Revising Alopecia Areata Classification and Scoring
Alopecia areata – need for a revision in morphological classification and scoring
Imran Majid1*, Insha Latif2, Areeb Imran3
- Director, Cutis Institute of Dermatology, Srinagar Kashmir.
- Consultant Dermatologist, Cutis Institute of Dermatology, Srinagar Kashmir.
- MBBS Student, Newcastle University, UK.
OPEN ACCESS
PUBLISHED: 30 June 2025
CITATION Majid, I., Latif, I., Imran, A., 2025. Alopecia areata – need for a revision in morphological classification and scoring. Medical Research Archives, [online] 13(6). https://doi.org/10.18103/mra.v13i6.6708
COPYRIGHT © 2025 European Society of Medicine. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
DOI https://doi.org/10.18103/mra.v13i6.6708
ISSN 2375-1924
ABSTRACT
Background: Scalp hair is believed to be the commonest site involved in Alopecia Areata (AA), and the morphological classification and scoring of the disease mainly concentrate on scalp hair involvement.
Objectives: This study aims to assess terminal hair involvement across different body sites in patients with alopecia areata (AA), evaluate the current classification and scoring systems, and propose potential revisions and solutions.
Methods: Data of patients of AA registered over 4 years at our institute from April 2021 to March 2025 was analyzed for the site(s) of involvement, morphological type of disease, and associated cutaneous/medical disorders. The data was analyzed to assess whether all the patients could be classified into any one of the currently known morphological types and scored in an ideal fashion.
Results: A total of 1010 patients with alopecia areata (AA) were seen over 4 years, including 602 males and 408 females. Scalp involvement alone was observed only in 488 patients (48.3%) patients while 522 patients (51.7%) had terminal hair involvement beyond the scalp. Among the 602 males, 394 were older than 18 years, and in this subgroup, approximately 63% (248/394) had beard hair involvement, either alone or along with scalp hair. The multifocal type was the most common morphological pattern of AA observed. However, some patients with extensive involvement of the scalp, beard, and body hair could not be classified into any known morphological type. For this pattern, we propose the term alopecia subuniversalis.
Conclusions: Given that beard hair is affected as commonly as scalp hair, we propose the use of a composite scoring system to assess the severity of alopecia areata (AA) involving the beard, eyebrows, and eyelashes. Additionally, we propose a new morphological subtype—alopecia subuniversalis—to describe scalp AA with extensive involvement of the other hair-bearing areas of the face and body.
Keywords: Alopecia Areata, Epidemiology, Classification, Scoring, Objective assessment, SALT score, AASI score, Alopecia subuniversalis.
INTRODUCTION
Alopecia areata (AA) is a common hair disorder with a lifetime prevalence of approximately 2% in the general population.¹ The disease is presumed to have an autoimmune pathogenesis and can affect individuals of all age groups.2,3 AA is divided into many morphological types depending upon the severity of the disease and the distribution of lesions. These morphological subtypes include focal AA (single patch), multifocal AA (multiple patches on single or more areas), Alopecia Subtotalis, Alopecia Totalis, Alopecia Universalis, diffuse AA, Ophiasis and Sisaipho types.1 AA involves both genders and has a worldwide distribution. Scalp is considered the most commonly affected site in AA. In fact, most clinical studies assess disease severity primarily based on scalp involvement.1,2
