Hyperbaric Oxygen Therapy for Long COVID: Evidence Review
Hyperbaric Oxygen Treatment of Long Covid: Review of the Evidence and Perspective
D. Craig Lindsey, MD1; Sandra Wainwright, MD FUHM1
- Hyperbaric Wellness, LLC Founder and CEO; Assistant Clinical Professor, University of New Mexico Hospital, Albuquerque, NM
- Assistant Clinical Professor, Yale School of Medicine, New Haven, CT
OPEN ACCESS
PUBLISHED: 31 August 2025
CITATION Lindsey, DC., and Wainwright, S., 2025. Hyperbaric Oxygen Treatment of Long Covid: Review of the Evidence and Perspective. Medical Research Archives, [online] 13(8). https://doi.org/10.18103/mra.v13i8.6795
COPYRIGHT © 2025 European Society of Medicine. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
DOI https://doi.org/10.18103/mra.v13i8.6795
ISSN 2375-1924
ABSTRACT
Hyperbaric oxygen therapy (HBOT) has emerged as an effective treatment for Long COVID, a condition affecting tens of millions of people in the US and characterized by persistent and debilitating symptoms following SARS-CoV-2 infection. This analysis explores the mechanisms and clinical evidence supporting the efficacy of HBOT in addressing the complex pathophysiology underlying Long COVID. The authors also discuss the social and economic consequences of this new disease, the barriers to accessing HBO treatment and they propose solutions to these barriers.
Keywords
Hyperbaric oxygen therapy, Long COVID, SARS-CoV-2, treatment efficacy, clinical evidence
Mechanisms of Action:
- Anti-inflammatory effects: HBOT reduces pro-inflammatory cytokines (IL-1, IL-6, TNF-α) and elevates anti-inflammatory IL-10
- Endothelial protection: Improves endothelial function, enhances nitric oxide bioavailability, and attenuates oxidative stress
- Neuroplasticity: Stimulates stem cell mobilization, mitochondrial biogenesis, and synaptic plasticity
- Angiogenesis: Stimulates development of new small blood vessels in areas of lost microcirculation, relieves tissue and organ hypoxia, and restores function
- Immune Modulation: HBO inhibits abnormal activation of T and B Lymphocytes
Clinical Evidence:
- Randomized controlled trials using computerized cognitive battery testing and standardized SF-36 physical function metrics have demonstrated significant improvements in fatigue, cognitive function, attention, and quality of life.
- Case studies report reduced inflammation, oxidative stress, enhanced lung function and significant improvement in neurocognitive function in Long COVID patients treated with HBO.
- Durable benefits observed up to one-year post-treatment, with greatest improvements in most disturbed domains.
- Controlled studies demonstrate the safety of HBO treatments.
The growing list of published scientific studies show that HBOT is effective and safe in treating Long COVID. The effectiveness of HBOT is correlated with its ability to target the likely underlying pathophysiology of Long COVID. Currently, HBOT is the only known single treatment that can improve or reverse the many symptoms across multiple organ systems that define Long COVID. These results have been verified and repeated from multiple clinical trials and case reports across the world. The improvement of these symptoms is also sustained long term.
Long COVID affects at least 25-50 million people in the US and up to 1 billion worldwide. The individual effects are varied and can be mild to severely debilitating. When the disease symptoms are profound, it removes people from the workforce, strains personal relationships, and may require around the clock care. It is estimated that the economic impact may be 100 billion in the US annually and up to two trillion globally.
To date, there is not a widely accepted and effective treatment for all the symptoms of Long COVID. This paper presents a review of current scientific studies that highlight hyperbaric oxygen as an effective treatment, a treatment that can reverse the symptoms of Long COVID in a six to eight-week period and has benefits sustained long term. The authors discuss reasons that this treatment currently sees only limited use and they discuss the current limited availability and cost associated with this treatment. They suggest an alternative form of HBOT implementation that would improve both access and affordability. If these last barriers can be overcome, HBO treatment could become the standard by which people recover from Long COVID.
Introduction
Long Covid has emerged as a new significant worldwide medical problem. Long Covid is a condition that follows acute SARS-CoV-2 infection in approximately 10-20% of those acutely infected. It is a constellation of symptoms that has as many as 200 separate defined symptoms and affects as many as 35 million people in the US and upwards of one billion people worldwide. In approximately 20% of those affected, it causes a level of disability that eliminates people from the workforce, creates long term disability, severely negatively affects quality of life, and has a significant monetary cost to communities and societies. It is a challenging problem in several respects including the ability to make an accurate diagnosis and the availability of an effective treatment.
This paper reviews the global scientific literature using Hyperbaric Oxygen as an effective treatment of Long Covid. Hyperbaric Oxygen therapy has known physiologic effects on the processes that are thought to cause Long Covid and is able to effectively reverse many of the symptoms across multiple organ systems. The results are uniformly positive, the treatment is safe, and the results are long lasting. Affordable access and availability of HBO treatments remains challenging, and the authors discuss possible solutions to this issue.
Defining Long COVID
Long COVID is a challenging clinical entity for a variety of reasons: the number of people affected, the significance of disability, the number of symptoms, the variability in presentation, the difficulty in diagnosis, and the lack of a broadly available effective treatment. Up until recently, the definition and nomenclature could also be included in this list.
Long COVID, as a new disease, has been plagued by inconsistent terminology developed by governmental agencies, medical societies, journals, and health organizations in the US and internationally. This has caused confusion among clinicians, has limited research dissemination, and has impeded patients from obtaining recognition, care and support.
The National Academy of Sciences, Engineering and Medicine (NASEM) a private, nongovernmental institution, recently published a 187-page document describing a unifying nomenclature and definition of Long COVID. The Academy chose the name Long COVID and defined it with all the elements of the disease and consequences. The National Academy’s definition as published in 2024 is as follows:
“Long COVID is an infection-associated chronic condition that occurs after SARS-CoV-2 infection and is present for at least 3 months as a continuous, relapsing and remitting, or progressive disease state that affects one or more organ systems.”
Long COVID can present in a multitude of ways with hundreds of possible individual symptoms and or diagnosable conditions affecting any organ system. Common symptoms include shortness of breath, cough, persistent fatigue, post-exertional malaise, difficulty concentrating, memory changes, recurring headache, lightheadedness, tachycardia, sleep disturbances, problems with taste or smell, bloating, constipation and diarrhea.
