Occupational Risks of Resin-Based 3D Printing in Dentistry
Assessing the Occupational and Environmental Risks of Resin-Based 3D Printing in Dental Clinics: Airborne Chemical Emissions and Mitigation Strategies
Adam Brian Nulty1*
OPEN ACCESS
PUBLISHED: 30 December 2024
CITATION: Nulty, A.B. 2024. Assessing the Occupational and Environmental Risks of Resin-Based 3D Printing in Dental Clinics: Airborne Chemical Emissions and Mitigation Strategies. Medical Research Archives, Volume 12 Issue 12.
COPYRIGHT: © 2025 European Society of Medicine. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
DOI: https://doi.org/10.18103/mra.v12i12.6043
ISSN 2375-1924
Abstract
3D printing has become a pivotal technology in digital dentistry, enabling the production of highly customized dental products, prostheses, and orthodontic devices. Despite its advantages, the adoption of this technology raises significant occupational and environmental concerns, particularly regarding indoor air quality and the health of dental professionals and patients. This review aims to assess the airborne chemical emissions associated with resin-based 3D printing processes in dental clinics and to propose mitigation strategies to minimize exposure risks.
Keywords
3D printing, dental clinics, airborne emissions, occupational health, environmental risks, mitigation strategies
1. Introduction
The adoption of 3D printing technology in dentistry has revolutionised clinical workflows, offering unprecedented precision and efficiency in the creation of dental restorations, surgical templates, and orthodontic appliances. Its advantages include enhanced customisation, reduced production times, cost efficiency, and improved patient outcomes facilitated by computer-aided design systems. Among the various 3D printing technologies available, resin-based methods, including stereolithography and digital light processing, are widely employed in dental clinics due to their superior precision and material adaptability.
Despite its transformative potential, resin-based 3D printing introduces significant occupational and environmental health risks. During the printing process, harmful emissions such as volatile organic compounds and ultrafine particles are released, which can degrade indoor air quality and pose serious health risks to dental professionals. These emissions have been linked to respiratory issues, skin irritation, and other health concerns, making them a critical focus for improving workplace safety in dental clinics.
Although the clinical benefits of 3D printing are well-documented in the literature, the health risks associated with these emissions remain underexplored. This literature review aims to address this gap by evaluating the types and concentrations of emissions, their impact on indoor air quality, and their associated health implications. Furthermore, the review identifies effective mitigation strategies, including advanced ventilation systems, air filtration technologies, and safe material handling practices, to provide practical recommendations for minimising these risks.
By focusing on the dual themes of airborne chemical emissions and mitigation strategies, this review seeks to guide dental professionals towards safer and more sustainable adoption of resin-based 3D printing, ensuring the health and safety of both practitioners and patients as digital dentistry continues to evolve.
2. Airborne Chemical Emissions in the Course of Resin-Based 3D Printing
2.1 Volatile Organic Compounds (VOCs)
One of the significant concerns associated with resin-based 3D printing is the emission of volatile organic compounds (VOCs). These emissions occur during the photopolymerisation process when liquid resin is exposed to ultraviolet (UV) light. Common VOCs released from dental resins include methacrylate, styrene, and isocyanates, which are known to cause respiratory irritation, skin sensitisation, and, with prolonged exposure, may have carcinogenic effects. A study noted that many dental practitioners in Saudi Arabia lack awareness of the VOC emissions associated with 3D printing, indicating a knowledge and safety practice deficit.
The levels of VOC emissions are influenced by various factors, including the type of resin and printer, the duration of the printing process, and environmental conditions. Additionally, research has shown that the colour and translucency of dental materials used in 3D printing can impact VOC emissions, with certain materials releasing higher levels of VOCs when exposed to UV light for extended periods. Viitanen et al. demonstrated that the emission profiles of lattices used in tissue engineering can vary depending on the density and design of the printed object.
2.2 Particulate Matter (PM) and Ultrafine Particles (UFPs)
Another critical issue involves the release of particulate matter (PM) and ultrafine particles (UFPs) during resin-based 3D printing. These particles, typically less than 100 nanometres in size, can penetrate deep into the respiratory system, potentially leading to severe health implications. Research indicates that environments utilising resin-based 3D printers exhibit higher concentrations of UFPs compared to other indoor environments, particularly when acrylate-based resins are used.