The ‘Severity of Alopecia Tool’ (SALT) score is the most widely used scoring system to evaluate severity of disease and treatment outcomes in AA. This scoring system assesses the severity of scalp hair involvement on 4 different areas of the scalp and quantifies the severity individually on these 4 areas. The total SALT score is then calculated by adding the scores from all 4 areas of the scalp. Almost all clinical studies use SALT score as the objective scoring system to assess disease severity and treatment outcome in AA. SALT score, as described above, focuses almost exclusively on scalp involvement and does not take any other hair-bearing area into account.⁴ There are a few other scoring systems that are employed in AA which include Alopecia Density and Extent (ALODEX) score, Alopecia Areata Progressive Index (AAPI) score, Alopecia Areata Predictive score and SBN score.5-7 A review of existing clinical studies and the scoring systems reveals a consistent emphasis on scalp AA, often overlooking involvement of other hair-bearing sites. There are some scoring systems available for assessing the beard hair, eyelash and eyebrow involvement but none of these scores is comprehensive enough to assess the disease severity as a whole.8-9
In clinical practice, patients frequently present with AA affecting other cosmetically significant areas, such as the beard, eyebrows, and eyelashes, sometimes in combination with scalp hair involvement and sometimes in isolation as well. These patients experience psychological distress comparable to those with scalp involvement.10-11
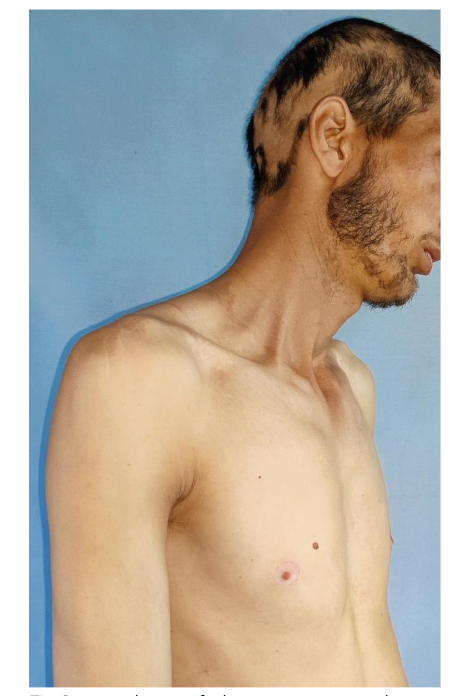
In addition to the individual site of involvement, the severity of AA may vary from one site to another. In some cases, scalp may be more severely involved than the other areas or conversely, the scalp hair may be less involved than the other sites. Thus, there is a subset of patients in whom the scalp hair involvement is significantly less in comparison with the involvement of hair beyond the scalp. Many of these patients have complete or almost complete loss of eyebrows, eyelashes and/or body hair with a limited involvement of scalp hair (Figure 1). Such patients cannot be classified into any of the documented morphological types of AA as outlined above.

METHODS
This is a retrospective data analysis study that was conducted at our institute in April 2025. Data of all AA patients registered with us over 4 years, from April 2021 to March 2025 was analyzed. Diagnosis of AA in all these patients was made by a board certified dermatologist with >20 years of clinical experience (Author 1) and supplemented by dermoscopic examination. All these patients had attended the out-patient department of the institute over 4 years. Data pertaining to demography, morphological type of AA, sites of involvement, and any associated cutaneous and systemic disorder was collected and analyzed statistically.
The clinical patterns of the disease were classified as Focal, Multifocal, Ophiasis, Sisaipho, Alopecia Subtotalis, Alopecia Totalis, Alopecia Universalis, and Diffuse AA.
RESULTS
A total of 1,010 patients with alopecia areata (AA) attended our outpatient department (OPD) over a four-year period. Of these, 602 (59.6%) were males and 408 (40.4%) were females. The mean age of patients was 24.38 ± 14.1 years, and the mean disease duration was 11.54 ± 23.06 months.
The scalp was the most commonly affected site. However, scalp-only involvement was seen in 488 patients (48.3%), while 522 patients (51.7%) had terminal hair involvement beyond the scalp. The beard was the second most commonly affected site and was the sole site involved in 173 patients (17.1%). When analysis was restricted to male population (including male children), the incidence of beard involvement rose to 28.7% (173/602).
Among the 602 male patients, 394 were older than 18 years, and 248 of them (63%) had beard involvement, either isolated or in combination with scalp involvement.
Eyebrows and eyelashes alone were involved in 27 patients (2.7%), while eyebrows or eyelashes with scalp involvement were seen in 71 patients (7%). Body hair involvement alone was observed in 11 patients, comprising 1.1% of the study population (Table 1).
| Site involved | No. of patients | Percentage |
|---|---|---|
| Scalp only | 488 | 48.3% |
| Beard only | 173 | 17.1% |
| Scalp and beard | 143 | 14.2% |
| Scalp and upper face (eyebrows, eyelashes) | 71 | 7.0% |
| Scalp, beard, and body hair | 48 | 4.7% |
| Upper face only | 27 | 2.7% |
| Scalp, upper face, and body hair | 27 | 2.7% |
| Scalp and body hair | 22 | 2.2% |
| Body hair only | 11 | 1.1% |
| Total | 1010 | 100% |
The most common morphological type of AA was multifocal (612 patients, 60.6%), followed by the focal type (210 patients, 20.8%). Ophiasis was seen in 33 cases and diffuse AA in 31 patients (Table 2).
