Post-Professional Doctoral Education for PAs: A Review
“`html
Review of Post Professional Doctoral Education for the Physician Assistant/Associate: Recommendations for Entry-level Curriculum
Jenna Rolfs, DMSc, MBA, PA-C, DFAAPA, Debra Munsell, DHSc, PA-C, DFAAPA, James R. Kilgore, DMSc, PhD, PA-C, DFAAPA, Jeremy M. Welsh, PhD, DHSc, JD, PA-C, DFAAPA, Michael S. Roscoe, PhD, PA-C, DFAAPA, Blake Rogers, DMSc, PA-C, Thomas Colletti, DHSc, MPAS, PA-C Emeritus, DFAAPA, Raquelle Akavan, DMSc, PA-C, Travis Kaufman, DMSc, PA-C, FIBODM
Abstract
The Physician Associate (PA) profession has undergone significant educational evolution, culminating in the emergence of PA-specific post-professional doctoral degree (PPDD) programs. Amid growing interest in transitioning to an entry-level doctoral degree (ELDD), this manuscript provides a comprehensive review of current PPDD curricula, analyzes thematic trends across programs, and proposes strategic curricular expansions for entry-level PA education. The analysis includes data from 33 PA PPDD programs, revealing consistent emphasis on scholarly writing, healthcare leadership, advocacy, and administrative competencies. Drawing on bridge program models and stakeholder initiatives including the American Academy of Physician Associates House of Delegates and the Physician Assistant Education Association Doctoral Commission, the manuscript recommends a 9-12 credit hour curricular augmentation, achievable within 1-3 months, to align master’s-level instruction with doctoral-level rigor. Suggested revisions to Accreditation Review Commission-PA standards aim to ensure curricular compliance and feasibility. The proposed model seeks to enhance the leadership, policy-making, and scholarly capacities of future PA graduates while preserving clinical excellence. These findings contribute to an evidence-informed dialogue around ELDD feasibility and offer actionable pathways for advancing PA education.
Keywords
Physician Assistant, Doctoral Education, Curriculum Development, Healthcare Leadership, Entry-Level Doctoral Degree
Introduction
Since the Physician Associate (PA) profession’s inception in 1967, a series of changes in the types of degrees that PA programs confer have occurred. Initially, PA programs awarded their graduates either a certificate or a baccalaureate degree. In 1973, the University of Colorado was the first PA school to grant a master’s degree to its graduates. The number of PA programs offering master’s degrees as the entry-level degree for completion has increased, whereas those awarding certificates or baccalaureate degrees have declined. By the end of 2001, 54% of PA programs awarded master’s degrees, and by 2010, 91% of them did, although this criterion did not become an accreditation standard until 2021, when it became a standard for students matriculating into a PA program after December 31, 2020.
The profession is now witnessing the rise of PA-specific post-professional doctorate degree (PPDD) programs. Many US health professions require or encourage profession-specific doctoral training, with many having introduced transitions from baccalaureate to master’s or master’s to doctoral pathways over the last 40 years. There are now 33 PPDD programs, which include eight bridge programs that allow recent graduates of an entry-level PA educational program to receive credit for clinical training and a truncated process to complete their doctoral training within three to six months. Most of the bridge programs allow for direct entry into the doctoral program upon graduation from an entry-level PA program.
The PA profession is not alone in its exploration of entry-level doctoral education. Other healthcare fields, such as physical therapy (DPT) and advanced nursing practice (DNP), have already transitioned to doctoral-level entry points. Lessons from these professions, both in terms of curriculum restructuring and stakeholder adaptation, may offer valuable guidance as the PA profession evaluates a similar trajectory.
There were 189,907 certified PAs at the end of 2024, and 2.7% of those held doctorate degrees. PAs represent one of the largest groups of licensed clinical practitioners in the United States who do not have doctoral degrees. Additionally, the US Bureau of Labor Statistics projects a 28% employment growth for PAs between 2022 and 2032. This growth is significantly faster than average, resulting in approximately 12,900 job openings each year.