Several studies have assessed the emissions from different 3D printing processes, noting that the evels of particulate emissions vary depending on the workflow. Adjusting print settings and selecting appropriate resins have been shown to reduce emissions. In their analysis of metal 3D printing for dental prostheses, Kangas et al. observed that different printing technologies produce varying levels of UFPs. They recommended the use of resin formulations with lower particle release, particularly in healthcare settings where both workers and patients are directly exposed to the emissions.

3. Effects on the Quality of Indoor Air and Health Risk Assessment
Volatile organic compounds (VOCs) and ultrafine particles (UFPs) can accumulate in dental clinics, significantly affecting indoor air quality. Prolonged exposure to these emissions can lead to long-term respiratory and cardiovascular illnesses among dental professionals and patients. Jeong et al. compared the reliability of dental models produced through different techniques, including CAD/CAM milling and 3D printing, and noted that environments using 3D printing displayed elevated concentrations of airborne pollutants, posing potential health risks.The health impacts associated with exposure to these emissions have been explored in multiple studies, which highlight the need for safer materials in 3D printing. Specifically, reviews on 3D-printable materials for intraoral orthodontic applications emphasise the importance of selecting materials with lower emission levels. Furthermore, Voet et al. reviewed the use of 3D printing in oral soft tissue engineering and stressed the importance of addressing the environmental consequences of 3D printing processes to protect both patients and the broader environment.
4. Measures which have been put in place in order to minimise the risks that are associated with the identified hazards.
4.1 Enhanced Ventilation Systems
The concentration of airborne contaminants, such as volatile organic compounds and ultrafine particles, in indoor environments can be effectively managed through improved ventilation. Research highlights that well-designed ventilation systems can significantly reduce the levels of these pollutants in dental clinics. Chýlek et al. demonstrated that the integration of high-efficiency particulate air (HEPA) filtration within ventilation systems is a particularly effective method for minimising emissions in clinics utilising resin-based 3D printers.
Furthermore, Rogers et al. emphasised the importance of adhering to established guidelines for room air exchange rates and recommended the installation of local exhaust ventilation (LEV) systems to capture emissions at their source. The incorporation of real-time monitoring sensors into ventilation systems could further enhance safety by providing staff with immediate feedback on elevated pollutant concentrations, allowing for timely interventions.
4.2 Air Filtration Technologies
The use of air filtration technologies, such as HEPA filters and activated carbon filters, has been identified as an effective means of reducing both volatile organic compounds and ultrafine particles in dental facilities. Chiu and Chen highlighted that these filters, when used in air purifiers, can help maintain safer indoor air quality, ensuring a healthier working environment for dental professionals.
4.3 Safety Measures in Handling and Disposing of the Chemicals
Proper handling and disposal of 3D printing materials play a crucial role in mitigating emissions of volatile organic compounds and ultrafine particles. Jeong et al. advocated for comprehensive training for dental personnel on the safe handling of resins, the necessity of personal protective equipment (PPE), and the appropriate conditions for storing these materials. Compliance with local and international guidelines for the disposal of hazardous materials can further reduce environmental pollution and minimise occupational exposure risks.
4.4 Material Selection and Process Optimisation
Choosing low-emission resins and optimising the printing process are critical strategies for reducing emissions. The use of biocompatible, low-odour photopolymers has been shown to release fewer hazardous volatile substances. Spagnuolo et al. stressed that selecting the right materials for dental applications can significantly decrease both volatile organic compound and particulate emissions. Additionally, Shinkai et al. demonstrated that improvements in resin composition and adjustments to printing parameters, such as curing time and temperature, can lead to safer and more efficient solutions.