| Type | No. of Patients | Percentage |
|---|---|---|
| Multifocal | 612 | 60.6% |
| Focal | 210 | 20.7% |
| Alopecia Subuniversalis | 71 | 7% |
| Ophiasis | 33 | 3.2% |
| Diffuse Alopecia Areata | 31 | 3.1% |
| Alopecia Universalis | 21 | 2.1% |
| Alopecia Subtotalis | 20 | 2% |
| Alopecia Totalis | 12 | 1.2% |
| Total | 1010 | 100% |
In 7% (71/1010) of the study population, there was extensive terminal hair loss on different body sites with either a limited or significant degree of scalp involvement. These patients typically presented with limited scalp disease or alopecia subtotalis-like pattern combined with widespread facial and body hair involvement. This population group could not be classified under any of the established morphological types of AA (see Figure 2).
Associated medical and dermatological conditions included vitiligo (36 patients), urticaria (28), generalized pruritus (14), and telogen effluvium (5). Thyroid disorders were found in 62 patients (6.1%), and 9 patients (8.9%) reported a history of hypertension. Atopy was present in 134 patients (13.2%), and its presence was positively correlated with AA severity.
DISCUSSION
Alopecia areata (AA) ranks second only to androgenetic alopecia as the most common cause of hair loss. It is the leading cause of inflammatory alopecia and remains a therapeutic challenge due to its recurrent and unpredictable course. Although AA can begin at any age, an earlier age of onset is associated with a higher risk of recurrence and a more chronic disease trajectory. Poor prognostic factors include early onset, extensive involvement, atopic diathesis, and the ophiasis pattern.1,2
While the scalp is typically the most frequently affected site, other hair-bearing areas such as the beard, eyebrows, and eyelashes are often involved and can have a profound psychological impact. In many cases, hair loss in these areas is as distressing, if not more so, than scalp involvement—particularly because scalp patches may be more easily concealed, whereas beard or eyebrow involvement is more visible. These factors should be considered when tailoring treatment strategies in clinical practice and when designing research protocols.
Despite this, most clinical studies on AA focus primarily on scalp hair and often overlook the impact of involvement in other cosmetically sensitive areas. Very few epidemiological studies have assessed the distribution of AA across different body sites.
In this retrospective analysis of patient records over a four-year period, several noteworthy observations emerged. While scalp involvement may be predominant across the general population—including children—our data shows that among adult males, beard involvement is nearly as common as scalp involvement, with 63% of adult male patients showing beard hair loss. Additionally, more than half of the overall study population had involvement of non-scalp terminal hair. Previous epidemiological studies have similarly reported that more than 50% of AA cases involve sites beyond the scalp.12-13
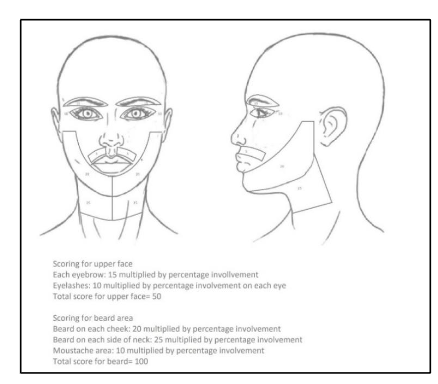
These findings emphasize the need for a comprehensive and objective scoring system that accounts for beard, eyebrow, and eyelash involvement, in addition to scalp hair loss. We have previously proposed the Alopecia Areata Scoring Index (AASI), which quantifies disease severity in these areas.14 The AASI score is calculated as the sum of individual regional scores (Figure 3).
Another important finding from this analysis was the presence of a subset of patients who exhibited AA on multiple body sites, with either limited or significant scalp involvement. These cases do not fit neatly into existing morphological categories such as Alopecia Universalis (due to preserved scalp hair) or Alopecia Subtotalis (due to extensive body hair involvement). In many such cases, the patients present with AA of scalp or beard hair and they are not even aware of the body hair involvement.
We propose the term “Alopecia Subuniversalis” to describe this pattern, characterized by partial but widespread non-scalp involvement, mirroring the concept of subtotalis for the scalp. In our clinical practice we have observed that a significant proportion of patients labelled as Alopecia subtotalis are actually Alopecia subuniversalis cases.
Our study suggests that Alopecia Subuniversalis is more prevalent than certain established patterns like Alopecia subtotalis, Alopecia totalis, Ophiasis or Sisaipho, accounting for approximately 7% of the AA population. This fact alone calls for a relook at the current classification system for AA, which seems to be incomplete as it excludes a significant percentage of patients suffering from this disease.