Common conditions that can be newly diagnosed or if present before SARS-CoV-2 infection, can be made worse, include: interstitial lung disease, hypoxemia, cardiovascular disease and arrhythmias, cognitive impairment, mood disorders, anxiety, migraine, stroke, blood clots, chronic kidney disease, postural orthostatic tachycardia syndrome (POTS) and other dysautonomia, chronic fatigue syndrome, myalgic encephalomyelitis, mast cell activation syndrome, fibromyalgia, connective tissue diseases, hyperlipidemia, diabetes, and autoimmune disorders such as lupus, rheumatoid arthritis and Sjogren’s syndrome.
FEATURES OF LONG COVID
- Long COVID can follow asymptomatic, mild or severe initial SARS-Cov-2 infection
- Long COVID can be continuous from the initial acute infection, or it can be delayed weeks or months
- Long COVID can affect adults and children and does not discriminate among socioeconomic status, age, gender, sexual orientation, race or ethnicity, geographic location, or previous health or disability
- Long COVID can exacerbate previous health conditions or present as new symptoms or diagnoses
- Long COVID can range from mild to severe and can resolve over months or persist for years
- Long COVID is diagnosed based on clinical presentation
- Long COVID can impair an individual’s ability to work, attend school, care for a family member or care for themselves. It can have a profound emotional and physical impact on patients, families, and caregivers.
Scope of the Problem
Long COVID is thought to affect 10-35% of all those that have contracted and recovered from acute SARS-CoV-2 infection. By the end of 2022, the SARS-CoV-2 infection had affected 77% of the US population. If 15% of these go on to develop Long COVID then the number of people that potentially have Long COVID is 35 million people in the US and approaches 1 billion worldwide. The incidence of Long COVID is declining and recent analysis suggests that approximately 3.5% of vaccinated people will go on to develop Long COVID (and 7% of non-vaccinated). This is thought to be related to the effectiveness of immunizations and through the emergence of virus variants. However, there are still about a million new cases of acute SARS-CoV-2 infection daily in the US. At this rate, the number of Long COVID would increase by 12.4 M new cases per year among those vaccinated and at higher rates among those that are not.
There is a growing body of evidence that has met delays or barriers to publication that regardless of vaccine manufacturer have developed POTS or small fiber neuropathy after receiving a COVID vaccine. Although the symptoms that may be induced by the COVID vaccine can overlap with the symptoms that define Long COVID, one is not the same as the other and there is evidence that the COVID vaccine is not the cause of Long COVID. In fact, unvaccinated people are diagnosed with Long COVID nearly twice as often as those that have been vaccinated. However, some PVS participants showed elevated levels of circulating SARS-CoV-2 spike protein up to 709 days post-vaccination, and evidence of EBV-re-activation. Indicating that the vaccines are actually protective against Long COVID rather than the cause. Further research and publications are in process that will help define post vaccination syndrome (PVS).
There is an inherent degree of uncertainty in accurately identifying the number of people in the US and worldwide with Long COVID. Regardless of this, the number is significant. To put this into perspective, the likely number of Long COVID cases in the US (35 million) exceeds the number of adults diagnosed with diabetes (29.4 million).
The symptoms of Long COVID may improve somewhat over time but for many, the symptoms are persistent and result in significant disability that can last for years. Long COVID has significant long term medical consequences for individuals that are affected. Given the fact that this problem also affects millions if not billions of people worldwide, it has a significant economic and social impact on communities, societies and nations.
Economic Impact on Society
A significant number of cases of Long COVID and its associated disabilities affect the working class and result in loss of workforce and associated productivity. The direct and indirect costs of the Long COVID condition have been recently estimated to range from $140 to $600 billion in the US annually and 2-3 trillion globally. To put this into perspective of other medical diagnosis that HBO providers treat, the annual economic impact of the diabetic foot ulcer (DFU) is 9-13 billion in the US.
To date, there is not a widely accepted effective treatment for all, or even most, of the symptoms associated with Long COVID. Long COVID can affect every organ system in the human body and results in hundreds of symptoms and new disease presentations. This makes not only diagnosis difficult, but the search for an effective overall treatment seems beyond reach. However, if one considers a unifying underlying pathophysiology, a systemic process that can affect any organ system, and the organism globally, then the search for an effective treatment can be more focused. Indeed, most of the current research efforts are aligned with this concept.
Pathophysiology of Long COVID and Known Physiologic Effects of HBO Therapy
The pathophysiology of Long COVID is not yet fully understood but current areas of research include chronic inflammation, dysregulated immune response, vascular injury with macro and micro vascular thrombosis resulting in end organ hypoxia and loss of function, mitochondrial dysfunction, and sequestered virus with an associated ongoing immune response.
Each of this pathophysiology has the potential to affect every organ system in our bodies and as a result, could explain the 200+ symptoms and disease categories that are the manifestation of Long COVID. This spectrum of illness is something we are witnessing for the first time in medicine. HBO can address the probable underlying pathophysiology of Long COVID by altering and correcting the mechanisms of this disease.
Long COVID and associated chronic inflammation
- HBO decreases chronic inflammation by decreasing the inflammatory cytokines Tumor Necrosis Factor-alpha (TNF-a), Interleukin 1 and 6 (IL-1, IL-6), and increasing the concentration of anti-inflammatory cytokine Interleukin 10 (IL-10).
- Long COVID and poor organ function related to hypoxia from micro and macro thrombosis. HBO improves tissue and end organ perfusion by stimulating angiogenesis through stem cell mobilization. Resulting in enhanced nutrient blood flow and function in hypoxic organs and tissue beds.
- Long COVID and associated fatigue, exertional intolerance and mitochondrial dysfunction. HBO improves mitochondrial function and increases ATP production.
- Long COVID associated Immune Dysregulation. HBO affects dysregulation of the immune system by inducing stem cell release from the bone marrow and reversing the dysregulated T cell activation. Similar effects are seen with B cell.
- Long COVID associated endothelial cell dysfunction. HBO decreases endothelial cell dysfunction and subsequent macro and micro thrombosis while promoting angiogenesis to those areas with vascular impairment such as the small vessels of end organs like the brain, lung and heart.
The known effects of HBO therapy make it an intriguing treatment arm of Long COVID as it can address the likely mechanisms causing the many symptoms associated with this debilitating illness.
