Growth Sparing Techniques in Early Onset Scoliosis
Does growth sparing techniques improve lung function tests in idiopathic Early Onset Scoliosis – A Retrospective Single Centre Analysis
Sai Gautham Balasubramanian MS(Ortho), DNB(Ortho), MRCSEd 1; Boresh Dhamija MS, MCH(NS), FRCSEd (NS) 1; Colin Bruce FRCS (T&O) 2; Neil Davidson FRCS (T&O) 3; Jayesh Trivedi FRCS (T&O) 3; Sudarshan Munigangaiah MRCSI, MSc (T&Orth), MCh (T&Orth), FRCSI (T&Orth) 3- Consultant Spine Surgeon, Alder Hey Children’s NHS Foundation Trust, Liverpool, L14 5AB, United Kingdom
OPEN ACCESS
PUBLISHED: 31 December 2024
CITATION: BALASUBRAMANIAN, Sai Gautham et al. Does growth sparing techniques improve lung function tests in idiopathic Early Onset Scoliosis – A Retrospective Single Centre Analysis. Medical Research Archives, [S.l.], v. 12, n. 12, dec. 2024. Available at: <https://esmed.org/MRA/mra/article/view/6121>.
COPYRIGHT: © 2025 European Society of Medicine. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
DOI: https://doi.org/10.18103/mra.v12i12.6121
ISSN 2375-1924
Abstract
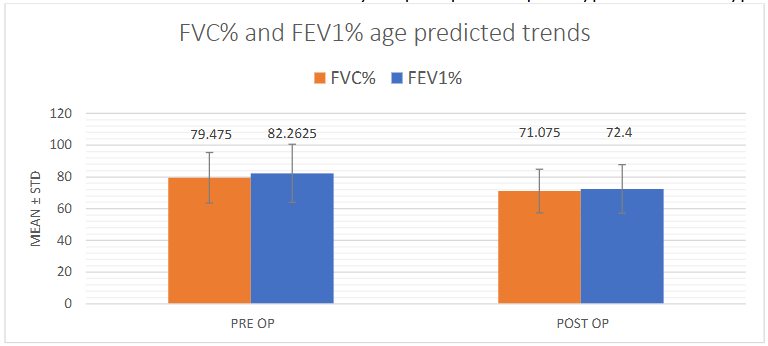
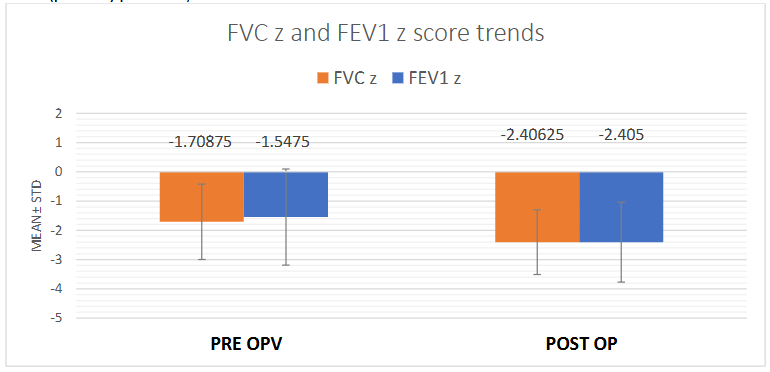
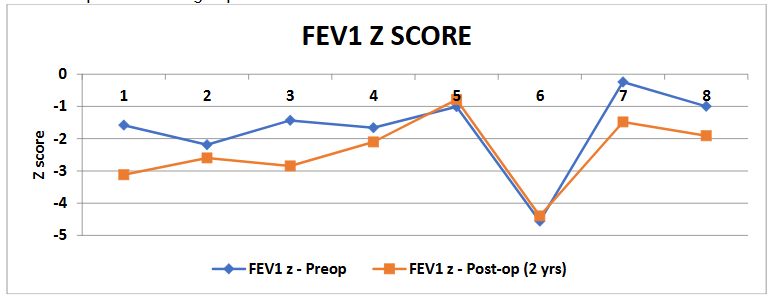
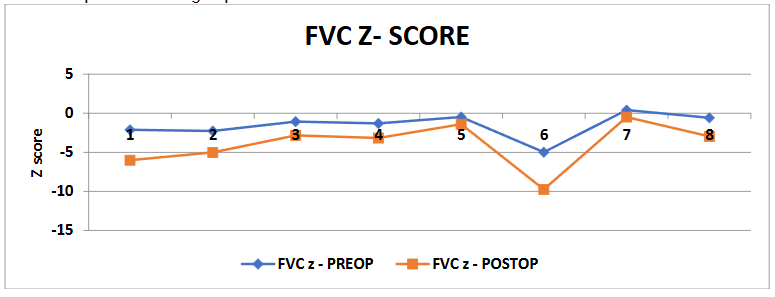
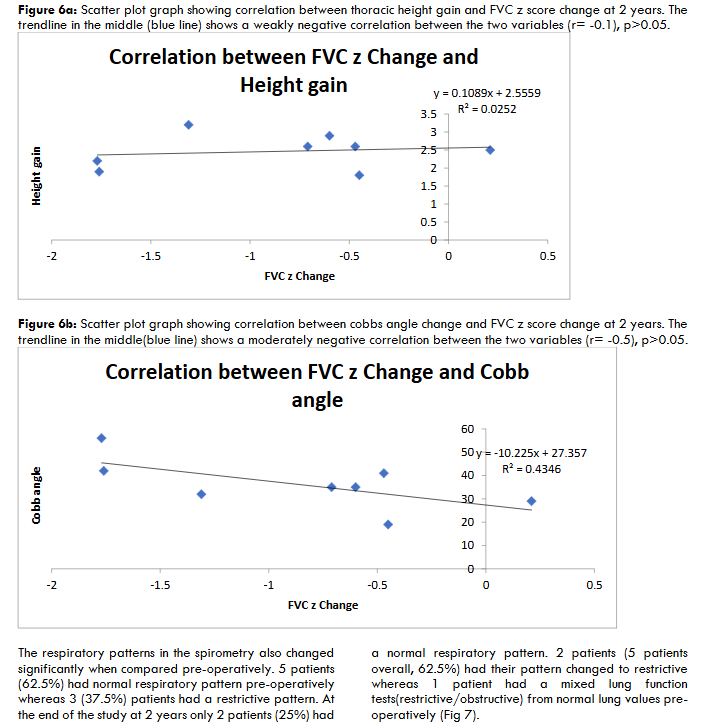
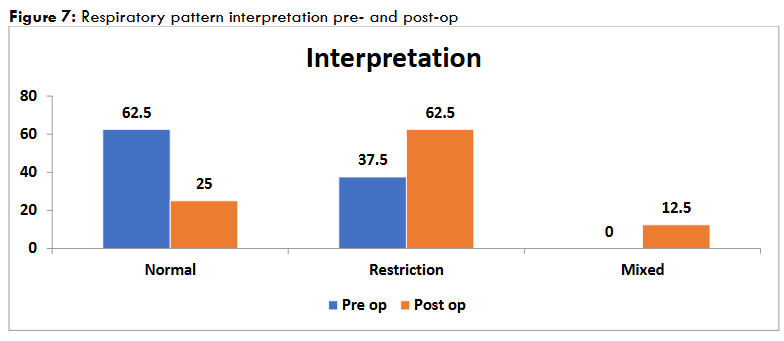
Introduction: Growth-sparing surgical strategies are routinely employed in Early Onset Scoliosis to allow for thoracic cavity growth and lung development along with spinal growth. Pulmonary function tests (PFT) are measured pre- and post-operatively to assess improvement of respiratory functions. The general consensus is that growing rods are associated with an improvement in pulmonary function compared to early fusion. We aimed to analyse and compare the pre- and post-op PFTs to assess any statistically significant improvements in the lung functions. Methods: We conducted a retrospective study of all surgically managed patients with idiopathic Early Onset Scoliosis with minimum 2 years follow up. Radiological parameters and Pulmonary function tests were observed and compared. The FEV1 and FVC were measured, and the age-predicted values were calculated along with z score change of FEV1 and FVC pre-and post-operatively. The correlation between thoracic height gain and change in PFTs was also calculated. Results: Overall, 28 patients had underwent growing rods insertion for EOS in 2016-2018 at Alder Hey Children’s Hospital, Liverpool, UK. 17 idiopathic EOS patients were included in the study, out of which 8 were included. The average T1-T12 height gain was 2.5 cm. Both the mean FEV1 and FVC increased with age(p<0.0001) due to the lung growth. However, the mean age predicted percentage values were decreased for both FEV1(p<0.05) and FVC (p<0.01). The z scores were also reduced/negative for both values (p<0.05). There were moderate negative