So, we propose that Alopecia subuniversalis type of AA should be included as a specific morphological type of AA to the current morphological classification to make it more encompassing and complete.
CONCLUSIONS
In AA, beard hair is affected almost as commonly as scalp hair in the male population. In addition, other body areas are also affected in a good percentage of patients in different combinations. This necessitates the use of a composite scoring system to evaluate the severity of alopecia areata (AA) affecting the beard, eyebrows, and eyelashes. Additionally, a significant percentage of patients of AA have extensive disease beyond the scalp with variable scalp hair involvement- we propose a new morphological subtype—alopecia subuniversalis—to describe the disease pattern in these patients.
LIMITATIONS:
This study is limited by its retrospective design and lack of a population-based sampling method. Larger, prospective, and community-based epidemiological studies are required to validate and expand upon these findings.
Conflict of Interest Statement:
None.
Funding Statement:
None.
Acknowledgements:
None.
REFERENCES:
- Mirzoyev SA, Schrum AG, Davis MD, Torgerson RR. Lifetime incidence risk of Alopecia Areata estimated at 2.1 percent by Rochester Epidemiology Project, 1990–2009. The Journal of investigative dermatology. 2014 Apr;134(4):1141.
- Fricke AC, Miteva M. Epidemiology and burden of alopecia areata: a systematic review. Clinical, Cosmetic and Investigational Dermatology. 2015;8:397.
- Harries M, Macbeth AE, Holmes S et al. The epidemiology of alopecia areata: a population-based cohort study in UK primary care. Br J Dermatol 2022; 186:257–65.
- Olsen EA, Roberts J, Sperling L, Tosti A, Shapiro J, McMichael A, Bergfeld W, Callender V, Mirmirani P, Washenik K, Whiting D. Objective outcome measures: collecting meaningful data on alopecia areata. Journal of the American Academy of Dermatology. 2018 Sep 1;79(3):470-8.
- Jang YH, Moon SY, Lee WJ, Lee SJ, Lee WK, Park BC, Kim H. Alopecia areata progression index, a scoring system for evaluating overall hair loss activity in alopecia areata patients with pigmented hair: a development and reliability assessment. Dermatology. 2016;232(2):143-9.
- Olsen EA, Roberts J, Sperling L, Tosti A, Shapiro J, McMichael A, Bergfeld W, Callender V, Mirmirani P, Washenik K, Whiting D. Objective outcome measures: collecting meaningful data on alopecia areata. Journal of the American Academy of Dermatology. 2018 Sep 1;79(3):470-8.
- Waśkiel‐Burnat A, Rakowska A, Sikora M, Olszewska M, Rudnicka L. Alopecia areata predictive score: A new trichoscopy‐based tool to predict treatment outcome in patients with patchy alopecia areata. Journal of Cosmetic Dermatology. 2020 Mar;19(3):746-51.
- Manjaly P, Li SJ, Tkachenko E et al. Development and validation of the Brigham Eyelash Tool for Alopecia (BELA): a measure of eyelash alopecia areata. J Am Acad Dermatol 2021; 85:271–2.
- Stefanis A, Arenberger P, Arenbergerova M et al. Alopecia Barbae Severity Score: a novel scoring system to estimate the extent of beard loss and success of treatment. Br J Dermatol 2021; 185:847–9.
- Liu LY, King BA, Craiglow BG. Health-related quality of life (HRQoL) among patients with alopecia areata (AA): a systematic review. J Am Acad Dermatol. 2016; 75: 806-812.e3.
- Rees H, Wall D, Bokhari L et al. Reliability and validity of a measure to assess the health-related quality of life of women with alopecia areata. Cli Exp Dermatol 2023; 48:681–4.
- Al-Ajlan A, Alqahtani ME, Alsuwaidan S, Alsalhi A. Prevalence of Alopecia Areata in Saudi Arabia: Cross-Sectional Descriptive Study. Cureus. 2020 Sep;12(9).
- Alshahrani AA, Al-Tuwaijri R, Abuoliat ZA, Alyabsi M, AlJasser MI, Alkhodair R. Prevalence and Clinical Characteristics of Alopecia Areata at a Tertiary Care Center in Saudi Arabia. Dermatology Research and Practice. 2020 Mar 13;2020.
- Majid I, Sameem F, Sultan J, Aleem S. Alopecia areata severity index (AASI): A reliable scoring system to assess the severity of alopecia areata on face and scalp—a pilot study. Journal of Cosmetic Dermatology. 2021 Aug;20(8):2565-70.