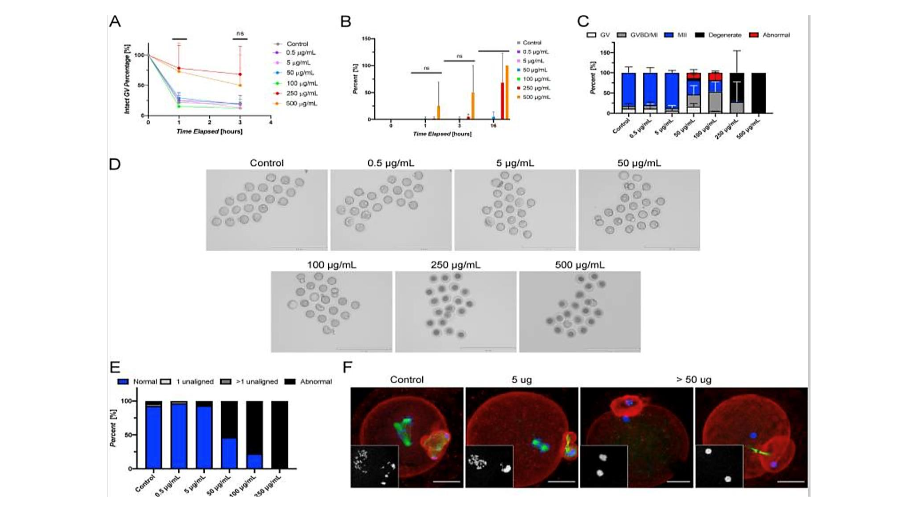
Figure 2 – Tinuvin 292 induces abnormal meiotic phenotypes and oocyte degeneration in a dose-responsive manner in vitro. [29]
5. Future research and development required
Advancements in 3D printing technology have significantly enhanced creativity, customisation, and precision in dental practice. However, the associated health impacts, such as airborne particle emissions, reproductive toxicity from leachates, and environmental concerns, necessitate the development of safer and more sustainable practices. Future research and development efforts should focus on the following areas:
5.1 Development of Environmentally Sensitive and Low Volatile Organic Emission Resins
Addressing the toxicological risks posed by existing dental resins, including their emissions of volatile organic compounds and potential for reproductive toxicity, requires the creation of safer formulations. Realising the full potential of resin-based 3D printing in dentistry depends on the development of materials that emit fewer volatile organic compounds while maintaining essential mechanical properties and precision. Future materials should utilise less harmful additives, such as reduced quantities of photoinitiators and the exclusion of reproductive toxicants like Tinuvin 292.Innovative approaches could include biopolymer-based resins or nano-composites reinforced with natural or synthetic elements to improve safety and environmental compatibility. Biocompatible solutions, such as resins with zirconia or glass silica micro-fillers, have shown promise in minimising risks associated with conventional resin-based materials. Realising these advancements requires interdisciplinary collaboration among materials scientists, toxicologists, and dental researchers to ensure performance and compliance with environmental standards.
5.2 Improving Ventilation and Air Filtration Systems
Improving indoor air quality in dental clinics remains crucial to reducing emissions from resin-based 3D printing. Current ventilation and filtration systems in healthcare settings may be inadequate for controlling volatile organic compounds and particulate matter. Future efforts should focus on designing highly efficient HVAC systems tailored to the unique chemical outputs of dental 3D printing.Activated carbon filters and HEPA filters should be optimised to capture volatile organic compounds and nano-sized particles effectively. Furthermore, integrating ultraviolet sterilisation and photocatalytic oxidation systems may enhance air purification, removing airborne chemicals and pathogens and reducing exposure risks for dental personnel.
5.3 Digital Monitoring Tools for Real-Time Emission Tracking
Digital tools and automated systems for real-time monitoring of emissions are vital for maintaining safe indoor air quality in dental clinics. Sensors capable of detecting volatile organic compounds, particulate matter, and other pollutants can provide immediate feedback on air quality. This data could be used to dynamically control ventilation and filtration systems, ensuring optimal air quality throughout the clinic.
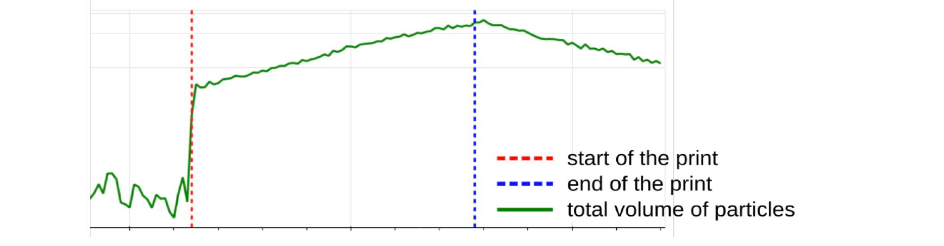
Integrating these systems with the Internet of Things (IoT) would enable smart environments that initiate air purification processes when emission thresholds are exceeded. Additionally, machine learning algorithms could predict high-emission events, allowing clinics to take preemptive measures to safeguard dental professionals.