Current Treatment of Long COVID
To date, there have been a variety of potential treatments of Long COVID, including physical therapy, systemic and topical anti-inflammatory therapy, dietary and behavioral therapy, cognitive therapy, rehabilitation, immune therapy and anticoagulation therapy. Unfortunately, none of these have proven universally effective and do not adequately address all of the underlying pathophysiology’s of Long COVID or the constellation of symptoms associated with this entity.
There have been some selective interventions for individual symptoms (IE beta blockers for POTS and corticosteroids for PMR like symptoms) but none have adequately addressed the entirety of the disease or resulted in improvement of the multiple organ system dysfunction seen in Long COVID. The one exception of this, is treatment with hyperbaric oxygen (HBOT). HBO therapy is emerging as one of the only effective treatments. Katz and Wainwright have published a literature review from November 2021 to January 2024 of all published scientific articles related to HBO treatment of Long COVID.
This review included prospective randomized clinical trials, prospective treatment series, case series, case reports, and safety studies. The review included 10 published articles, 8 treatment trials and 2 safety studies and included 284 total patients. The results of all the treatment trials uniformly demonstrated that HBO treatment of Long Covid provided significant improvement in many of the symptoms of Long COVID and was safe.
| Author/Year | # of Subjects | Trial Design | Biomarkers collected | Outcome Measures | Treatment Profile | Results Hyperbaric Effects on Long COVID |
|---|---|---|---|---|---|---|
| Kjellberg A et al Jan 2023 | 20 (goal of 80) | Randomized double blind placebo | n/a | RAND-36 6MWT | 2.4 ATA 90 minutes, two 5-minute air breaks x 40 sessions | No serious adverse events. Favorable safety profile for long COVID patients all of whom had lower quality of life score is than normal population. |
| Robbins T et al Nov 2021 | 10 | Case Series | n/a | Chalder Fatigue scale NeuroTrax evaluation | 2.4 ATA 105 minutes, three 5-minute air breaks x10 sessions over 12 days | Improvement (statistically significant) in fatigue score and cognitive measures using validated scales. |
| Leitman M et al Jun 2023 | 79 | Randomized controlled trial | n/a | Echocardiogram | 2.0 ATA 90 minutes, three 5-minute air breaks x 40 sessions | 48% of long COVID patients demonstrated pre-HBOT systolic dysfunction which was significantly improved. |
| Lindemann J et al Sep 2023 | 59 | Prospective trial | n/a | SF-36 VAS (visual analog scale) | 2.2 ATA 75 minutes x10 sessions (no air breaks mentioned) | In as little as 10 HBOTs – statistical improvement in 80% of metrics, safe and feasible tool for LCS. |
| Zant A, Figueroa S, Paulson C, Wright J 2022 | Six | Clinical Case Report | n/a | Modified Borg dyspnea scale ImPACT symptoms questionnaire | 2.0 ATA 90 minutes x 15-29 sessions (no air breaks mentioned) | All patient’s saw improvement in symptoms. |
| Kitala et al Dec 2022 | 31 | Prospective trial | n/a | Upper and Lower body range of motion Pulsoximetry Spirometry EQ-5D-5L psychotecnical test | 2.5 ATA 75 minutes x15 sessions (no mention of air breaks) | HBOT resulted in significant and lasting improvement in QOL, endurance, strength, spirometry, memory and attention. |
| Zilberman-Itskovich S et al 2022 | 73 | Prospective Randomized Sham Controlled Trial | n/a | SF-36 PSQI BSI-18 Voxel based neuroimaging | 2.0 ATA 90 minutes, three 5-minute air breaks x 40 sessions | HBOT improve cerebral blood flow and brain micro structural changes in those areas that are associated with executive function, cognitive and psychiatric symptoms. |
| Mrakic-Sposta S et al Sep 2023 | Five | Case Series | Urine and Saliva | ROS, TAC, (IL-6, IL1β and TNF-α) Fatigue Severity Scale Spirometry | 2.4 ATA 90 minutes (no mention of air break) | N=2, 15 Statistically significant effect of HBOT on biomarkers in all subjects. HBOT is a potential treatment for long COVID patients. |
| Bhaiyat A et al Feb 2022 | One | Case Report | n/a | Perfusion MRI Exercise Testing Spirometry | 2.0 ATA 90 minutes, three 5-minute air breaks x60 sessions | Improved cognition and cardiopulmonary function. |
| Kjellberg A et al Apr 2025 | 80 (40 HBOT 39 control) | RCT, double blind phase II | n/a | RAND-36 RP | 2.4 ATA 90 minutes two 5-minute air breaks x 10 sessions | In both control and experimental groups improvement was demonstrated with no significant difference between each group. |
One of the publications reviewed was a randomized, sham-controlled, double-blind trial evaluating the effects of hyperbaric oxygen therapy (HBOT) on patients suffering from Long COVID by Zilberman-Itskovich et al. The study involved 73 patients who had ongoing symptoms for at least three months after confirmed SARS-CoV-2 infection. Participants were randomized into two groups: one receiving HBOT (35 patients) and the other receiving a sham treatment (37 patients) while in a hard sided hyperbaric chamber. The treatment profile was 40 sessions divided 5 days per week. Each HBO session was at 2.0 ATA of 100% oxygen delivered by face mask for 90 minutes. Five-minute air brakes were provided every 20 minutes. The trial aimed to assess improvements in neurocognitive functions and various physical symptoms. Patients had neurocognitive function tested at baseline, at study completion and at a year after study completion. The patients also had functional MRI’s done to evaluate CNS blood flow at each of these time points.
Key findings include:
- Statistically significant improvements in global cognitive function, attention, and executive function in the HBOT group compared to the control group.
- Statistically significant improvements in energy levels, sleep quality, depression, somatization and pain interference.
- Brain MRI showed increased perfusion and microstructural changes in specific brain regions associated with the cognitive and emotional functions that had improved.
The study suggests that HBOT can induce neuroplasticity and improve many symptoms across multiple organ systems in Long COVID patients. Mechanisms were thought potentially due to increased brain perfusion and neuroplasticity. Follow up analysis of these patients at 1 year post treatment indicated that the results and physiologic changes were sustained.
