PRGF-Endoret in Surgical Treatment of Oral Metastases
Is it Possible to Use a Platelet Rich Plasma (PRGF-ENDORET®) in Case of Oral Metastatic Lesions?
Maurizio Stefano Giacomello ¹, Alberto Giacomello ², Enrico Rescigno ³, Alberta Greco Lucchina 4, Carmen Mortellaro 4
¹ School of Dentistry (Director: Prof. M. Baldoni), School of Medicine and Surgery, University of Milano-Bicocca, 20126 Milan, Italy. [email protected]
² Private practice
³ President-elect of ANTHEC (Academy of Neoregeenrative Therapies and Hemocomponents)
4 Research Laboratory in Regenerative Medicine and Tissue Engineering Saint Camillus International University of Health Sciences, Rome, Italy
OPEN ACCESS
PUBLISHED: 31 August 2025
CITATION Giacomello, MS., Giacomello, A., et al., 2025. Is it Possible to Use a Platelet Rich Plasma (PRGF-ENDORET®) in Case of Oral Metastatic Lesions? Medical Research Archives, [online] 13(8). https://doi.org/10.18103/mra.v13i8.6789
COPYRIGHT © 2025 European Society of Medicine. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
DOI: https://doi.org/10.18103/mra.v13i8.6789
ISSN 2375-1924
ABSTRACT
Aim of the present study is to describe the surgical treatment of a metastatic lesion in mandibular region derived from a prostatic cancer in an old patient, and the benefits of the PRGF®-Endoret®, a particular kind of Platelet Rich Plasma (PRP), on healing processes. The old patient was in a very bad conditions with several medical pathologies, as congestive cardiopathy and chronic kidney distress. Moreover, he was treated with zolendronic acid to block the metastatic bone lesions, a drug that increases the risks to have a BRONJ (bisphosphonates related osteonecrosis of the jaws): in fact, the mandibular lesion was associated with bone necrosis and neuropathic pain from the right mandible to the right ear along the path of the lower alveolar nerve. Moreover, bisphosphonates drugs normally disturb the healing processes of the oral mucosae and gums. The use of PRGF®-Endoret® during the surgical treatments of this case helped to solve the mandibular lesion avoiding the risk of a bad healing. Furthermore, this case shows that in selected cases it is possible to use a PRPs as PRGF®-Endoret® after removal metastatic lesions despite these autologous biomaterials can promote the cancer cells growth. Anyway, in these kinds of problems, the selection of the patients, their life expectancy and their clinical conditions are very important to decide if the benefits are more than the risks associated to the use of PRP. However more studies are necessary to confirm the possibility to use the PRP in the surgical treatment of the cancer or metastatic lesions, exactly because these biomaterials can induce a worsening of the cancer prognosis.
Keywords: osteonecrosis, jaw necrosis, BRONJ, PRGF®-Endoret®, PRP, platelet concentrates, healing improvement, metastatic lesion.
COVER LETTER
This article wants to highlight the usefulness of platelet concentrates in promoting tissue healing, even in cases of severe patient frailty, particularly when associated with the use of drugs that may impair the tissue repair processes. In particular, since the use of autologous platelet concentrates and growth factors (secreted by the platelets themselves) may promote tumor growth, this work aims to highlight how an appropriate surgical resection approach can reduce this risk, although not eliminate it entirely, despite the use of these molecules at the treatment site. The decision to employ this autologous biomaterial was based on the need to enhance the natural healing process, which was negatively affected by the ongoing pharmacological therapy and the patient’s clinical condition. For this reason, the publication of this clinical case report may provide useful information for other clinicians who are faced with similar clinical situations.
THE EUROPEAN SOCIETY OF MEDICINE
Medical Research Archives, Volume 13 Issue 8
RESEARCH ARTICLE
Aim of the study
Tissue healing represents a fundamental biological process through which the body restores the structural and functional integrity of damaged tissues. This complex mechanism involves a well-orchestrated sequence of cellular and molecular events, including hemostasis, inflammation, cell proliferation, and tissue remodeling. Each of these phases is regulated by specific biochemical signals produced locally in response to injury and can be influenced by systemic, environmental, or pathological factors. Under ideal conditions, repair results in restitutio ad integrum, meaning the complete restoration of the original morphology and function of the tissue. However, when tissue damage is extensive, or in the presence of alterations in the cellular microenvironment, the process may shift toward healing by second intention, characterized by scar formation and partial or complete loss of original tissue function. A particularly relevant clinical challenge is the impaired healing observed in patients with chronic or systemic diseases. Conditions such as diabetes mellitus, vascular insufficiency, autoimmune disorders, neoplasms, and immunosuppression (whether iatrogenic or due to primary causes) profoundly affect the inflammatory response, vascularization, cellular proliferation, and remodeling of the extracellular matrix. In these patients, healing is often delayed, incomplete, or complicated by infections and recurrences, with significant prognostic and therapeutic implications.
Aim of the present study is to describe the surgical treatment of a metastatic lesion in mandibular region derived from a prostatic cancer in an old patient, and the benefits of the PRGF®-Endoret®, a particular kind of PRP, on healing processes. The peculiarity of this case, and the reason to tell this story, is the very bad conditions of the patient (with several medical pathologies, as congestive cardiopathy and chronic kidney distress) and his treatment with zolendronic acid, drug that increases the risks to have a BRONJ (bisphosphonates related osteonecrosis of the jaws), conditions that stopped any trial of a surgical approach to solve the problems of this patient. In fact, these clinical situations usually induce several disturbs of the healing processes. Our surgical approach, helped by the use of the PRGF®-Endoret®, a pure Platelets Rich Plasma (P-PRP), solved the mandibular lesion. Furthermore, this case shows that in selected cases it is possible to use PRP as PRGF®-Endoret® (and growth factors released by the platelets) after removal of cancer or metastatic tissues without the risk of an excess of cell growth stimulation.