The PPDD pursued by PAs is for those who seek advanced training and additional skills related to healthcare administration, organizational leadership, research, scholarship, clinical, and education roles. There are two primary options for PA-specific postgraduate training. Those are clinical fellowships, some of which award doctoral degrees or a post-professional doctorate. The 2025 American Academy of Physician Associates (AAPA) House of Delegates (HOD) moved forth a recommendation for the investigation of an entry-level doctoral degree (ELDD) for the profession. HP-4262 was adopted, which stated: AAPA recognizes the rigor, breadth, and depth of current PA curricula, and supports working with relevant stakeholders on the development of a pathway to awarding an entry-level PA doctoral degree. The HOD requests that a report on this pathway be delivered no later than the 2027 HOD meeting. This has resulted in continuing work by a variety of entities to investigate the curriculum requirements for an entry-level doctoral degree for the PA profession.
The PAEA has been formally investigating the ELDD for the PA profession since 2019. The process of exploring the ELDD began with a vote by the PAEA Board of Directors to hold a Doctoral Summit in March 2023. Members of the PA community and select related fields participated in the 2-day Summit. Additionally, PAEA-sponsored faculty research teams conducted stakeholder interviews, and discussions took place at several town halls and two Education Forums regarding the ELDD. While confirming the current entry-level degree as a master’s degree, the decision was made to develop a comprehensive doctoral degree strategy for pathways to a doctoral degree as the entry-level degree for the profession. Since its first meeting in the fall of 2024, the Doctoral Commission has made steady progress on its work and presented a report on the PAEA Doctoral Education Commission at the AAPA 2025 Annual Conference.
Given the forthcoming reports from the AAPA HOD and the PAEA Doctoral Commission, this manuscript serves as a timely contribution to the literature by offering a detailed curricular proposal rooted in an empirical review of current post-professional and bridge doctoral programs. It aims to complement and guide future discussions around the feasibility, structure, and alignment of an entry-level doctoral model for the PA profession.
The number of credit hours for an entry-level master’s PA education program ranges from 90 to 144 credit hours, which is determined by the institution’s approved curriculum. With the range of credit hours for a master’s degree being 30 to 60, entry-level master’s PA education programs are nearly double the master’s credit hour requirement. Thus, when determining the PPDD bridge program curriculum for PAs, it is imperative to keep this high credit hour requirement at the forefront. Additionally, Section B of the Accreditation Review Commission – PA (ARC-PA) standards for entry-level PA accreditation outlines what must be taught for curriculum and instruction to graduate PAs ready to enter the workforce to provide excellent patient care. The question being considered is what additional coursework should be required for an entry-level PA program to award the doctoral degree.
Method
The authors conducted an internet search for PA-specific PPDD websites in June 2025. Information was collected from PA-specific PPDD representative organizations (Consortium of DMS/DMSc Programs and the PAEA website). Clinical fellowships that offered doctorates were identified but not included. Using these resources, PA-specific PPDD education websites were reviewed. An exhaustive review of PPDD programs for the PA was conducted, focusing on program-identified core courses as listed on program websites, promotional materials, and university course catalogs, or obtained through personal communication with program representatives. A thematic analysis of the course titles was used to identify general categories of instruction. Descriptive statistics were applied to evaluate the data.
Results
As of June 2025, a total of 33 PA-specific post-doctoral programs were identified. A majority of programs offered several concentrations or tracks. The number of core courses ranged from four to fifteen. These concentrations and/or certificate programs offer participants the option to gain specific instruction in advanced clinical or professional skills. Concentration and certificate instructions included a wide variety of options. Most concentrations or tracks included leadership and advocacy, medical education, and healthcare administration instruction.
PROGRAM DURATION, COST, AND INSTITUTIONAL ALIGNMENT
The number of credit hours required to graduate from PA-specific doctorate programs ranges from 24 to 50, with an average of 39. The start dates for students in the current PPDD programs evaluated by McKenna and Hooker vary, and the number of cohorts each program enrolls annually ranges from one to six. The programs are 9 to 30 months in duration, with an average of 16 months. An enrollment period depends on the number of credits transferred from an entry-level PA program and the number of courses taken each quarter or semester. The inclusion of the bridge programs in the current research has identified program length ranging from one to six months.