In a paper by Efrati et al, neurocognitive battery testing essentially found that the Long COVID brain functions similarly to a brain with ADHD. In order to complete a task, for example, from A to B, the long COVID brain will require multiple steps across several regions. That same brain after HBOT exposure will process information more efficiently with reduced processing pathways. This was statistically significant. Essentially people with long COVID complain of profound fatigue and will have to sleep after any taxing social or cognitive exposures. The ‘Long COVID brain’ is paralleled by a severely sleep deprived brain. It exhibits impaired cognitive function, attention, memory and decision-making capacities. This type of neurologic fatigue can cause lapses in attention and performance which presents similarly to ‘micro-sleeps’ a behavior seen in humans who are subjected to extreme exhaustion. Consider military and first responders. Soldiers or truck drivers ‘nod off’ despite the high-risk environment.
The only study that found no difference between the control group and the HBO treated group was the recent publication by Kjellberg et al. This study treated patients with 10 sessions of HBO over a 6 week period. The lack of significant improvement over the control group is likely related to the relatively low number of HBO sessions and the fact that they were spread over a six week period.
The review by Katz and Wainwright highlights the beneficial effects of HBO treatment across populations of patients. This is critical in terms of understanding the potential utility of HBO for effectively treating this problem. It does not, however, highlight the struggles that individuals can suffer when afflicted with this disease.
A Case Study Highlighting Hyperbaric Oxygen Effect
M Martinez, a 49-year-old male professional with Long COVID was referred to our HBO center following an 18-month history of persistent symptoms following acute SARS-CoV-2 infection. The symptoms were many but the most pronounced and debilitating was severe neurocognitive dysfunction. This impairment prevented the patient from working full time in the local court system and caused him to stop driving as he could no longer remember which way to turn at a 4-way traffic stop to get to his destination. This was in a small town in which he had lived his entire life. He had tried many other forms of therapy including a variety of supplements and allographic IV stem cell therapy without success. The patient was distraught and thought that he may have to live in an assisted living/memory care home for the rest of his life. He had contemplated suicide as an alternative to living with this condition. He was treated with HBO receiving once daily sessions (M-F) at 2.2 ATA for 90 minutes with no air brakes for a total of 40 sessions. He also did independent third-party neurocognitive testing before and after his treatments. (CNS Vital Signs)
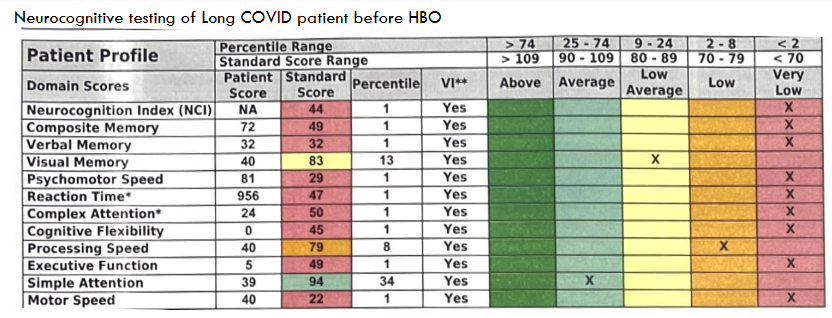
Neurocognitive testing of Long COVID patient before HBO:
Neurocognitive testing of Long COVID patient at 31 HBO sessions:
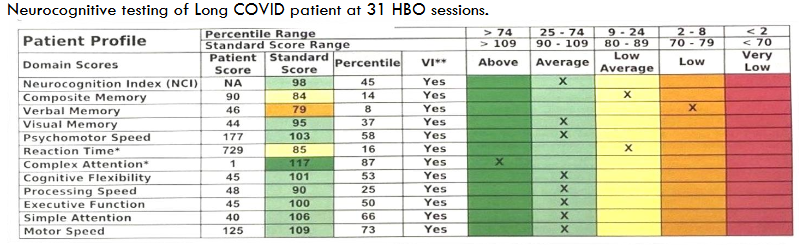
The patient had a profound neurocognitive deficit at his pretreatment baseline. The patient scored in the 1 percentile of a normal population in 9/12 tested categories. After treatment, the patient improved his scores resulting in 8/12 test scores in the normal range and one in the above normal range. Only 3/12 categories remained in the low-to-low average categories. Many of his other associated symptoms of Long COVID including fatigue, muscle and joint pain, sleep quality, depression and anxiety were also improved. The patient was able to return to work full time and resumed driving and other ADLs of independent living. In essence, his life returned to normal. Note that the final neurocognitive testing was done at 31 completed sessions, the patient went on to complete a total of 40 sessions but did not return to do another neurocognitive test.
Rarely has this provider seen such a dramatic reversal of symptoms with a single form of treatment in such a short period of time.
Discussion
The published studies of treating Long COVID with HBO have uniformly shown benefit. Whether HBO treatment of Long COVID is effective or not is now hard to debate. It has repeatedly been shown to be effective in reversing or improving many symptoms across multiple organ systems. It is safe and the results are long lasting. Considering this, it is surprising that HBOT treatment of Long COVID has not been recognized or widely adopted by the general medical community. What then, are the possible reasons that HBOT is not yet the standard treatment for Long COVID?
Why is HBOT not the standard of care for Long COVID?
There are several factors that are likely responsible for the lack of acceptance of HBO as a standard treatment for Long COVID. We will outline each of these areas below:
- Lack of large, randomized trials
- Lack of large-scale dissemination of existing trial results
- Lack of general medical education and awareness of HBO mechanisms and efficacy
- Lack of effective number of chambers to address Long COVID
- High cost of current HBO delivery models
We will also discuss a competing unregulated and unproven HBO labeled treatment promoted by medical spas and wellness centers where patients are attracted by relatively low cost and easy access. We address each of these issues below:
Lack of large scale randomized clinical trials:
Hyperbaric oxygen as a drug has been a treatment modality since the 1960’s with many randomized controlled trials demonstrating its efficacy in various diseases. However, many of these trials are small in comparison to the larger pharmaceutical trials often approved by the FDA and where corporate sponsorship is responsible for approximately 75% of funding to the FDA for clinical research.
The niche field of HBO medicine that uses oxygen under pressure as a therapeutic intervention does not attract industry interest or government funding in terms of sponsoring large clinical trials. This accounts for the relatively few and small clinical trials with limited dissemination and awareness of HBO’s clinical effectiveness in treating Long COVID as well as other emerging indications.