Materials and methods
A male patient (87 years old) suffering from prostatic cancer in serious conditions of health (for severe cardiopathy and chronic kidney distress) had metastatic bone lesions in several part of his body, as the bone scintigraphy exam showed (image 1), with low expectancy of life. Moreover, his quality of life was very poor because he suffered from a pain starting on the right part of the mandible and arising up to the right ear along the path of the lower alveolar nerve. The pain was deep, continuos and burning due to a bone lesion in right part of mandible that surrounded the alveolar nerve.
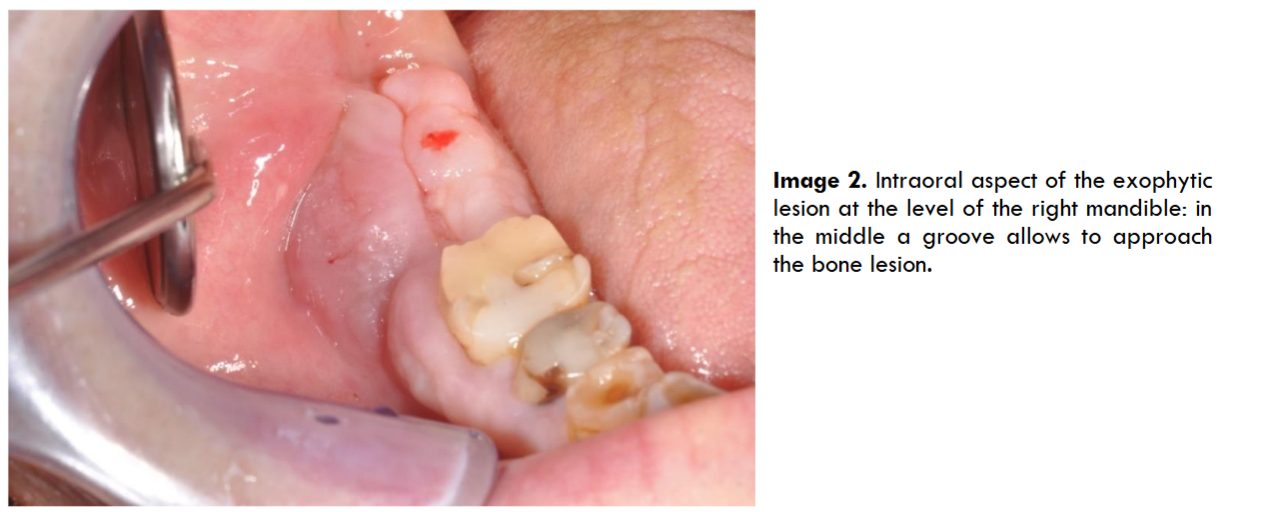
Despite his bad conditions the patient was independent and conscious of his health conditions and he required the resolution of the pain to live the last years without that problem. The oral lesion had a vegetative aspect with exophitic growth of the gingival mucosa associated with bone osteolysis and osteonecrosis of the right mandible. The lesion had an important opening along the edge of the mandible into the exophitic tissue (image 2) that connected the osteolytic lesion with the oral cavity: this gap allowed to a continuous bacterial invasion with frequent infections.
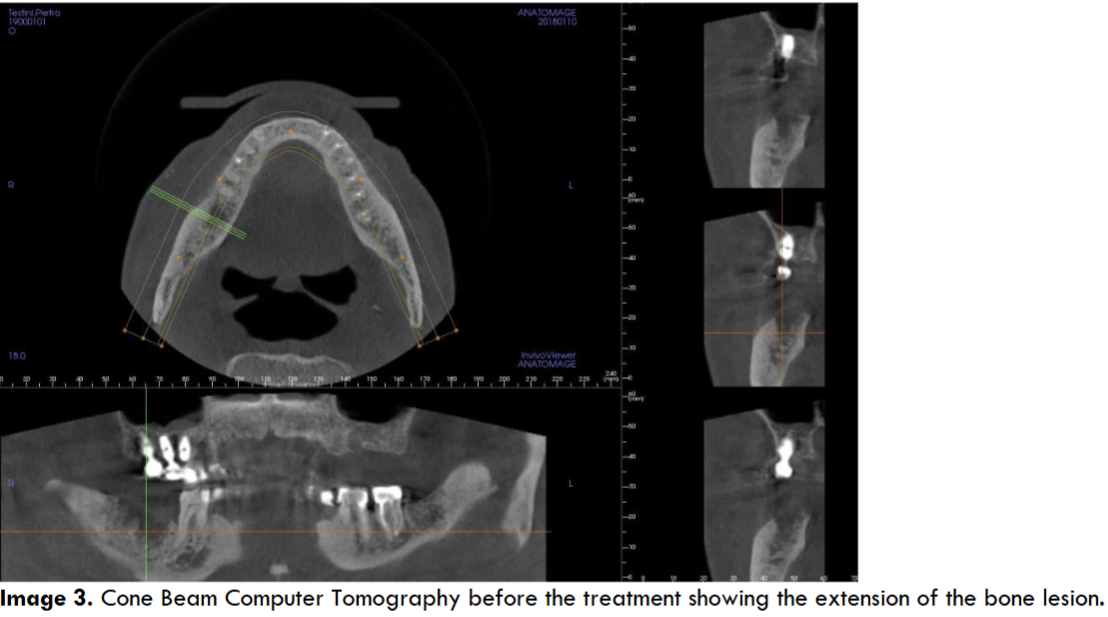
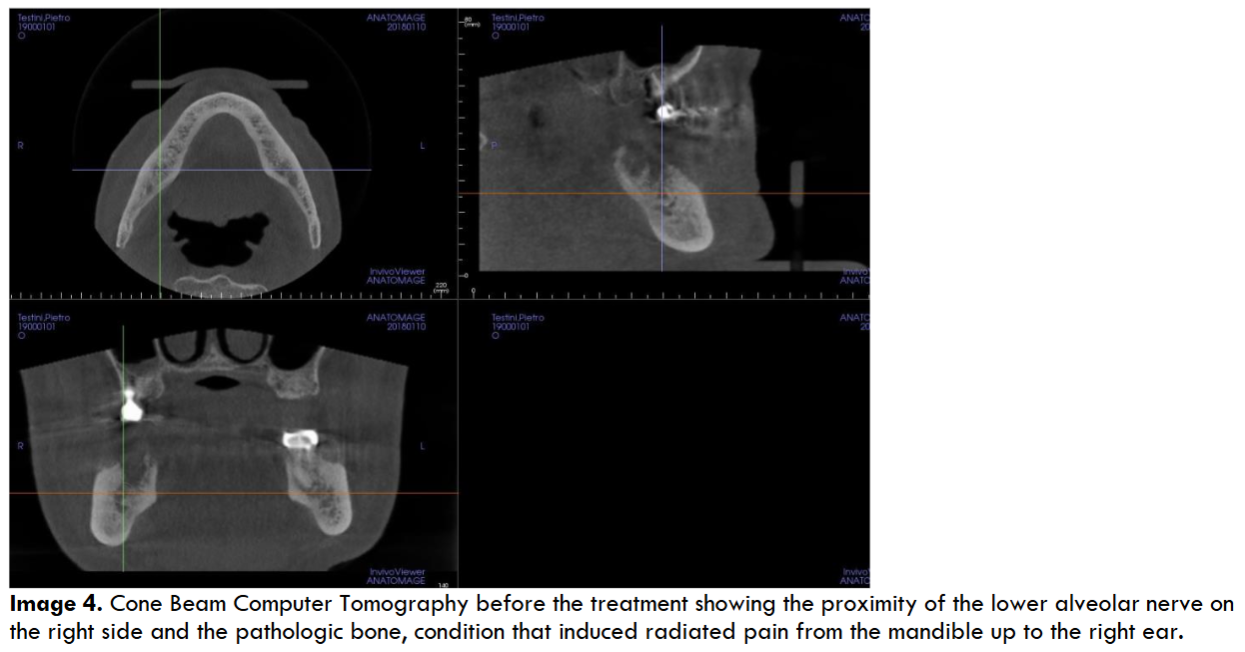