The cost per credit hour was $785, ranging from $480 to $1,275. Additional fees for applications, labs, books, or other fee-based resources were noted but not computed due to inconsistencies in their citations. Considering the costs per credit hour and the varying number of credit hours required to complete each program, the average tuition-only cost was $30,109 in 2024.
Most programs offer core courses in evidence-based medicine and training in the skills necessary to produce peer-reviewed and practical scholarship. The most common concentrations reported by McKenna and Hooker were medical education, health administration, management, leadership, global and public health, professional development, and emergency/disaster management. Other curricular focuses included behavioral, health program management, health informatics, and entrepreneurship. Several programs concentrated on enhancing and applying medical knowledge in primary care, emergency medicine, internal medicine, psychology/behavioral health, or a field chosen by the student. It is worth noting that clinically focused PPDD programs differ from clinical fellowships. Students in clinically focused programs already practice in their fields of study and apply didactic lessons learned to their daily patient-care duties, which are logged as part of their practicums.
PREPARING FOR AN ENTRY-LEVEL DOCTORAL MODEL
Although curricula, credit hours, and time commitments may vary, the majority of PA PPDD include a course in evidence-based medical writing. These can lead to a capstone project or a scholarly research paper. This final experience typically involves researching, writing, and submitting a manuscript to a journal, followed by a peer review process. Upon analysis of all post-professional doctoral programs for PAs, this has emerged as a defining feature across nearly all post-professional PA doctoral programs. This is likely because, for current entry-level master’s PA education programs, the curriculum must include instruction in preparing students to evaluate the medical literature but does not require every student to write a scholarly manuscript. This remains a variation amongst entry-level master’s programs, but a constant in post-professional doctorate programs.
Most programs include core courses that address the overall process of healthcare delivery. Organizational theory and leadership management are key components of these programs, with many offering electives that allow students to customize their course of study. It was noted in the findings by McKenna and Hooker that their analysis mirrors those of McQuillan and colleagues, who identified 22 PA doctorate programs in their research offering 30 concentrations. In analyzing their learning outcomes and mission statements, they reported that these programs aligned with four of the seven competencies for the PA profession. One area of interest for college- or university-based PA programs is the potential influence of the institutional accreditation process on the development of future entry-level professional doctorate degrees for PAs. The same six institutional regional accreditation commissions that McKenna and Hooker identified were examined by Snyder and Miller, who found that most PA programs are housed within comprehensive or doctoral degree-granting organizations. This implies that these new programs are unlikely to encounter significant accreditation challenges should they choose to create entry-to-practice DMSc programs.
In a review of the post-professional doctoral program curriculum by Hussein, Sasek, Danielsen, et al., the primary intended outcomes of the PA-specific doctoral programs were to develop PA leaders, PA faculty, and increase clinical acumen. Common concentrations offered included academic/education, leadership, clinical practice, and global health. Clinical practice focuses within the programs include various specialties, such as addiction medicine, behavioral medicine, critical care, emergency medicine, internal medicine, primary care, and psychiatry.
A more recent review of PA-specific post-professional doctoral program themes found that the majority of the programs focus on leadership and management, research and scholarly activity, evidence-based practice, quality and safety, health systems and policy, capstone and practicum, professionalism and ethics, and public and population health.
The Accreditation Review Commission on Education for the Physician Assistant (ARC-PA) is the current accrediting agency for entry-level PA educational programs in the United States. The curriculum guidelines for an entry-level PA program are contained within the Accreditation Standards for Physician Assistant Education, Fifth Edition, Effective September 1, 2020 (Clarifications 11/2019, 9/2020, 3/2021, 3/2022, 9/2022, 3/2023, 9/2023, 3/2024, 6/2024 & 07/2024; Updates December 2024 and April 2025). The standards in section B1 apply to the entire curriculum of the program and have application to all curricular components. The standards in Section B2 primarily apply to the didactic curriculum of the program but may also be included in the clinical curriculum, as appropriate and as determined by the program. The standards in section B3 apply to the clinical curriculum of the program. The standards in section B4 apply to the entire curriculum of the program and have application to all curricular components. The current ARC-PA Standards are extensive and define a wide range of required didactic and clinical training.