Lack of broad dissemination and awareness of HBO treatment mechanisms and efficacy:
There are competing efforts along the path of treating Long Covid patients. Most Long COVID clinics are studying the spectrum of symptoms in a multidisciplinary approach that usually includes a team of cardiologists, pulmonologists, neurologists and infectious diseases physicians. Therapies often consist of behavioral training, oral supplements along the lines of nutraceuticals, dietary modification, some trials with pharmaceutical agents and immune modulating therapies. However, none of these approaches comprehensively address the underlying pathology of Long COVID, nor reverse the vascular injury or hypoperfusion to end organs like hyperbaric oxygen therapy does.
Hyperbaric oxygen therapy (HBOT) remains a striking example of a disconnect between the medical community and the public. While the medical establishment often views HBOT with skepticism or limited awareness—relegating its proven efficacy to a narrow list of conditions like decompression sickness, chronic wounds, and carbon monoxide poisoning—laypeople are increasingly turning to Google in droves, desperately seeking it as a therapeutic lifeline.
Physicians, bound by evidence-based practice and cautious about off-label uses, may lack training or exposure to HBOT’s broader potential, with many medical schools glossing over it and research funding lagging behind more conventional treatments. Meanwhile, driven by anecdotal success stories, wellness trends, and conditions like Long COVID or traumatic brain injury, patients scour the internet, discovering spas and clinics offering HBOT, often outpacing the medical community’s willingness to embrace or study it further. This juxtaposition highlights a growing chasm: a cautious, underexplored modality in medicine versus a grassroots clamor for access fueled by hope and online discovery.
Hyperbaric medicine is a niche area of medicine and is not routinely part of general medical education, training or residency programs. As a result, most providers entering medical practice have little or no experience or background in hyperbaric medicine. It is perhaps of little surprise then, that many don’t understand its physiologic effects or its relevance to the likely pathophysiology of Long COVID.
In contrast, HBO medical providers have been trained and are experienced with the physiology and safety of this treatment. They also likely understand that many of the known mechanisms of HBO treatments would make it a good candidate to counter the effects of Long COVID. Many of these trained HBO providers follow the guidelines established by their medical society, the Undersea and Hyperbaric Medical Society or UHMS. This organization accredits HBO facilities, trains and educates HBO providers and approves medical diagnosis for treatment, CMS and private insurance, in large part, support the medical diagnosis approved by the UHMS. At this point in time, Long COVID is not approved for HBO treatment by the UHMS and is not supported for payment by CMS or private insurance. As a result, most hospital-based HBO treatment centers are not accepting Long COVID patients for treatment.
The UHMS seeks to promote high standards of education, research and practice. Its conservative approach to accepting new indications is founded in a methodological review of the existing body of evidence. While the current literature favors HBOT for treatment of Long COVID – this is a relatively new disease. As with many scientific bodies, adopting new therapies requires time and consideration. Fortunately, hyperbaric medicine has been established as safe and effective in many other conditions – it is a matter of adopting this as a new indication as the body of evidence continues to grow.
The UHMS and the HBO community does not have a history of being presented with the sheer number of patients affected by one disease that responds as well to HBO as Long COVID. A new disease that affects 10’s of millions of people in the US, one that is associated with a significant individual disability, one that, as a collective, has an enormous economic impact, and one where HBOT appears to be the only effective treatment. The usual multi-year waiting period before approval, as it has been the case for other supported diseases, would be disastrous for those individuals affected by Long COVID and to the economies of the communities and nations where they reside.
To put this into perspective, most accepted diagnoses for HBO treatments affect relatively few people. For example, one of the more common diagnoses for treatment is the diabetic foot ulcer. Estimates of the total number of cases at any given time are around 1.6 million annually in the US. Of these, only a small fraction (1.2% of Medicare and 2.3% of private insured age 65 and older) received HBO treatment. This equates to about 19 K to 37 K patients per year. In contrast, the Long COVID population in the US is 35 million and virtually all of them could benefit from HBO treatment.
The relative lack of awareness and acceptance of HBO treatment of Long COVID by regulatory and insurance agencies is, unfortunately, only one of several barriers preventing routine access of Long COVID patients to HBO treatments.
Lack of effective number of chambers to address Long COVID
Another major barrier is the relative lack of availability of chambers that are operated in a safe and regulated environment. There are approximately 1000 hospital associated hyperbaric centers in the US, each with 2-6 chambers. If one assumes an average of 4 chambers per facility (note that the number of centers and chambers are estimates and are chosen for the ease of calculation and to facilitate discussion) and that each chamber could treat 4 patients per 8-hour workday. This results in 16 patients treated per facility per day. If each patient receives 30 M-F treatments, one facility of 4 chambers could treat 139 patients in a year at full capacity. Most facilities fill only 50-60% of their daily treatment capacity with insurance reimbursable diagnosis and do not treat other diagnoses. This leaves about 70 patient treatment slots open for treatment of any other diagnosis such as Long COVID per facility per year, or about 70,000 patients per year across all facilities in the US. This is the entire existing HBO treatment capacity that could be available to treat Long COVID. With an estimated 35 million patients diagnosed with Long COVID in the US, it would take 500 years to treat the current number of cases. If one limits the number of treated Long COVID cases to only the most severely affected and out of the workforce (25% of Long COVID patients had significant physical limitations after a year and 18% had remained out of the workforce) this would conservatively be 18% and would total 6.3 million. It would still take 90 years to treat just the most significantly impaired of the Long COVID patients. Again, this would mean all the centers in the US dedicating all their open treatment slots to just Long COVID and this does not consider the 12 million new cases per year that are expected to occur. Clearly, there is a need for more HBO treatment access at existing facilities and or for more treatment facilities to be available, perhaps even outside of the standard hospital-based model.
The next barrier for Long COVID patients to receive HBO treatment is cost.
Many more HBO centers need to exist, but they also need to be able to provide treatment at an affordable cost. Most HBO treated patients have Medicare and or a private insurance payor. The billed amount to these payors in total is roughly 5K per treatment or 150K per patient. This is roughly $600 per session or $18K per patient from Medicare and the rest from private insurance. The reimbursed payments are, by contract, somewhat less than this.
If Long COVID were to be treated at a hospital facility, the patient would have to pay out of pocket at a rate determined by the hospital. At a minimum, this would have to be a rate that covers the cost of HBO delivery in this environment and be affordable to the patient as an out-of-pocket expense. This would have to be at a much lower rate than what hospitals currently receive from CMS and insurance providers. The reality is that hospital-based HBO centers would not likely displace insurance reimbursable diagnosis with one that is paid out of pocket at a much lower rate. It is unlikely that hospitals would make any more treatment slots available to out of pocket payment categories.