The lesion showed necrotic bone mixed with other parts in rapid growth: the cavity arrived so much deep that the lesion interested the lower alveolar nerve, causing a continuous, severe and burning pain interesting the mandible and radiated to the right ear, causing a worsening of the patient’s quality of life. Since his clinical conditions were very compromised above all for a severe heart failure it was decided to avoid any surgical approach, and the applied therapy was just a local disinfection and antibiotic drugs in case of infection. Moreover the patient used a lot of drugs (furosemide 125 mg twice a day, acetilsalicilic acid 100 mg once a day, Ivabradine 2.5 mg twice a day, Canrenone 50 mg a day, Silodosin 8 mg once a day and pantoprazole 40 mg once a day), and above all he used zolendronic acid (Zometa®) to control the bone metastasis growth derived from the prostatic cancer: this condition increased the risk to have a BRONJ as a postsurgical complication. However, for a continuous worsening of the symptoms and for the several infections of the mandibular lesion we decided, in agreement with his relatives, to surgically remove the gingival lesion cleaning the bone cavity with a conservative approach. To reduce the risk of postsurgical infections and of a bad healing (due to the zolendronic acid and the clinical conditions of the patients) we decided to fill the residual cavity with PRGF®-Endoret® autologous membranes, a particular platelet concentrate that improves and stimulates the healing processes inducing a good tissue regeneration. The Cone Beam Computer Tomography (CBCT) showed the extension of the bone lesion (images 3-4).