A summary of the requirements for an entry-level PA program as defined in the B2.02a B4.04b Standards is described as follows:
- CORE AREAS OF INSTRUCTION:
- Medical sciences: Anatomy, physiology, pathophysiology, pharmacology, pharmaco-therapeutics, genetics, and molecular biology.
- Clinical medicine: Comprehensive coverage of all organ systems and patient populations across the lifespan.
- Patient care skills: History taking, physical exams, diagnosis, differential diagnosis, ordering/interpreting tests, management of acute/chronic care, patient education, and referral.
- Special populations and considerations: Emphasis on diversity, disability status, gender identity, race/ethnicity, religion, and social determinants of health.
- Clinical reasoning and communication: Development of problem-solving skills and interpersonal communication with patients, families, and other professionals.
- ADDITIONAL INSTRUCTIONAL CONTENT:
- Procedural and technical skills: Aligned with current practice standards.
- Interprofessional collaboration: Team-based care involving a variety of health professionals, beyond traditional physician-PA dynamics.
- Social and behavioral sciences: Topics include human development, stress, illness response, sexuality, substance use, and violence prevention.
- Counseling and patient education: Focused on patient adherence, cultural sensitivity, and behavior change strategies.
- Evidence-based practice: Literature search and evaluation, biostatistics, research methods, and database use.
- Health care systems: Includes billing, coding, documentation, policy, and system navigation.
- Public health: Disease prevention, surveillance, population health, and advocacy.
- Patient safety and quality: Focus on error prevention, risk management, and system improvement.
- PA professional topics: Credentialing and professional standards.
The curriculum must align with the program’s established competencies and provide both the breadth and depth necessary to prepare students for clinical medical practice.
For every didactic and clinical course, including both required and elective rotations, the program must:
- Define and publish learning outcomes and instructional objectives
- Ensure these outcomes are stated in measurable, assessable terms
- Use them to guide students in acquiring the required competencies
SUPERVISED CLINICAL PRACTICE EXPERIENCES (SCPEs) MUST:
- Support all students in achieving learning outcomes related to preventive, emergent, acute, and chronic care
- Span the entire lifespan, including care for infants, children, adolescents, adults, and the elderly
- Include conditions that require surgical management, encompassing pre-operative, intra-operative, and post-operative care
- Address behavioral and mental health conditions
The program must conduct frequent, objective, and documented evaluations of student performance in both the didactic and clinical components. These assessments must:
- Reflect the content and expectations of the instruction
- Identify and address any student deficiencies promptly
Finally, each student must undergo a summative evaluation during the final four months of the program. This evaluation is required to confirm that the student has achieved competence in:
- Clinical and technical skills
- Clinical reasoning and problem-solving
- Interpersonal communication
- Medical knowledge
- Professional behavior
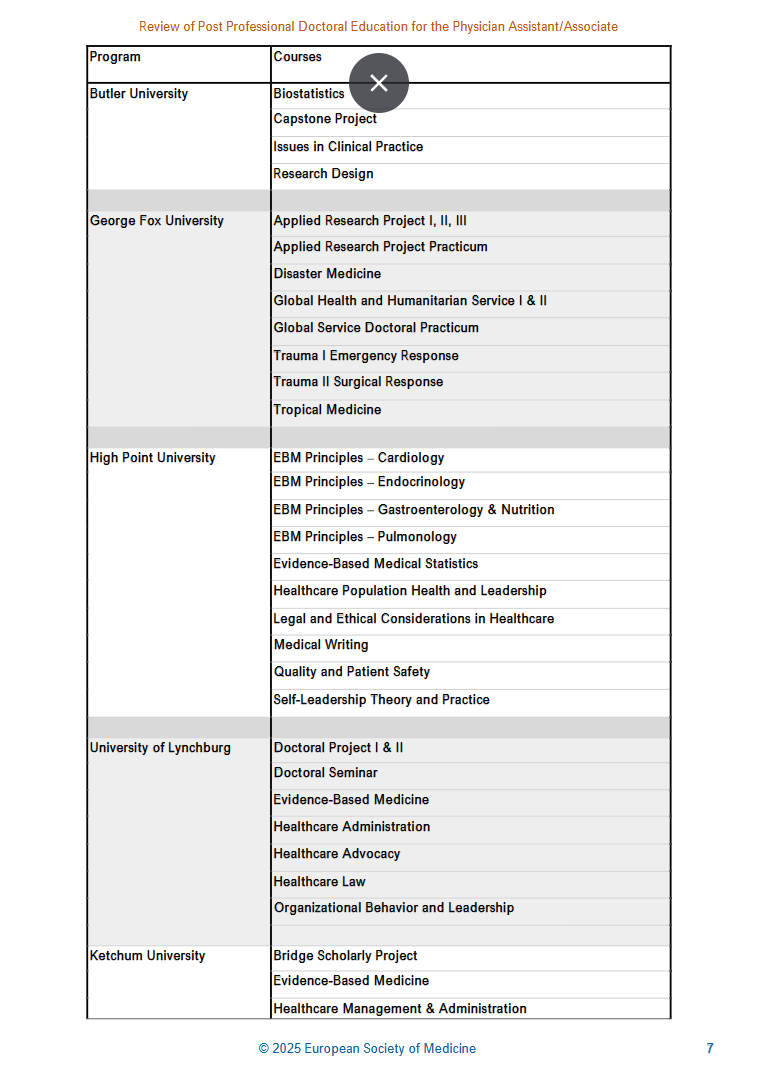