There is also a concern that if Hospitals treat so-called off label diagnoses like Long COVID that they will somehow put their ability to bill CMS for any or all other diagnoses at risk. I have personally had my hospital and its parent company’s (Operating 600 Centers in the US, Mexico and South America) legal department investigate this and they have found no case law that would indicate that this is a concern. Unfortunately, this is still a commonly held concern and deterrent for most hospital-based HBO providers and their administrations.
It is in the long-term economic interest of CMS and private insurance to support the current cost of Hyperbaric treatments for Long COVID patients in a hospital-based facility. It is estimated that the short- and long-term disability costs, (loss of wages, medical care etc) of the Long COVID patients will approach 600 billion dollars annually. However, to pay for HBO treatments at the current rates of combined Medicare and private insurance at 100-150K per patient for 70,000 patients per year = 7-10.5 billion per year. And if supported by Medicare only, the cost would be 18K X 70,000= 1.26 billion per year. This is significantly less than the estimated 140-600 billion per year of not treating this population.
This is still a very expensive treatment when provided in a hospital setting and is likely a deterrent to acceptance of CMS and private insurance support in the short term, even if it makes sense in the long term. And, as outlined above, even if CMS and private insurance supported this treatment, there are not nearly enough HBO treatment slots available to adequately address the Long COVID problem.
A POSSIBLE SOLUTION:
An alternative way to provide HBO for the millions of people with Long COVID is to build nonhospital based centers. To do this with the same standards and safety of those in the hospital setting and provide HBO treatment at a fraction of the hospital costs. The few non-hospital-based centers that exist in the US and treat non yet FDA approved diagnosis charge anywhere between 100 to 1000 per session or 3K to 30K for a series of 30 treatments. Far less than the 100-150K at hospital-based centers. Let’s assume a cost per treatment session at $600 per session and $18K per patient (30 sessions). This may be a fee that allows nonhospital based facilities to be financially sustainable and at the same time, be affordable to at least a segment of the Long COVID population, especially if CMS and private insurance were to offset this cost.
Patients afflicted by Long COVID are aware of the costs at hospital centers, the lack of insurance coverage, and the lack of access. They are being attracted to something often called mild HBO treatment. “Mild” HBOT (mHBOT) systems—lower-pressure chambers (e.g., 1.3–1.5 ATA)—which are more affordable and commonly adopted by wellness spas compared to medical-grade chambers (2.0–3.0 ATA). These mild systems don’t require the same regulatory oversight or medical staffing, making them ideal for spas. This is not a true HBO treatment but is being advertised as such. The UHMS defines HBO treatment as whole-body exposure to 100% oxygen at pressures greater than 1.4 ATA. The mild HBO treatment occurs typically in a soft sided chamber and internal pressures are typically less than 1.4 ATA and oxygen concentrations often less than 100%. These centers do not comply with national safety standards and although the treated patients may say they feel better after treatments, there have not been published objective results that indicate improvement like there has been for true medical grade HBO treatments in hard sided chambers, that are FDA approved and meet ASME and PVHO-2 standards in facilities that are NFPA 99 compliant, at pressures equal to or greater than 2 ATA.
Mild HBO treatments should not be considered real HBO treatments or even mild HBO treatments. They don’t qualify by UHMS standards to be labeled HBO treatments at all and should not be used for indications like Long COVID. However, given the lack of access and cost of hospital-based HBO treatments, one can see why patients are attracted to mislabeled yet much more available and affordable forms of HBO labeled treatments.
As of February 20, 2025, likely a few hundred to a couple thousand wellness spas nationally offer HBOT, with the number having grown an estimated 30–50% since 2020, driven by post-pandemic wellness demand and the affordability of mild chambers – which are not capable and have not been studied to provide therapeutic exposure to either pressure or oxygen. Many of these facilities are using unsafe and/or unimproved pressure vessels and ‘providers’ who are not licensed to practice medicine or deliver oxygen as a drug depending on state law.
How do we balance the faster pace of public interest in potential therapies with the slower pace of collecting enough evidence to support the adoption of a new hyperbaric indication? Perhaps the bridge between the two worlds is a pathway by which office based hyperbaric centers support the body of evidence by treating these patients under the understanding that the condition is “under investigation” via access to an IRB or by contributing to a hyperbaric registry. However, safety is tantamount and should be optimized through collaboration with a scientific organization that has subject matter experts in diverse hyperbaric technical and medical knowledge like the UHMS.
Long COVID is the most significant medical problem in terms of number of patients, and economic impact, that has faced the HBO community in its history. How this medical specialty responds to this issue will likely determine their future. They can lead a new and safe way of making HBO available to 10’s of millions of patients in need and, as an industry and medical specialty, be revitalized and provided with a bright and long future. Their choices will also determine the future of HBO medicine as a regulated and safe entity. This could be the unforeseen medical crisis that opens a new and prosperous era to HBO medicine.
It is the opinion of this HBO provider that HBO treatments should be made available to Long COVID patients at a reasonable cost and in a safe and controlled environment. This could be in the traditional hospital-based facilities, but because of the sheer enormity of the problem, hospital-based centers cannot effectively treat this entity in a meaningful time frame. To ethically provide this needed intervention, more treatment centers are needed and this likely means supporting and allowing this to be performed outside of the traditional hospital setting but regulated to keep treatments safe and of a standard that is proven to provide results.
As shown, emerging research suggests hyperbaric oxygen therapy may offer benefits for conditions like Long COVID. However, caution is essential when applying oxygen as a drug. This constitutes medical treatment that requires oversight by licensed medical professionals using FDA-approved Class II medical devices that comply with ASME PVHO-2 and NFPA safety standards. Healthcare providers and consumers are encouraged to pursue evidence based practices, ensuring proper medical supervision and informed consent.
Conclusion
HBO treatment of Long COVID is effective and safe. It remains the only effective treatment for this diagnosis that can reverse or improve most symptoms across all organ systems and the benefits are long lasting. The mechanisms by which this occurs remain unconfirmed but are thought to be related to the ability of HBO treatment to modulate inflammation, release stem cells from the bone marrow, affect the immune system and mitochondria and regenerate the microcirculation. Regardless of mechanism conformation, the results are real and reproducible. Unfortunately, access to this treatment remains unavailable to the vast majority of those that are afflicted. The number and severity of this illness has a significant impact on the workforce and the cost to the healthcare system. Possible solutions are presented and discussed.