5.4 The Use of Sustainable 3D Printing Practices
Sustainability in 3D printing workflows is increasingly important as digital dentistry grows. Strategies such as closed-loop recycling systems, which capture and reuse waste resin materials, can reduce environmental impact. Similarly, energy-efficient printers and optimised printing workflows that minimise production time while maintaining precision can significantly lower the carbon footprint of digital dentistry.Collaboration among dentists, researchers, and industry stakeholders is necessary to establish guidelines for sustainable practices in 3D printing, encompassing manufacturing, application, disposal, and recycling. These efforts would promote environmentally responsible digital workflows in dentistry.
5.5 More General Consequences for Occupational Safety in Digital Dentistry
In addition to addressing emissions and material safety, future research should consider the broader occupational hazards associated with digital dentistry. These include the ergonomic challenges posed by prolonged use of 3D printing technologies and the human-machine interface. Examining the effects of low-level emissions and the impact of working in digitally enhanced environments can provide a more comprehensive understanding of occupational risks in modern dental practice.
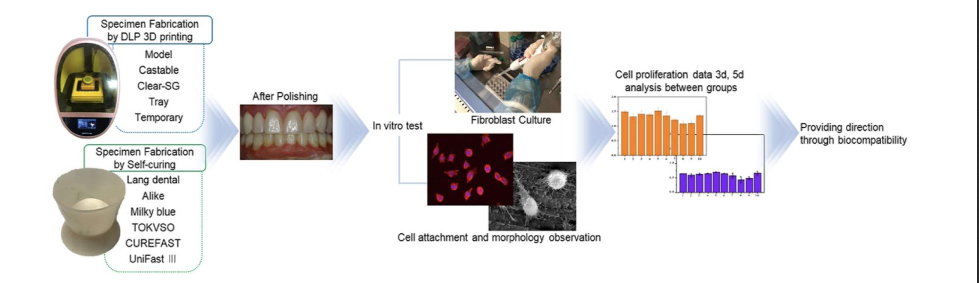
Figure 4 – Dental fabrication process of temporary restorations by DLP 3D printing and Self-curing method cytocompatibility of the fibroblast cell.
In addition to addressing emissions and material safety, future research should consider the broader occupational hazards associated with digital dentistry. These include the ergonomic challenges posed by prolonged use of 3D printing technologies and the human-machine interface. Examining the effects of low-level emissions and the impact of working in digitally enhanced environments can provide a more comprehensive understanding of occupational risks in modern dental practice.
5.6 Lifelong Learning in Dental Professionals
Ongoing education and training are critical for ensuring safety in digital dentistry. Encouraging dental professionals to adopt preventive measures will empower them to make informed decisions about handling 3D printing materials, using appropriate personal protective equipment, and understanding the risks of chemical exposure. Training programmes focused on best practices for operating and maintaining 3D printing equipment
6. Conclusion
Resin-based 3D printing has revolutionised digital dentistry, offering numerous benefits such as precision, customisation, and efficiency. However, its adoption is not without challenges, particularly in terms of emissions of volatile organic compounds and ultra-fine particles, which pose risks to both workers and the environment.This review underscores the importance of recognising these risks and implementing measures to mitigate them. Key strategies include improving ventilation, employing high-efficiency filtration systems, and adhering to safe practices for handling and disposing of materials. By adopting these measures, dental clinics can create safer, healthier, and more environmentally sustainable workplaces, ensuring that the digital transformation of the dental industry progresses responsibly and ethically.Author Contributions: Conceptualisation, writing—original draft preparation, writing—review and editing, visualisation, A.B. Nulty. The author has read and agreed to the published version of the manuscript.
Conflicts of Interest:
The author declares no conflicts of interest.Funding:
This research received no external funding.Institutional Review Board Statement:
Not applicable.Use of Artificial Intelligence:
AI or AI-assisted tools were not used in drafting any aspect of this manuscript.References
1. Suganna M, Kausher H, Rownaq Ali ABM, Abed MM, Albishi WS, Al Hajji FA, Sultan NA. Knowledge on Applications of 3D Design and Printing in Dentistry Among Dental Practitioners in Saudi Arabia: A Questionnaire-Based Survey. Cureus. 2022 Aug 25;14(8):e28379. doi: 10.7759/cureus.28 379. PMID: 36171830; PMCID: PMC9508789.