There are currently eight post-professional doctoral PA programs in the US that are considered bridge programs, awarding a degree to students within one to six months post-graduation. Several programs allow credit for didactic and clinical courses from the entry-level PA programs. The credit ranges from 16 to 37 hours. The common courses amongst the current bridge programs are evidence-based medicine or scholarly writing, capstone projects/manuscripts, healthcare leadership/administrative focus, ethics and advocacy, and healthcare law. The bridge programs are Butler University, George Fox University, High Point University, University of Lynchburg, Marshall B. Ketchum, Pacific University Oregon, Shenandoah University, and Wingate.
Discussion
The current didactic and clinical training in the entry-level PA curriculum should be preserved to maintain a strong foundation in medical knowledge and clinical competencies. However, the curriculum should be expanded to include courses in evidence-based writing, aimed at producing scholarly work suitable for publication or presentation. ARC-PA B Standards currently require evidence-based practice: literature search and evaluation, biostatistics, research methods, and database use to be included in didactic instruction. Additionally, integrating coursework in leadership and administrative skills would strengthen students’ preparedness for roles in healthcare management, policy development, and interdisciplinary team coordination. This could potentially be completed in nine to twelve credit hours of additional coursework over one to three months of didactic-focused training. Through curriculum adjustments, programs could integrate core doctoral-level content, such as scholarly writing, healthcare advocacy, and leadership, into existing didactic and clinical components. By embedding these competencies within current structures, many PA programs may only require an additional one to three months of didactic-focused training. This strategic integration supports the feasibility of transitioning to an entry-level doctoral model without extending program length beyond current norms.
The foundational elements of Evidence-Based Medicine (EBM) and Doctoral Project courses may align with content already covered in current Master’s entry-level programs. Each program will need to evaluate its existing curriculum to determine the most effective approach. Each program will need to either integrate new doctoral-level courses or enhance the rigor of current offerings. If an existing master’s program includes a group-based Master’s Research Project, this course could be elevated to doctoral-level rigor by transitioning it to an individual manuscript requirement. This strategic approach to optimizing the current curriculum clarifies and supports the recommendation for an additional 9-12 credit hours of new coursework.
The addition of the recommended curriculum for an entry-level PA doctoral degree would necessitate the development of new standards to be inclusive of this added curriculum. Upon review of the current ARC-PA 5th Edition standards, the following standards would need to be revised, or an additional standard added to meet curriculum needs for the entry-level PA Doctoral Degree.
- Standard B2.13 The curriculum must include instruction to prepare students to search, interpret, and evaluate the medical literature to include:
- a) Framing of research questions,
- b) Interpretation of basic biostatistical methods,
- c) The limits of medical research,
- d) Types of sampling methods, and
- e) The use of common databases to access medical literature.