About the authors:
Dr Lindsey, MD is a board-certified emergency physician and has been the medical director of a nationally accredited HBO treatment center for the last 15 years. He has recently retired from this position and is focusing full time on Long COVID treatment and issues surrounding access, as well as wound care education. He directs and runs Hyperbaric Wellness, LLC, an online resource to help Long COVID patients with diagnosis, testing and connection to affordable and safe HBO treatments.
Dr. Wainwright, MD is board certified in Pulmonary and Critical Care medicine. She is the medical director of the Hyperbaric Medicine and Wound Healing Center at Yale New Haven Health – Greenwich campus. She has been practicing hyperbaric medicine for nearly two decades. She is active in the UHMS organization, is currently the UHMS president elect and is developing an interest in hyperbaric medicine ethics and safety.
References
- National Academies of Sciences, Engineering, and Medicine. A Long COVID Definition: A Chronic, Systemic Disease State with Profound Consequences. Washington, DC: The National Academies Press; 2024. doi:10.17226/27768
- Huerne K, Filion KB, Grad R, Ernst P, Gershon AS, Eisenberg MJ. Epidemiological and clinical perspectives of long COVID syndrome. Am J Med Open. 2023;9:100033. doi:10.1016/j.ajmo.2023.100033
- Tin A. How many Americans still haven’t caught COVID-19? CDC publishes final 2022 estimates. CBS News. Published July 3, 2023. Accessed June 24, 2025. https://www.cbsnews.com/news/how-many-americans-havent-caught-covid-cdc-estimates/
- Elflein J. Long COVID in the U.S. – statistics & facts. Statista. Published October 29, 2024. Accessed June 24, 2025.
- Office of the Assistant Secretary for Health (OASH). Long COVID. U.S. Department of Health & Human Services. Published February 2024. Accessed June 24, 2025. https://us.pagefreezer.com/nl/wa/browse/0a7f82bb-be6e-448a-ae11-373d22c37842?url=https:%2F%2Fwww.hhs.gov%2Fsites%2Fdefault%2Ffiles%2Flong-covid-update-2024.pdf×tamp=2025-05-01T07:02:19Z
- Backman I. COVID vaccines reduce long COVID risk, new study shows. Yale Medicine. Published September 2, 2024. Accessed June 24, 2025. https://www.yalemedicine.org/news/covid-vaccines-reduce-long-covid-risk-new-study-shows
- Bornali Bhattacharjee, Peiwen Lu, Valter Silva Monteiro et al; Immunological and Antigenic Signatures Associated with Chronic Illnesses after COVID-19 Vaccination medRxiv2025.02.18.25322379; doi: https://doi.org/10.1101/2025.02.18.25322379
- Centers for Disease Control and Prevention (CDC). National Diabetes Statistics Report. CDC Diabetes. Published May 15, 2024. Accessed June 24, 2025. https://www.cdc.gov/diabetes/php/data-research/index.html
- Centers for Disease Control and Prevention (CDC). Living with Long COVID. Published February 3, 2025. Accessed July 11, 2025. https://www.cdc.gov/covid/long-ter-effects/living-with-long-covid.html
- Hadanny A, Zilberman-Itskovich S, Catalogna M, et al. Long term outcomes of hyperbaric oxygen therapy in post covid condition: longitudinal follow-up of a randomized controlled trial. Sci Rep. 2024;14(1):3604. Published February 15, 2024. doi:10.1038/s41598-024-53091-3
- Al-Aly Z, Davis H, McCorkell L, et al. Long COVID science, research and policy. Nat Med. 2024;30:2148–2164. doi:10.1038/s41591-024-03173-6
- Voruz P, Assal F, Péron JA. The economic burden of the post-COVID-19 condition: underestimated long-term consequences of neuropsychological deficits. J Glob Health. 2023;13:03019. Published May 5, 2023. doi:10.7189/jogh.13.03019
- Katz AA, Wainwright S, Kelly MP, Albert P, Byrne R. Hyperbaric oxygen effectively addresses the pathophysiology of long COVID: clinical review. Front Med. Published February 14, 2024. Accessed June 24, 2025.
- Schottlender N, Gottfried I, Ashery U. Hyperbaric oxygen treatment: effects on mitochondrial function and oxidative stress. Biomolecules. 2021;11(12):1827. Published December 3, 2021. doi:10.3390/biom11121827
- Chen L, Wang Y, Zhou H, Liang Y, Zhu F, Zhou G. The new insights of hyperbaric oxygen therapy: focus on inflammatory bowel disease. Precis Clin Med. 2024;7(1):pbae001. Published 2024 Jan 18. doi:10.1093/pcmedi/pbae001
- Li Y, Zhang H, Liang Y, et al. Effects of hyperbaric oxygen on vascular endothelial function in patients with slow coronary flow. Cardiol J. 2018;25(1):106-112. doi:10.5603/CJ.a2017.0132
- Miike T, Sakamoto Y, Sakamoto Y, et al. Influence of hyperbaric oxygen therapy on thrombus formation ability in humans. Undersea Hyperb Med. 2020;47(4):591-595. doi:10.22462/10.12.2020.8
- Davis HE, McCorkell L, Vogel JM, et al. Long COVID: major findings, mechanisms and recommendations. Nat Rev Microbiol. 2023;21:133–146. doi:10.1038/s41579-022-00846-2
- Katz AA, Wainwright S, Kelly MP, Albert P, Byrne R. Hyperbaric oxygen effectively addresses the pathophysiology of long COVID: clinical review. Front Med. Published February 14, 2024. Accessed June 24, 2025. Thom SR. Hyperbaric oxygen: its mechanisms and efficacy. Plast Reconstr Surg. 2011;127 Suppl 1(Suppl 1):131S-141S. doi:10.1097/PRS.0b013e3181fbe2bf
- Kjellberg A, Abdel-Halim L, Hassler A, et al. Hyperbaric oxygen for treatment of long COVID-19 syndrome (HOT-LoCO): protocol for a randomised, placebo-controlled, double-blind, phase II clinical trial. BMJ Open. 2022;12(11):e061870. Published November 2, 2022. doi:10.1136/bmjopen-2022-061870
- Robbins T, Gonevski M, Clark C, et al. Hyperbaric oxygen therapy for the treatment of long COVID: early evaluation of a highly promising intervention. Clin Med (Lond). 2021;21(6):e629-e632. doi:10.7861/clinmed.2021-0462
- Leitman M, Fuchs S, Tyomkin V, Hadanny A, Zilberman-Itskovich S, Efrati S. The effect of hyperbaric oxygen therapy on myocardial function in post-COVID-19 syndrome patients: a randomized controlled trial. Sci Rep. 2023;13(1):9473. Published June 10, 2023. doi:10.1038/s41598-023-36570-x
- Wu BQ, Liu DY, Shen TC, Lai YR, Yu TL, Hsu HL, Lee HM, Liao WC, Hsia TC. Effects of Hyperbaric Oxygen Therapy on Long COVID: A Systematic Review. Life (Basel). 2024 Mar 26;14(4):438. doi: 10.3390/life14040438. PMID: 38672710; PMCID: PMC11051078.