correlations between FEV1 and FVC z score change with cobbs angle change indicating worsening of lung function tests at a short term follow up. Conclusion: This study suggests improvement in FEV1 and FVC with thoracic height gain. There was a negative impact on pulmonary function tests with greater change in cobb angle over a short period of time (2 years) or greater the acute distraction, as indicated by negative correlations between % predicted and z-score values of FEV1, FVC or FEV1/FVC ratios. Longer-term studies are essential to demonstrate the efficacy of treatment related to pulmonary functions in idiopathic Early Onset Scoliosis.Keywords
- Early Onset Scoliosis
- Growth Sparing Techniques
- Pulmonary Function Tests
- FEV1
- FVC
- Cobb Angle
Introduction
Early Onset Scoliosis (EOS) is defined as a three-dimensional coronal plane deformity with age of onset less than 10 years. EOS is often associated with loss of pulmonary functions and significant cardiopulmonary morbidities as the curve progresses without any intervention. EOS results in restrictive lung changes with loss of chest wall compliance and loss of lung volumes. This is due to a combination of physical constraints of thoracic cavity in a scoliotic spine along with poor development or asymmetrical underdevelopment of lung tissues. The most rapid and exponential growth of alveoli occurs during the first 8 years of life. Hence, it becomes necessary to prevent the progression of curvatures in young children with an aim to improve lung functions and to avoid thoracic insufficiency syndrome (TIS). Growth sparing surgical strategies like traditional or magnetic controlled growing rods (MCGR) are routinely employed in Early Onset Scoliosis (EOS) to allow for thoracic cavity growth and lung development along with spinal growth. This has been one of the most acceptable or rather the only available management option for EOS currently. Early spinal fusion to arrest the curve progression has been frought with complications of limiting chest growth and lung functions. TIS associated with early fusion procedures are widely accepted and a proven concept in patients with EOS. Hence the main management strategy in such patients involves implantation of growing rods and serial distractions until the patients graduate sufficiently to a final posterior instrumented fusion after adequate completion of their growth. Pulmonary function tests (PFT) including Vital capacity, FVC, FEV1 are measured in these patients to measure and monitor improvement of respiratory functions pre- and post-operatively. Such growing rods had proven to be effective in neuromuscular EOS patients with improvement in pulmonary functions. However, PFTs in idiopathic EOS have been studied sparsely. The general consensus is that the growth sparing methods are associated with an improvement in pulmonary function compared to early fusion. Our aim was to analyse patients with idiopathic EOS and to compare the pre- and post-op PFTs to assess whether there is any statistically significant improvements in the lung functions post-operatively.Material and Methods