One suggested rewrite to meet the Evidence-Based Medicine and individualize Doctoral Project for the entry-level PA Doctoral Degree could be:
- Standard B2.13 The curriculum must include instruction and practical application to prepare students to search, interpret, evaluate the medical literature, and compose scholarly writing to include:
- a) Framing of research questions,
- b) Interpretation of basic biostatistical methods,
- c) The limits of medical research,
- d) Types of sampling methods, and
- e) The use of common databases to access medical literature.
- f) Composing a scholarly manuscript to include structuring, writing, and refining a research paper suitable for publication.
To incorporate Healthcare Advocacy into the entry-level PA doctoral degree, upon review of the current standards, an additional standard would need to be added. One suggested addition could be:
- Standard B2.X Healthcare Advocacy: The curriculum must include advanced instruction and opportunities to prepare students to develop a strong professional identity, critically analyze, strategize, and engage in advocacy efforts aimed at improving healthcare systems, policy, and professional standards to include:
- a) Explore and utilize resources for health professions advocacy,
- b) Design and apply advocacy models for governmental engagement,
- c) Propose and implement leadership models for coalition advocacy,
- d) Construct strategic approaches to healthcare system reform,
- e) Advocate for improved regulation and training of health professionals.
To incorporate Organizational Behavior and Leadership instruction into the entry-level PA Doctoral Degree, upon review of the current standards, an additional standard would need to be added. One suggested addition could be:
- Standard B2.Z Organizational Behavior and Leadership: The curriculum must include instruction and experiential learning opportunities to develop students’ capabilities as influential leaders within complex healthcare organizations, to include:
- a) Analyze healthcare organizational structures and culture,
- b) Apply fundamental leadership theories and styles,
- c) Develop skills in team leadership and interprofessional collaboration,
- d) Appraise change management within healthcare organizations,
- e) Explore the PA’s role in influencing organizational effectiveness.
To incorporate Healthcare Law into the entry-level PA Doctoral Degree, upon review of the current standards, an additional standard would need to be added. One suggested addition could be:
- Standard B2.BB Healthcare Law and Regulatory Compliance: The curriculum must include comprehensive instruction designed to equip students with a foundational understanding of healthcare law and regulatory frameworks to include:
- a) Identify Key Healthcare Laws and Regulations,
- b) Examine Professional Licensure and Scope of Practice,
- c) Analyze Medical Malpractice and Liability,
- d) Recognize Ethical and Legal Implications in Clinical Practice,
- e) Apply Legal Principles to Documentation and Risk Management,
- g) Discuss the Impact of Health Policy on Practice.
Limitations
Omitted from this analysis are PA clinical postgraduate fellowship programs, which vary in length and are growing in number. A few of these programs award a doctorate upon completion, whereas others confer degrees in collaboration with the post-professional programs included in our analysis. The most significant limitation of this work is the lack of information from each program regarding alumni outcomes, the employment demand for advanced degrees, or their societal value based on their curriculum.
Conclusion
The Physician Associate (PA) profession has steadily advanced in educational rigor, culminating in the development of PA-specific post-professional doctoral programs. Although only a small percentage of certified PAs currently hold doctoral degrees, the increasing institutional interest signals a shift toward exploring entry-level doctoral pathways. This review reveals that key competencies, including scholarship, healthcare leadership, advocacy, and administrative acumen, are deeply embedded in existing post-professional curricula but remain underrepresented in traditional master’s-level entry programs.
Integrating targeted doctoral-level coursework into entry-level PA education is both feasible and strategically valuable. A compact 9-12 credit hour expansion, focused on evidence-based medical writing, leadership, healthcare law, ethics, and policy, could be added without significantly extending program duration. This enhancement would equip graduates not only for clinical excellence but also for influential roles in academia, administration, and health system reform, amplifying the profession’s reach and impact across diverse healthcare settings.