- Zant AE, Figueroa XA, Paulson CP, Wright JK. Hyperbaric oxygen therapy to treat lingering COVID-19 symptoms. Undersea Hyperb Med. 2022 Third Quarter;49(3):333-339. doi: 10.22462/05.06.2022.7. PMID: 36001566.
- Kitala D, Łabuś W, Kozielski J, Strzelec P, Nowak M, Knefel G, Dyjas P, Materniak K, Kosmala J, Pająk J, Czop J, Janda-Kalus B, Marona B, Nowak-Wróżyna A, Gierek M, Szczegielniak J, Kucharzewski M. Preliminary Research on the Effect of Hyperbaric Oxygen Therapy in Patients with Post-COVID-19 Syndrome. J Clin Med. 2022 Dec 30;12(1):308. doi: 10.3390/jcm12010308. PMID: 36615108; PMCID: PMC9821575.
- Garred P, Madsen MB, Hyldegaard O, Hedetoft M. Hyperbaric oxygen treatment is associated with a decrease in cytokine levels in patients with necrotizing soft-tissue infection. Physiol Rep. Published March 14, 2021. Accessed June 24, 2025. https://physoc.onlinelibrary.wiley.com/doi/full/10.14814/phy2.14757
- Zilberman-Itskovich S, Catalogna M, Sasson E, et al. Hyperbaric oxygen therapy improves neurocognitive functions and symptoms of post-COVID condition: randomized controlled trial. Sci Rep. 2022;12:11252. Published July 12, 2022. doi:10.1038/s41598-022-15565-0
- Mrakic-Sposta S, Vezzoli A, Garetto G, Paganini M, Camporesi E, Giacon TA, Dellanoce C, Agrimi J, Bosco G. Hyperbaric Oxygen Therapy Counters Oxidative Stress/Inflammation-Driven Symptoms in Long COVID-19 Patients: Preliminary Outcomes. Metabolites. 2023 Sep 25;13(10):1032. doi: 10.3390/metabo13101032. PMID: 37887357; PMCID: PMC10608857.
- Bhaiyat AM, Sasson E, Wang Z, Khairy S, Ginzarly M, Qureshi U, Fikree M, Efrati S. Hyperbaric oxygen treatment for long coronavirus disease-19: a case report. J Med Case Rep. 2022 Feb 15;16(1):80. doi: 10.1186/s13256-022-03287-w. PMID: 35168680; PMCID: PMC8848789.
- Kjellberg A, Abdel-Halim L, Hassler A, El Gharbi S, Al-Ezerjawi S, Boström E, Sundberg CJ, Pernow J, Medson K, Kowalski JH, Rodriguez-Wallberg KA, Zheng X, Catrina S, Runold M, Ståhlberg M, Bruchfeld J, Nygren-Bonnier M, Lindholm P. Hyperbaric oxygen for treatment of long COVID-19 syndrome (HOT-LoCO): protocol for a randomised, placebo-controlled, double-blind, phase II clinical trial. BMJ Open. 2022 Nov 2;12(11):e061870. doi: 10.1136/bmjopen-2022-061870. PMID: 36323462; PMCID: PMC9638753.
- Hadanny A, Zilberman-Itskovich S, Catalogna M, Elman-Shina K, Lang E, Finci S, Polak N, Shorer R, Parag Y, Efrati S. Long term outcomes of hyperbaric oxygen therapy in post covid condition: longitudinal follow-up of a randomized controlled trial. Sci Rep. 2024 Feb 15;14(1):3604. doi: 10.1038/s41598-024-53091-3. PMID: 38360929; PMCID: PMC10869702.
- Kjellberg A, Abdel-Halim L, Hassler A, El Gharbi S, Al-Ezerjawi S, Boström E, Sundberg CJ, Pernow J, Medson K, Kowalski JH, Rodriguez-Wallberg KA, Zheng X, Catrina S, Runold M, Ståhlberg M, Bruchfeld J, Nygren-Bonnier M, Lindholm P. Ten sessions of hyperbaric oxygen versus sham treatment in patients with long covid (HOT-LoCO): a randomised, placebo-controlled, double-blind, phase II clinical trial. BMJ Open. 2025 April 14; 15(04):e094386. doi: 10.1136/bmjopen-2024-094386. PMID: 40228859; PMCID: PMC11997836.
- www.sleepfoundation.org/sleepdeprivation/lack-of-sleep-and-cognitive-impairment
- https://www.cnsvs.com
- Bodenheimer, T. 2000. Uneasy alliance: Clinical investigators and the pharmaceutical industry. New England Journal of Medicine 342:1539-1544.
- https://www.nytimes.com/2022/09/15/health/fda-drug-industry-fees.html
- J. Bradford Rice, Urvi Desai, Alice Kate G. Cummings, Howard G. Birnbaum, Michelle Skornicki, Nathan B. Parsons; Burden of Diabetic Foot Ulcers for Medicare and Private Insurers. Diabetes Care 1 March 2014; 37 (3): 651–658. https://doi.org/10.2337/dc13-2176
- Ford ND, Slaughter D, Edwards D, et al. Long COVID and Significant Activity Limitation Among Adults, by Age — United States, June 1–13, 2022, to June 7–19, 2023. MMWR Morb Mortal Wkly Rep 2023;72:866–870.
- Gelly HB. Trends in Medicare costs of hyperbaric oxygen therapy, 2013 through 2022. Undersea Hyperb Med. 2024;51(2):137–144. Published June 2024. Accessed June 24, 2025.