We conducted a retrospective study of all surgically managed patients with idiopathic EOS with age at diagnosis <10 years of age. All the patients included in the study had growing rods inserted when the cobbs angle reached more than 50 degrees and were progressive with growth. These patients had a trial of casting under GA/bracing to control the curve progression when the age at diagnosis was less than 5 years of age. Those who failed conservative management were subsequently included for the insertion of growing rods. The study was conducted between the time period of 2016-2018 with a minimum of 2-year follow-up. Overall, 28 patients had underwent growing rods insertion for EOS at Alder Hey NHS Children’s Hospital, Liverpool, United Kingdom. The patients were treated surgically with standard insertion of growth rods (traditional/MCGR) at the stable/neutral vertebrae depending on the curve pattern and magnitude of the scoliotic curve. Out of 28 patients, only 17 had a idiopathic condition. The rest of the 11 patients were neuromuscular, syndromic and congenital hence they were excluded from the study. Demographics, radiological parameters and pulmonary function tests were observed and compared. The spirometry was done for all surgically planned patients pre-operatively and around 2 years post-operative period. The spirometry was done by the senior respiratory technician after adequate instructions to the children as per standard protocol. The test itself was repeated for 3 times to check the adequacy and repeatability of the acquired respiratory loops and curves. The quality was in turn graded from A to E (best to no acceptable loops). The tests were accepted only when the quality of the curves was adequate and repeatable. Out of 17, only 8 patients had a reproducible and acceptable pre- and post-operative pulmonary function test. The rest of the 9 patients had either just a post-operative PFTs or could not adequately perform PFTs pre-operatively and hence were excluded. All the patients included in the study during this time period had Magnetic Controlled Growing Rods (MCGR) inserted. The MCGR were sequentially distracted remotely under ultrasound guidance every 3 months by a specialist nurse/consultant. Post-op X-rays were taken to observe the height gain after each distraction along with implant status. The FEV1 and FVC were measured pre- and post-operatively, and the age predicted percentage values were calculated using the Stanojevic equations and Global Lung function Initiative (GLI 2012). The GLI provides reference values for lung function indices calculated with spirometry such