2. Nulty A. A comparison of trueness and precision of 12 3D printers used in dentistry. BDJ Open. 2022 May 26;8(1):14. doi: 10.1038/s41405-022-00108-6. PMID: 35618716; PMCID: PMC9135 705.
3. Yu X, Li G, Zheng Y, Gao J, Fu Y, Wang Q, Huang L, Pan X, Ding J. ‘Invisible’ orthodontics by polymeric ‘clear’ aligners molded on 3D-printed personalized dental models. Regen Biomater. 2022 Feb 4;9(1):rbac007. doi: 10.1093/rb/rbac007. PMID: 35414958; PMCID: PMC8992363.
4. Marturello DM, Déjardin LM. Post-sterilization Dimensional Accuracy of Methacrylate Monomer Biocompatible Three-Dimensionally Printed Mock Surgical Guides. Vet Comp Orthop Traumatol. 2023 Nov;36(6):279-286. doi: 10.1055/s-0043-1768991. Epub 2023 Jun 16. PMID: 37327880.
5. Prpić V, Schauperl Z, Ćatić A, Dulčić N, Čimić S. Comparison of Mechanical Properties of 3D-Printed, CAD/CAM, and Conventional Denture Base Materials. J Prosthodont. 2020 Jul;29(6):524-528. doi: 10.1111/jopr.13175. Epub 2020 Apr 20. PMID: 32270904.
6. Steinle P. Characterization of emissions from a desktop 3D printer and indoor air measurements in office settings. J Occup Environ Hyg. 2016;13 (2):121-32. doi: 10.1080/15459624.2015.1091957. PMID: 26550911.
7. Pham YL, Wojnowski W, Beauchamp J. Volatile Compound Emissions from Stereolithography Three-Dimensional Printed Cured Resin Models for Biomedical Applications. Chem Res Toxicol. 2023 Mar 20;36(3):369-379. doi: 10.1021/acs.chemresto x.2c00317. Epub 2022 Dec 19. PMID: 36534374.
8. Wallach R, English JD, Moon A, Brock RA 2nd, Paravina RD, Kasper FK. Colour stability of 3D-Printed orthodontic brackets using filled resins. Orthod Craniofac Res. 2023 Dec;26 Suppl 1:180-187. doi: 10.1111/ocr.12665. Epub 2023 Apr 23. PMID: 37089069.
9. Egan PF, Gonella VC, Engensperger M, Ferguson SJ, Shea K. Computationally designed lattices with tuned properties for tissue engineering using 3D printing. PLoS One. 2017 Aug 10;12(8): e0182902. doi: 10.1371/journal.pone.0182902. PMID: 28797066; PMCID: PMC5552288.
10. Alenezi A, Yehya M. Evaluating the Accuracy of Dental Restorations Manufactured by Two CAD/CAM Milling Systems and Their Prototypes Fabricated by 3D Printing Methods: An In Vitro Study. Int J Prosthodont. 2023 May-June;36(3):293-300. doi: 10.11607/ijp.7633. PMID: 34919097.
11. Nulty A, Lefkaditis C, Zachrisson P, Van Tonder Q, Yar R. A clinical study measuring dental aerosols with and without a high-volume extraction device. Br Dent J. 2020 Nov 20:1–8. doi: 10.103 8/s41415-020-2274-3. Epub ahead of print. PMID: 33184481; PMCID: PMC7658616.
12. Goracci C, Juloski J, D’Amico C, Balestra D, Volpe A, Juloski J, Vichi A. Clinically Relevant Properties of 3D Printable Materials for Intraoral Use in Orthodontics: A Critical Review of the Literature. Materials (Basel). 2023 Mar 8;16(6):2166. doi: 10.3390/ma16062166. PMID: 36984045; PMCID: PMC10058724.
13. Do AV, Khorsand B, Geary SM, Salem AK. 3D Printing of Scaffolds for Tissue Regeneration Applications. Adv Healthc Mater. 2015 Aug 26;4 (12):1742-62. doi: 10.1002/adhm.201500168. Epub 2015 Jun 10. PMID: 26097108; PMCID: PMC4597 933.