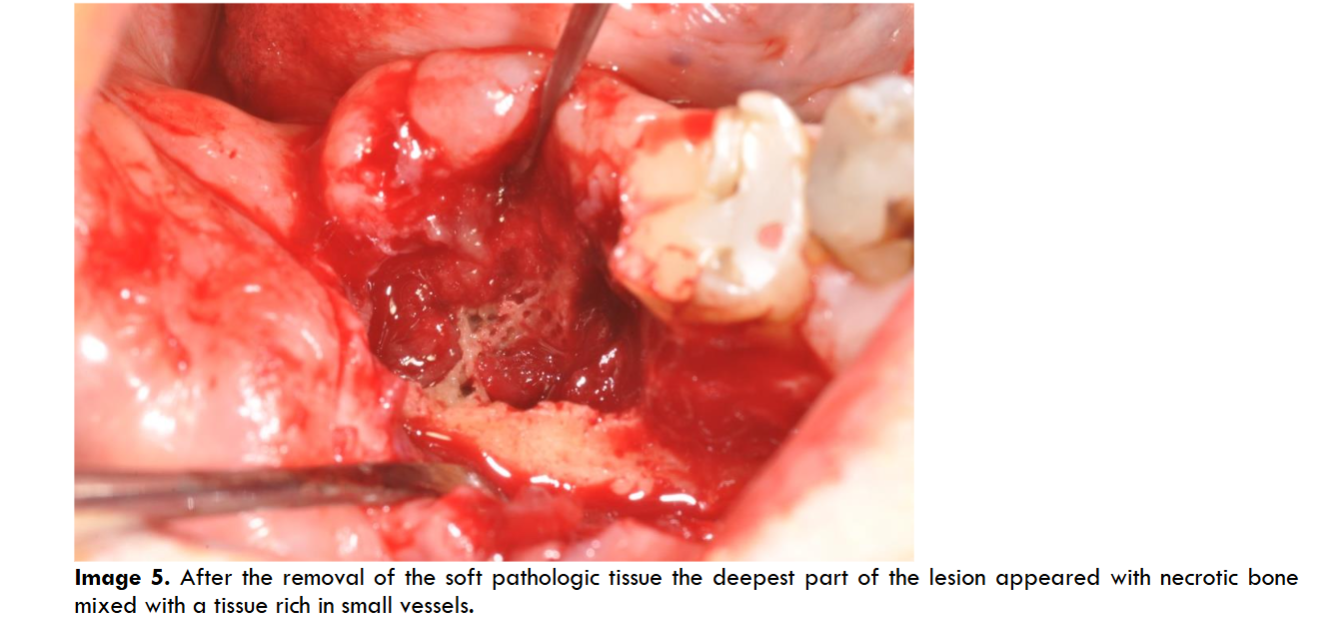
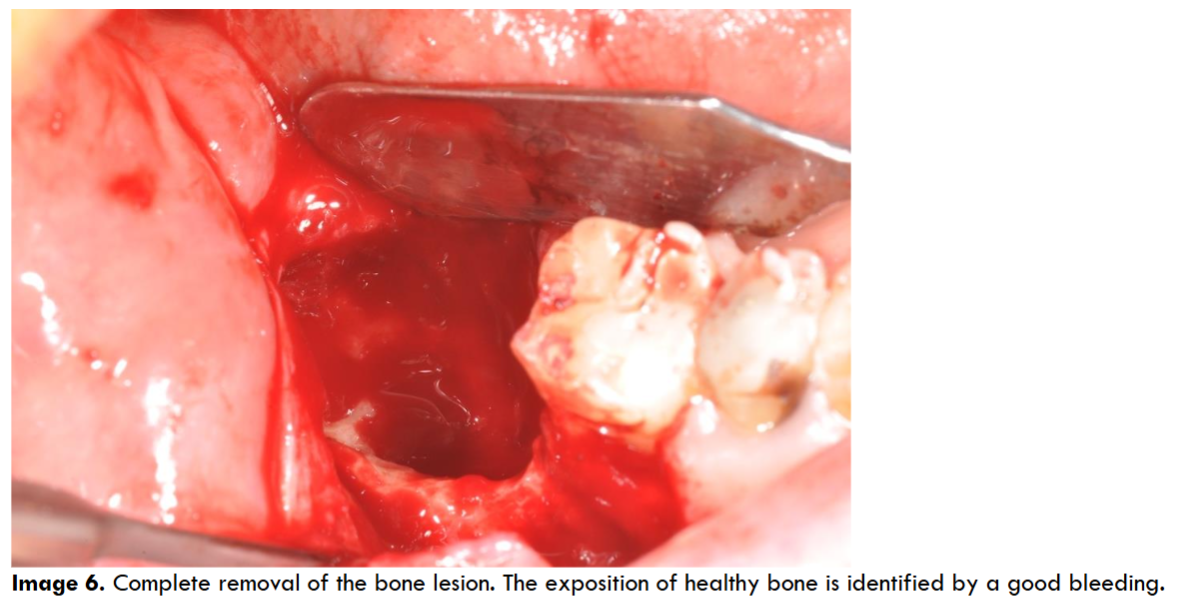
After the local anesthesia (with articain 4% with adrenaline 1:100.000, although the heart problems, but we needed a bleeding control) we opened a gingival flap removing the exophitic neoformation. The cortical bone was complete on the lingual side with a partial loss on the vestibular side: there was a big cavity that destroyed the alveolar edge behind the last residual molar (image 5). The cleaning of the upper part of the lesion made us to reach the deepest part of the bone lesion where it was possible to find granulation tissue with poor vessels and abundant necrotic bone. We completely removed these tissues with manual instrument and with ultrasonic instruments to have a total debridement of the cavity and to improve the bleeding from the residual bone walls (image 6). The necrotic bone surrounding the alveolar nerve was totally removed too.