as FEV1, FVC, FEV1/FVC, FEF25%, FEF 75% etc among others. The reference values are age, sex and height dependent and hence measured prior to the test pre- and post-op. The Upper and Lower Limits of Normal (ULN and LLN) were noted based on the reference values for a particular age, sex and height. The z score change of FEV1 and FVC pre- and post-operatively were calculated to indicate decline/improvement in lung functions. Z-score indicates how many standard deviations a measurement is from its predicted value usually mean +/- 2 SD. A value of LLN -1.64 is considered as a cut off to indicate presence of lung function decline in patients for that particular age, sex and height. Z scores were calculated pre- and post-operatively independently from the GLI reference values and the change in values were also measured and analysed. The Cobbs angle and T1-T12 height were calculated pre-op, post-op and at 2 years follow up using whole spine standing X rays or low radiation EOS images. The pattern of respiratory outcome was also analysed pre- and post-operatively. Non-parametric correlations(r) between %predicted values, z score changes and cobbs angle change, thoracic height gain over a period of 2 years were studied to assess if lung functions improved with increase in T1-T12 height or correction of cobb’s angle. Throughout the analysis, p<0.05 is considered statistically significant and r values were calculated for correlation analysis (r>0.5).Results
Eight patients, who had a reproducible respiratory function test, were included in the study (2 male, 6 female). 3 patients had age at diagnosis < 3 years of age and were given a trial of casting/bracing. 5 patients were < 10 years of age and were monitored every 6 months with radiological and clinical assessment to review the progression of the curve with a spinal brace. The patients were offered surgical management with growing rods once the cobbs angle reached > 50 degrees and pre-pubertal/Rissers grade 0 with atleast more than 2 years of growth left.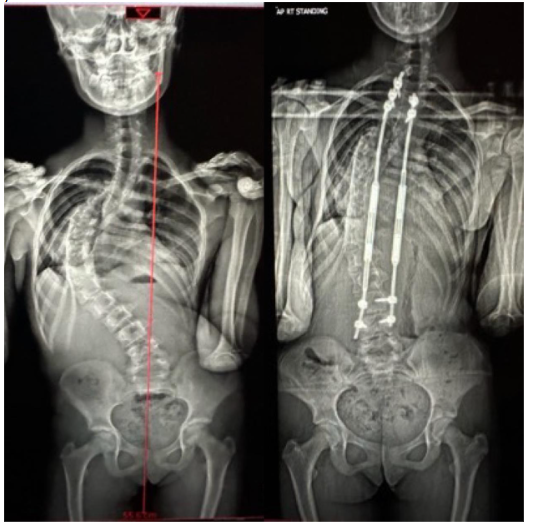
Discussion
EOS is a highly challenging condition to treat surgically as it includes multiple procedures on the children including lengthening of the growing rods or other growth friendly techniques. Apart from the multiple surgical procedures, loss of pulmonary function is a major factor with progressive EOS. EOS is viewed as a multi systemic disorder apart from spinal deformity due to inhibition of thoracic spinal growth resulting in TIS. Early spinal fusion is no more an option in these children as it is fraught with multiple complications of limiting the spinal and lung growth apart from restricting the lung functions in their maximal alveolar growth phase. Early fusion leads to reduction in the height and volume of the thoracic spine which in turn results in severe restrictive lung disease.
