treatment. The periimplantitis is treated like natural treat by flap elevation and debridement including regenerative periodontal therapy. The key to her successful is her commitment to three month recalls.
Discussion
This case highlights the importance of a personalized approach to the rehabilitation of severely compromised dentitions. While the “All-on-4” concept offers a predictable and efficient solution for many patients, it is essential to consider individual patient needs and circumstances. In this case, the decision to retain some teeth with periodontal treatment and augment the ridges prior to implant placement contributed to a more conservative and potentially more stable long-term outcome. Preserving natural teeth, where clinically sound, can offer advantages in terms of proprioception, psychological well-being, and potentially long-term maintenance of alveolar bone. The collaborative approach involving the patient’s physician ensured that the treatment plan was tailored to her specific medical conditions and risk factors. The patient’s successful smoking cessation underscores the importance of patient education and motivation in achieving long-term oral health improvements. The long-term success of this case emphasizes the significance of meticulous treatment planning, precise surgical and prosthetic execution, and ongoing maintenance in achieving predictable and satisfying results for patients with complex dental needs.
Conclusion
This case suggests that a personalized treatment approach, deviating from the classic “All-on-4” concept, can effectively restore function, stability, and esthetics in patients with severely compromised dentitions. By prioritizing patient education, addressing contributing systemic factors, and utilizing a combination of implant-supported prostheses and strategic retention of natural teeth, long-term success can be achieved, leading to significant improvements in the patient’s oral health, overall well-being, and quality of life. This case reinforces the importance of comprehensive assessment, interdisciplinary collaboration, and patient-centered care in the management of complex dental cases.
Authorship
Dr. Ahmad Soolari is a Diplomate of the American Board of Periodontology. He has a Postdoc Certificate in Periodontics from the Eastman Institute for Oral Health and a MS degree from the University of Rochester, Rochester, New York. Dr. Soolari is a former faculty at the New York University and the University of Maryland postdoctoral residency program. Dr. Soolari has published numerous articles in medical and dental journals. He operates a specialty practice in the Silver Spring, and Potomac area of Montgomery County, Maryland, USA.

References
- Tonetti MS, Greenwell H, Kornman KS. Staging and grading of periodontitis: Framework and proposal of a new classification and case definition. J Periodontol. 2018;89(Suppl 1):S159–S172.
- Sanz M, et al. Periodontitis and peri-implant diseases and conditions: Consensus report of the 2017 World Workshop. J Clin Periodontol. 2018;45(Suppl 20):S282–S385.
- Schimmel M, et al. Step-by-step approach for terminal dentition: Extraction, implants, or restoration? J Prosthodont Res. 2024;68(2):145–154.
- Simonelli, A et al. Minimal invasiveness in the surgical treatment of intraosseous defects: A systematic review. Periodontol 2000 2023 Feb;91(1):20-44.
- Maló P, Nobre A, Lopes A, Ferro A, Petrie A. “All-on-four” immediate-function concept for rehabilitation of the edentulous maxilla: a 5-year retrospective study. Clin Implant Dent Relat Res. 2011;13(4):e239-e249.
- Tonetti MS, Greenwell H, Kornman KS. Staging and grading of periodontitis: current concepts and implications for case definitions. J Periodontol. 2018;89 Suppl 1:S2-S19.
- Cobb CM, Scottosanti BF. The role of calculus in the etiology of periodontal disease. Periodontol 2000 2020;84(1):108-120.
- Zhang, H et al. Assessment of soft and hard tissue characteristics of ridge preservation at molar extraction sites with severe periodontitis: a randomized controlled trial. BMC Oral Health. 2022 Nov 17;22(1):511.
- Zaninovich, M. et al. Classification system for maxillary fixed dental prostheses. J Periodont. 2024 Dec;33(9):852-860.
- Cortellini P, Et al. Periodontal regeneration versus extraction and dental implant or prosthetic replacement of teeth severely compromised by attachment loss to the apex: A randomized controlled clinical trial reporting 10-year outcomes, survival analysis and mean cumulative cost of recurrence. J Clin Periodontol. 2020 Jun;47(6):768-776.
- Campanile VM, Et al. Risk factors for recurrence of periodontal disease in patients in maintenance care in private practice. J. Clin Periodontol. 2019 Sep;46(9):918-926.
- Soares PM Etal. Maintenance protocols for implant-supported dental prostheses: A scoping review. J Prosthet Dent. 2024 Jul;132(1):59-71.