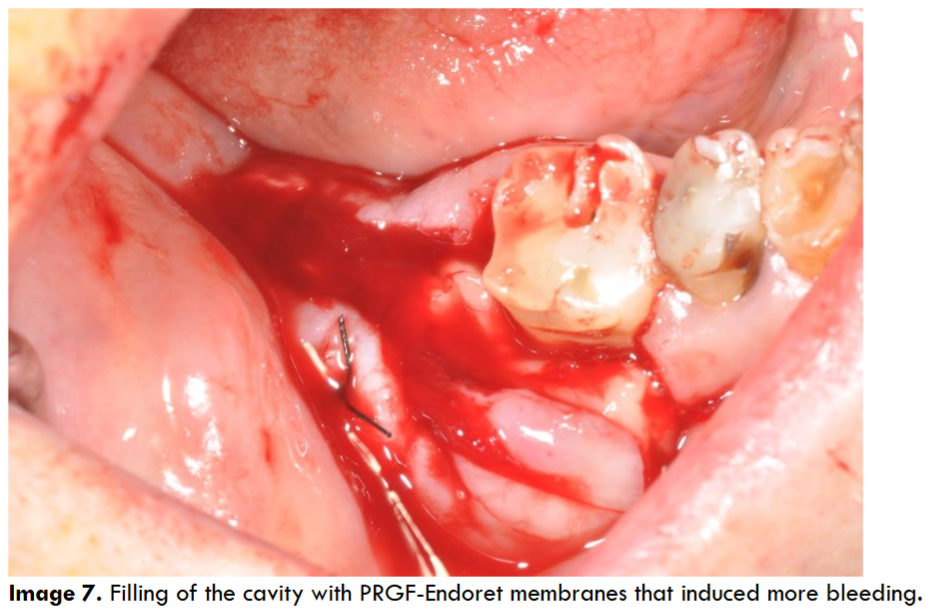
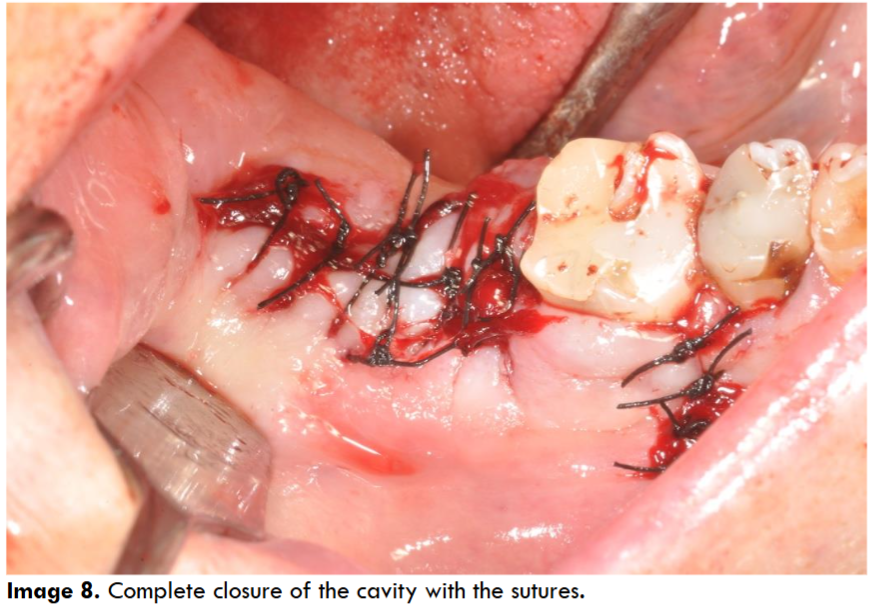
At the end of the cleaning, the cavity was filled by PRGF®-Endoret® autologous membranes to improve the healing processes: indeed, the PRGF improves the formation of new vessels (neoangiogenesis) stimulating the cells migration and differentiation. Immediately after the PRGF application in the cavity an important bleeding appeared due to the opening of the vessels of the surrounding tissues: this is a typical phenomenon of the PRGF application (image 7). It seems that the freedom of nitric oxide from the PRGF is the cause of this bleeding for release of the smooth musculature of the vessels. However, the presence of fibrin clot autologous membranes, another product derived from the PRGF, stopped the bleeding almost immediately (image 8).
The release of platelet’s growth factors promotes several biochemical results: the fibrin clot reduces the risk of bleeding, the increase of the new vessels formation (neoangiogenesis), a chemotactic effect on the cells coming from the surrounding tissues and their transformation in osteoblastic direction (when PRGF is into a bone cavity): indeed, thanks to the degranulation of platelets there is a release of several growth factors (GFs) which are key elements of any healing process. Moreover PRGF®-Endoret® reduces the risk of infections of the wound because the plasma is rich of several molecules of the humoral immunity: antibacterial molecules and immunoglobulins inhibit bacterial growth in the grafted material despite the absence of a protective gingival covering. The real problem was the risk to use an autologous biomaterial rich in growth factors in a part of the body where there probably were some residual cancer cells as the scintigraphic exam showed: anyway, the clinical conditions of the patient, his age and the pain he suffered for several months moved us to take the risk for a surgical approach. To reduce the risk of a bad healing we decided, in accord with the family members, to use pure platelets concentrate (a P-PRP) as PRGF-Endoret. Moreover, we were conscious that there was the risk of a stimulation of the growth of the cancer cells, and for that reason the debridement and the cleaning of the cavity was extremely accurate. To remove the necrotic tissue surrounding the alveolar nerve the cleaning of this part needed a particular attention and precision with lot of difficulties: despite this, there was no problem for the sensibility of this nerve without residual anesthesia or paresthesia.