This led to the development and evolution of growth sparing techniques to manage EOS and progressively increase the thoracic height along with the breathing units or lung functions. These techniques limit the rotation and torsion of the spine associated with the scoliosis which in turn leads to better excursion of the thorax and increase the lung compliance. However, these can also lead to auto fusion in the immature spine due to violation of the native anatomy and fusion of the facets. Such auto fusions can severely impair the further growth of the thoracic spine and the thoracic volume. Hence, frequent distractions are necessary to allow the immature lung to develop in EOS. A thoracic height of 18cm is currently proposed as a cut off value by Johnson et al 21 for thoracic adequacy and fusion of the facets. Such auto fusions can severely impair the further growth of the thoracic spine and the thoracic volume. Hence, frequent distractions are necessary to allow the immature lung to develop in EOS. A thoracic height of 18cm is currently proposed as a cut off value by Johnson et al 21 for thoracic adequacy and fusion of the spine. This cut off value is considered to be translated into a better clinical outcome at long term follow up from cardiopulmonary standpoint.
Lung development increases exponentially along with spinal growth in young children until age 8 and plateaus thereafter till 10 years of age. The growth and development of the spine and thorax occurs in a synchronized manner early in life. The thoracic volume is modified as the spinal deformity progresses early in life. This is most significant in children under 8 years of age when the apical vertebrae protrude within the thorax with thoracic lordosis which further complicates the chest wall compliance and normal expansion of the thoracic cage. Hence, it becomes crucial to support the thoracic growth with sequential distraction of the growing rods instead of early spinal fusion.
The management of EOS is currently emphasized more on the follow up and improvement of lung functions than the actual deformity correction. The focus is on the thoracic mobility after surgical treatment where there is a significant reduction in chest wall compliance along with reduction in lung functions in surgically treated patients due to posterior tethering of the thoracic spine with growing rods. Spirometry is the diagnostic method of choice currently to understand the severity of pulmonary disease pre- and post-operatively in surgically managed patients. However, the question arises regarding the feasibility and reliance of this diagnostic test in young children as it is difficult in providing meaningful results as it is a highly subjective test in this age group. As a result, any outcome is reported in thoracic spinal height which is not a reliable indicator due to multiple variables involved in EOS. These growth sparing techniques had a significant impact in juvenile neuromuscular scoliosis patients with multiple, albeit smaller study groups. Their lung functions had improved manifolds in their final follow-up.
The lung functions have been sparsely studied in idiopathic Early Onset Scoliosis patients. Some studies showed a stable or improvement in lung functions over a short term follow up. Wang et al reported a long term improvement in lung functions and no correlation between improvement in PFTs and radiological improvement. Multiple studies have noted improvement an actual FEV1 and FVC values, however, failed to notice an improvement in %predicted values. Our study also has similar findings and also finds a negative correlation with cobbs angle change, meaning a greater change in cobbs angle over a short period of time can actually has a negative impact by stiffening up the thoracic spine, hence, low chest compliance and chest mobility. The respiratory muscles were significantly weaker in surgically treated EOS patients in this study. Glotzbecker et al 24 suggested that we need to move away to more objective tests as radiological parameters had never correlated with pulmonary function tests. Hence, the suggestion was to move on to 3D thoracic volume and excursion in young patients correlated with pulmonary function tests.
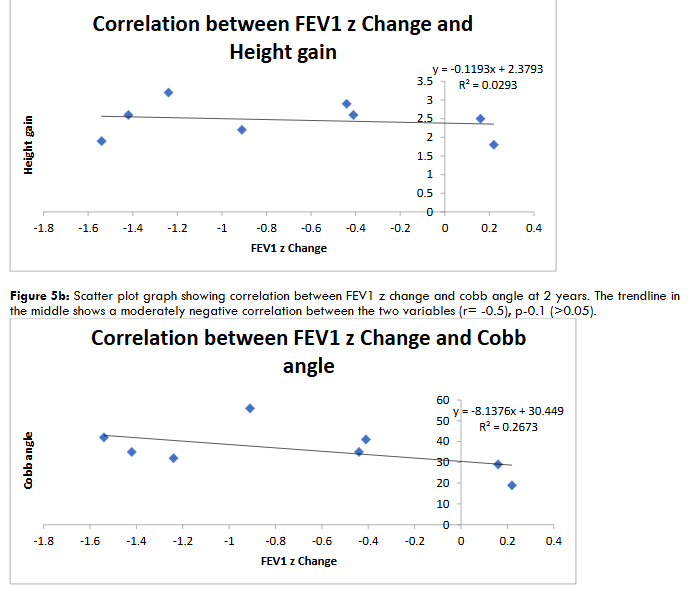
We noted a significant improvement in lung function tests both, %predicted and z score values at the end of 2 years with a statistically significant p value of <0.05. These values also negatively correlated with the thoracic height again and reduction of cobbs angle achieved over the 2 years. However, due to the small study group these values were not statistically significant. Nevertheless, this echoes the study by Johnson et al that the effect of curve correction has a moderate negative correlation on pulmonary function tests (R value of -0.5 in our study) and minimal to no effect on thoracic height again achieved (R value of -0.1 in our study). The % predicted values of FEV1 and FVC also had similar results.