Although institutional accreditation requirements and curricular demands present hurdles, the presence of bridge models and existing infrastructure provides a viable foundation for implementation. The proposed transition emphasizes outcome evaluation, stakeholder engagement, and financial sustainability to safeguard access and workforce readiness. In the broader context of healthcare education reform, this manuscript calls for the PA profession to define its future educational trajectory, ensuring graduates are prepared for interdisciplinary collaboration and leadership within a rapidly evolving healthcare landscape.
References
- University of Colorado Anschutz Medical Campus. Physician Assistant Program, School of Medicine. History and Future. University of Colorado PA Program website. Accessed February 12, 2025. https://medschool.cuanschutz.edu/physician-assistant-program/program/history-and-future.
- By the Numbers: Program Report 34: Data from the 2018 Program Survey. Physician Assistant Education Association; 2019:48. https://paeaonline.org/wp-content/uploads/imported-files/program-report-34-20191002.pdf
- Kulo V, Fleming S, Gordes KL, Jun H-J, Cawley JF, Kayingo G. A physician assistant entry-level doctoral degree: more harm than good? BMC Med Educ. 2021;21(1):274. doi:10.1186/s12909-021-02725-5
- Martin AER, Kayingo G. Doctoral education for physician assistants/associates: trends and characteristics in the U.S. BMC Med Educ. 2025; 25(1):2. doi:10.1186/s12909-024-06606-5
- Pang J, Armstrong D. Health Professions Education Program Outcomes, 2013-2022. University at Albany, School of Public Health; 2024. www.healthworkforceta.org
- Consortium of DMS/DMSc Post-Professional Doctoral Programs. (unpublished internal data)
- National Commission on Certification of Physician Assistants (NCCPA). 2024 Statistical Profile of Board Certified PAs. Published May 2025. Accessed July 8, 2025. https://www.nccpa.net/wp-content/uploads/2025/05/2024-Statistical-Profile-of-Board-Certified-PAs.pdf
- Ewing H, Davis R, Danielsen RD, Sauers E, Reesal R. The history and development of Doctor of Health Science (DHSc) programs in the United States. Part III Future needs, foundational factors, and principles. Internet J Allied Health Sci Pract. 2024;22(4):3. https://nsuworks.nova.edu/ijahsp/vol22/iss4/3/
- U.S. Bureau of Labor Statistics. Physician assistants. Occupational Outlook Handbook. April 2025. Accessed June 27, 2025. https://www.bls.gov/ooh/healthcare/physician-assistants.htm
- Ewing H, Davis R, Danielsen RD, Sauers E, Reesal R. The history and development of Doctor of Health Science (DHSc) programs in the United States. Part I Past. Internet J Allied Health Sci Pract. 2024;22(4):1. https://nsuworks.nova.edu/ijahsp/vol22/iss4/1/
- McKenna RE, Hooker RS. The PA postprofessional doctorate. JAAPA. 2025;38(5):35-41. doi:10.1097/01.JAA.0000000000000201
- PAEA Board of Directors. PAEA doctoral degree discussions. Accessed June 26, 2025. https://paeaonline.org/resources/public-resources/paea-news/paea-board-of-directors-releases-position-policy-on-the-entry-level-degree
- Accreditation Review Commission on Education for the Physician Assistant (ARC-PA). Accreditation Standards for Physician Assistant Education. 5th ed. 2020. Accessed June 22, 2025. https://www.arc-pa.org/wp-content/uploads/2025/05/Standards-5th-Ed-July-2024.pdf
- McQuillan MA, Asprey D, Brown D, Quincy B, Snyder JA, Sivahop J. Do physician assistant professional doctorate missions and learning outcomes align with the physician assistant professional competencies? J Physician Assist Educ. 2025;36(1). doi:10.1097/JPA.0000000000000642
- Snyder JA, Miller A. What if The impact of institutional accreditation on PA programs transitioning to an entry-level professional doctorate degree. J Physician Assist Educ. Published online December 24, 2024. https://journals.lww.com/jpae/abstract/2025/06000/what_if_the_impact_of_institutional_accreditatio
- Hussein AN, Sasek CA, Danielsen RD, et al. Exploring the landscape of physician assistant/associate specific doctoral education in the United States: a national program survey. J Physician Assist Educ. Published online May 9, 2025.
“`