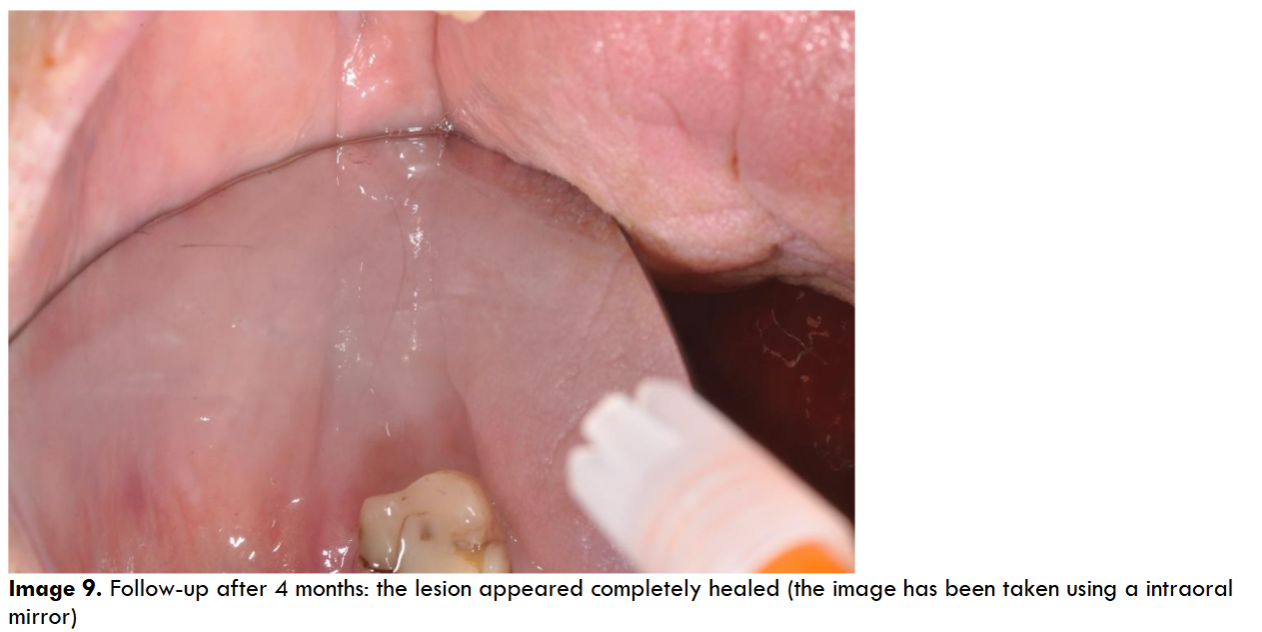
The post-surgery pharmacological protocol included a broad-spectrum antibiotic coverage (amoxicillin cps 1 gr x 3 times a day for 8 days from the day before surgery), accompanied by rinsing with 0.2% chlorhexidine-based mouthwash (1 minute for 3 times a day until stitches removal for 12-14 days). To control the inflammation, corticosteroid drugs for three days (deltacortene cps 5 mg) and granular ibuprofen 600 mg 2-3 times daily as needed was prescribed. The patient had acute pain and swelling for 4 days, well controlled by the anti-inflammatory drugs. The sutures were removed after 14 days and one month later the wound appeared in good conditions, instead the healing was not complete and the gingival flaps were divided by a defect. Anyway, the pain was completely solved (both localized or irradiate to the right ear), no bleeding and no infections into the gingival socket. After 4 months the gingival defect healed completely without any other drug or surgical therapy.
The results of this treatment were stable with a good gingival and bone healing, without any relapse of pain. Unfortunately, the patient died 18 months later for the worsening of his heart problems.
Discussion
It is well showed that the use of PRGF-Endoret, a particular platelet concentrate used both in liquid and gel form, allows to complete surgical procedures in patients without any medical problem or in patients with different problems as diabetes, natural immunodepression or induced by drugs, problems of coagulation or bone necrosis due to chemo- or radiotherapy (BRONJ or MRONJ). These good effects are the result of the rapid neoangiogenesis induced by the PRGF-Endoret, and this is very important to have a rapid healing and cell colonization of the wound. For that reason the use of PRGF-Endoret (or in general the PRPs) improves the healing of the tissue after any kind of trauma, above all in case of surgery. In addition, they can reduce post-surgical pain thanks to the freedom of several molecules, as plasmatic endocannabinoids and HGF (Hepatocitic Growth Factor) from the platelets: this growth factor blocks the NF-kB cascade of inflammation with good effects on inflammation and pain control. By a microbiological point of view several substances concentrated into the PRGF-Endoret membranes have antibacterial effects, reducing post surgical infection of the wound. For all these reasons we decided to use PRGF-Endoret in this case improving healing of a very suffering (and very delicate) patient. However, several studies showed that growth factors can stimulate the tumor progression, namely clonal expansion, invasion across tissue barriers, angiogenesis, and colonization of distant niches. For these reasons the use of platelets concentrates as PRGF-Endoret is normally counterindicate in the surgical treatments of tumors: however, the critical clinical conditions of our cardiopathic patient, his life expectancy, the bad quality of life for the continuos pain moved our choice to use the PRGF-Endoret to improve the healing reducing the risks of infections, and the related pain. In fact, the postoperatory pain was well controlled by using anti-inflammatory drugs and one month later the wound appeared in good conditions, instead the healing was not complete and the gingival flaps were divided by a defect. Anyway the chronic pain was completely solved (both localized or irradiate to the right ear), there were no bleeding and no infections into the gingival socket. After 4 months the gingival defect healed completely without any other drug or surgical therapy.