The patients who did not undergo early fusion had better clinical outcomes at the end of their graduation. The PFTs did not have any correlation with the radiological parameters, however this had an impact in the clinical outcome scores. As apart from the severe mental, psychological impact of undergoing multiple anaesthetic and surgical procedures. These improvements tend to occur over a long time or maintain the trendline values following the initial improvement. Nevertheless, the severe EOS groups where the % predicted values were less than 60% from the start, the outcome at the end of long term follow up or at graduation were not promising.
they had maintained the baseline values until the end of follow up when compared to lesser curves.
It also seems likely that %FVC or %FEV1 of <60% prior to maturity is unlikely to avoid respiratory morbidity from TIS, regardless of T1-T12 height exceeding 18 cm and irrespective of surgical treatment. All these studies and research points to early aggressive management of progressive EOS to maintain lung functions and an adequate reliable method of measuring the PFTs other than spirometry and 2D thoracic measurements. Redding et al reported cobbs angle or the thoracic height gain does not necessarily correlate with the PFTs and hence the respiratory outcome.
Finally, our study is not without limitations. This is a single centre retrospective analysis of patients with smaller population group to arrive at a meaningful result. The mean age of population group was >8 years which is around the time their alveolar development and microarchitecture had been fully established and hence the pre-op PFT values were well above 60% in the study group. One interesting observation from the excluded group were that 6 out of 9 patients were <8 years of age to start with and hence would have been the more useful and meaningful patient group to analyse the lung function tests. Finally, although some of the correlations were statistically significant, the weak correlations make it more difficult to suggest that there is clinical confidence that what is being measured is something meaningful.
This analysis raises more questions than providing a meaningful conclusion. Is spirometry a valid test for younger population to measure PFTs, as most of the researchers has moved away into objective tests such as thoracic 3D volumes, plethysmography, gas dilution and diffusion gas analysis which takes the patient bias off the study. The sleep study is the most reliable investigation of all to measure PFTs. However, this has been sparsely employed due to lack of adequate resources in the clinical scenario. These diagnostic tests have a very important role in understanding whether we are indeed changing the course of natural history of EOS or if we are simply slowing down the ultimate inevitable pulmonary decline. Elaborate multicenter studies with standardization of the most specific and sensitive diagnostic tests are needed to arrive at meaningful conclusions as the natural history of EOS after surgical treatment is one of the poorly understood and researched condition due to sparsity of available treatment methods and inadequate resources.
Conclusion
This study suggests improvement in absolute values of FEV1 and FVC with thoracic height gain. A decline in age predicted percentage and z scores of FEV1 and FVC were noted, at minimum 2 years post-operatively, in spite of improvement in absolute values with growth. There were negative correlations in PFTs with thoracic height gain and cobbs angle changes without any statistical significance. Also, moderate negative correlations were noted with cobbs angle reduction and PFTs. There was a negative impact on pulmonary function tests with greater change in cobb angle over a short period of time (2 years) or greater the acute distraction, as indicated by negative correlations. Longer term studies and the most adequate objective diagnostic tests, other than spirometry, are essential to demonstrate the efficacy of treatment related to pulmonary functions in idiopathic EOS.
Acknowledgements
SOURCE OF FUNDING – Nil
CONFLICTS OF INTERESTS – Nil.