Conclusions
This paper showed how the use of PRGF-Endoret, a particular kind of autologous platelets concentrate (PRP), improves the healing of surgical wounds also in a clinically compromised patient, instead his metabolic energies were low. PRGF-Endoret helps in any surgical treatment reducing post-surgical pain, bleeding and risk of infections. Moreover, the increased neoangiogenesis, chemotaxis and the stimulation of these new cells allows to recreate the architecture of the new connective tissue and the epithelium. These results are visible both on normal patients or in patients with difficult healing, suffering from diabetes, medical pathologies, immune pathologies or in treatment with drugs that can disturb the normal healing, as immunodepressant, corticosteroids or bisphosphonates drugs as the described case. In fact we described a case of a cardiopathic old patient who suffered from prostathic cancer with mandibular methastasis, causing a massive bone necrosis associated to cancer metastasis in the right part of the body of the mandible. The patient had low metabolic activities and his quality of life was very low for the chronic pain interesting the right mandible, the lateral part of the face and the right ear. Moreover, the metastatic lesions coming from the prostate cancers reduced his life expectancy. For all these reasons, in according with family members, we decided to treat him with a surgical approach: the aim was to reduce the continuous pain and the several infections interesting the mandible. The routinary use of PRGF-Endoret allowed us to suggest this kind of treatment helping the surgical approach because by a biological point of view it is a system that amplify the natural healing chances reducing at the same time the risks of a postsurgical infection. The described case confirmed our expectations and the result was very good, facilitating the tissues healing and solving completely the mandibular lesion, despite the difficult clinical conditions of the patient and the use of drugs facilitating the MRONJ. Furthermore, although the use of PRP and growth factors could be dangerous when applied on tissues with previous cancer lesions, our experience shows that this risk is not definite and sure and could be reduced if the surgical cleaning is important, well conducted and extensive. Anyway the patient selection and his knowledge about the risks is very important because the possibility of growth stimulation of the residual cancer cells is always real. For these reasons in these kinds of problems the selection of the patients, their life expectancy and their clinical conditions are very important to decide if the benefits are more than the risks associated to the use of PRP. Anyway, more studies are necessary to confirm the possibility to use the PRP in the surgical treatment of the cancer or metastatic lesions. Analyzing these results we may conclude that the use of PRGF-Endoret can help the surgical treatment of patients in bad clinical conditions, improving their healing in case of surgery.
Acknowledgement
None to declare.
Financial Disclosure or Funding
None to declare.
Conflict of Interest
None to declare.
Informed Consent
The patient and their family members were adequately and properly informed about the limitations and risks of the whole surgical procedure and the use of different biomaterials; they were also informed about the possibility of publishing the case report and gave their consent to the publication of the text and images.
Author contributions
None to declare.
Data Availability
None to declare.
References
- Del Fabbro M, Gallesio G, Mozzati M. Autologous platelet concentrates for bisphosphonate-related osteonecrosis of the jaw treatment and prevention. A systematic review of the literature. J Cancer. 2015 Jan;51(1):62-74. doi: 10.1016/j.ejca.2014.10.015. Epub 2014 Nov 6.
- Mozzati M, Gallesio G, Gassino G, Palomba A, Bergamasco L. Can plasma rich in growth factors improve healing in patients who underwent radiotherapy for head and neck cancer? A split-mouth study. Craniofac Surg. 2014 May;25(3):938-43.
- Mozzati M, Gallesio G, Arata V, Pol R, Scoletta M. Platelet-rich therapies in the treatment of intravenous bisphosphonate-related osteonecrosis of the jaw: a report of 32 cases. Oral Oncol. 2012 May;48(5):469-74.
- Razmara F, Bayat M, Shirian S, Shabankare G, Mohamadnia A, Mortazavi M, Alijani MR, Bahrami N. Application of a collagen scaffold saturated with platelet-rich plasma in prevention of bisphosphonate-related osteonecrosis of the jaw in the rat animal model. Heliyon 2021 May 1;7(5):e06930. doi: 10.1016/j.heliyon.2021.e06930. eCollection 2021 May.
- Steller D, Scheibert A, Sturmheit T, Rose D, Hakim SG. Impact of PRP and PRF on Viability of Zoledronic Acid Treated Osteoblasts in 2D and 3D Cell Culture. Anticancer Res. 2022 Mar;42(3):1295-1299. doi: 10.21873/anticanres.15596.
- Huang Z, Ren PG, Ma T, Smith RL, Goodman SB. Modulating Osteogenesis of Mesenchymal Stem Cells by Modifying Growth Factor Availability. Cytokine 2010 Sep;51(3):305-10.
- Bai Y, Yin G, Huang Z, Liao X, Chen X, Yao Y, Pu X. Localized Delivery of Growth Factors for Angiogenesis and Bone Formation in Tissue Engineering. Int Immunopharmacol. 2013 Jun;16(2):214-23.
- Zhang L, Ai H. Concentrated Growth Factor Promotes Proliferation, Osteogenic Differentiation, and Angiogenic Potential of Rabbit Periosteum-Derived Cells in Vitro. J Orthop Surg Res. 2019 May 22;14(1):146.
- Lu W, Xu W, Li J, Chen Y, Pan Y, Wu B. Effects of Vascular Endothelial Growth Factor and Insulin Growth factor‑1 on Proliferation, Migration, Osteogenesis and Vascularization of Human Carious Dental Pulp Stem Cells. Mol Med Rep. 2019 Oct;20(4):3924-3932.
- Anitua E, Alonso R, Girbau C, Aguirre JJ, Muruzabal F, Orive G. Antibacterial effect of plasma rich in growth factors (PRGF®-Endoret®) against Staphylococcus aureus and Staphylococcus epidermidis strains. Clin Exp Dermatol. 2012 Aug;37(6):652-7.
- Bayer A, Lammel J, Rademacher F, Groß J, Siggelkow M, Lippross S, Klüter T, Varoga D, Tohidnezhad M, Pufe T, Cremer J, Gläser R, Harder J. Platelet-released growth factors induce the antimicrobial peptide human beta-defensin-2 in primary keratinocytes. Exp Dermatol. 2016 Jun;25(6):460-5.
- Witsch E, Sela M, Yarden Y. Roles for growth factors in cancer progression. Physiology (Bethesda). 2010 Apr;25(2):85-101. doi: 10.1152/physiol.00045.2009.
- Yang SY, Miah A, Pabari A, Winslet M. Growth Factors and their receptors in cancer metastases. Front Biosci. 2011 Jan 1;16:531-8. doi: 10.2741/3703.
- Anderson NM, Simon MC. The tumor microenvironment. Curr Biol. 2020 Aug 17;30(16): R921-R925. doi: 10.1016/j.cub.2020.06.081.
- Stefani C, Miricescu D, Stanescu-Spinu I, Nica RI, Greabu M, Ripszky Totan A, Jinga M. Growth Factors, PI3K/AKT/mTOR and MAPK Signaling Pathways in Colorectal Cancer Pathogenesis: Where Are We Now? Int J Mol Sci. 2021 Sep 23;22(19):10260. doi: 10.3390/ijms221910260.
- Shorning BY, Dass MS, Smalley MJ, Pearson HB. The PI3K-AKT-mTOR Pathway and Prostate Cancer: At the Crossroads of AR, MAPK, and WNT Signaling. Int J Mol Sci. 2020 Jun 25;21(12):4507. doi: 10.3390/ijms21124507.
- Anitua E, Pelacho B, Prado R, Aguirre JJ, Sánchez M, Padilla S, Aranguren XL, Abizanda G, Collantes M, Hernandez M, Perez-Ruiz A, Peñuelas I, Orive G, Prosper F. Infiltration of plasma rich in growth factors enhances in vivo angiogenesis and improves reperfusion and tissue remodeling after severe hind limb ischemia. J Control Release. 2015 Mar 28;202:31-9. doi: 10.1016/j.jconrel.2015.01.029. Epub 2015 Jan 24.
- Shahidi M, Vatanmakanian M, Arami MK, Shirazi FS, Esmaeili N, Hydarporian S, Jafari S. A comparative study between platelet-rich plasma and platelet-poor plasma effects on angiogenesis. Med Mol Morphol. 2018 Mar;51(1):21-31. doi: 10.1007/s00795-017-0168-5. Epub 2017 Sep 25.
- Sidiropoulou S, Papadaki S, Tsouka AN, Koutsaliaris IK, Chantzichristos VG, Pantazi D, Paschopoulos ME, Hansson KM, Tselepis AD. The Effect of Platelet-Rich Plasma on Endothelial Progenitor Cell Functionality. Angiology. 2021 Sep;72(8):776-786. doi: 10.1177/0003319721998895. Epub 2021 Mar 8.
- Bendinelli P, Matteucci E, Dogliotti G, Corsi M, Banfi G, Maroni P, Desiderio MA. Molecular basis of anti-inflammatory action of platelet-rich plasma on human chondrocytes: mechanisms of NF-κB inhibition via HGF. J Cell Physiol. 2010 Nov;225(3):757-66. doi: 10.1002/jcp.22274.
- Karakaş DO, Dandin O, Müftüoğlu T, Tihan D, Bal AS, Yıldırım S. Effect of platelet-rich plasma on postoperative peritoneal inflammation and adhesions. Arch Med Sci. 2020 Apr 18;17(5):1408-1413. doi: 10.5114/aoms.2020.94538. eCollection 2021.
- Solakoglu O, Heydecke G, Amiri N, Anitua E. The use of plasma rich in growth factors (PRGF) in guided tissue regeneration and guided bone regeneration. A review of histological, immunohistochemical, histomorphometrical, radiological and clinical results in humans. Ann Anat. 2020 Sep;231:151528.
- Anitua E, Alonso R, Girbau C, Aguirre JJ, Muruzabal F, Orive G. Antibacterial effect of plasma rich in growth factors (PRGF®-Endoret®) against Staphylococcus aureus and Staphylococcus epidermidis strains. Clin Exp Dermatol. 2012 Aug;37(6):652-7. doi: 10.1111/j.1365-2230.2011.04303.x. Epub 2012 Feb 14.
- Pourkarim R, Farahpour MR, Rezaei S. Comparison effects of platelet-rich plasma on healing of infected and non-infected excision wounds by the modulation of the expression of inflammatory mediators: experimental research. Eur J Trauma Emerg Surg. 2022 Feb 12. doi: 10.1007/s00068-022-01907-0.