14. Katakam P, Bhavaraju MLR, Narayana TV, Bhandari K, Sriram N, Sisinty VS, Adiki SK. Navigating the Challenges of 3D Printing Personalized Medicine in Space Explorations: A Comprehensive Review. Crit Rev Ther Drug Carrier Syst. 2024;41(6):89-110. doi: 10.1615/CritRevTherDrugCarrierSyst.2024051126. PMID: 38804555.
15. Viitanen AK, Kallonen K, Kukko K, Kanerva T, Saukko E, Hussein T, Hämeri K, Säämänen A. Technical control of nanoparticle emissions from desktop 3D printing. Indoor Air. 2021 Jul;31(4): 1061-1071. doi: 10.1111/ina.12791. Epub 2021 Mar 1. PMID: 33647162.
16. Arif ZU, Khalid MY, Noroozi R, Sadeghianmaryan A, Jalalvand M, Hossain M. Recent advances in 3D-printed polylactide and polycaprolactone-based biomaterials for tissue engineering applications. Int J Biol Macromol. 2022 Oct 1;218:930-968. doi: 10.1016/j.ijbioma c.2022.07.140. Epub 2022 Jul 24. PMID: 35896130.
17. Väisänen A, Alonen L, Ylönen S, Hyttinen M. Organic compound and particle emissions of additive manufacturing with photopolymer resins and chemical outgassing of manufactured resin products. J Toxicol Environ Health A. 2022 Mar 4;85(5):198-216. doi: 10.1080/15287394.2021.199 8814. Epub 2021 Nov 11. PMID: 34763622.
18. Farcas MT, McKinney W, Qi C, Mandler KW, Battelli L, Friend SA, Stefaniak AB, Jackson M, Orandle M, Winn A, Kashon M, LeBouf RF, Russ KA, Hammond DR, Burns D, Ranpara A, Thomas TA, Matheson J, Qian Y. Pulmonary and systemic toxicity in rats following inhalation exposure of 3-D printer emissions from acrylonitrile butadiene styrene (ABS) filament. Inhal Toxicol. 2020 Sep-Oct;32(11-12):403-418. doi: 10.1080/08958378.2020.1834034. Epub 2020 Oct 20. PMID: 33076715; PMCID: PMC7673646.
19. Shuaib et al, Impact of 3D Printing on the environment: A literature-based study, Sustainable Operations and Computers, Volume 2, 2021, Pages 57-63, ISSN 2666-4127, https://doi.org/10.1016/j.susoc.2021.04.001.
20. Shujaat S, Bornstein MM, Price JB, Jacobs R. Integration of imaging modalities in digital dental workflows – possibilities, limitations, and potential future developments. Dentomaxillofac Radiol. 2021 Oct 1;50(7):20210268. doi: 10.1259/dmfr.20210268. Epub 2021 Sep 14. PMID: 34520239; PMCID: PMC8474138.
21. Kangas A, Kukko K, Kanerva T, Säämänen A, Akmal JS, Partanen J, Viitanen AK. Workplace Exposure Measurements of Emission from Industrial 3D Printing. Ann Work Expo Health. 2023 Jun 6;67(5):596-608. doi: 10.1093/annweh/wxad006. PMID: 36869756; PMCID: PMC10243937.
22. Tian Y, Chen C, Xu X, Wang J, Hou X, Li K, Lu X, Shi H, Lee ES, Jiang HB. A Review of 3D Printing in Dentistry: Technologies, Affecting Factors, and Applications. Scanning. 2021 Jul 17;2021:99 50131. doi: 10.1155/2021/9950131. PMID: 3436 7410; PMCID: PMC8313360.
23. Liu MH, Chen CT, Chuang LC, Lin WM, Wan GH. Removal efficiency of central vacuum system and protective masks to suspended particles from dental treatment. PLoS One. 2019 Nov 26;14(11): e0225644. doi: 10.1371/journal.pone.0225644. PMID: 31770413; PMCID: PMC6879156.
24. Park JH, Lee H, Kim JW, Kim JH. Cytocompatibility of 3D printed dental materials for temporary restorations on fibroblasts. BMC Oral Health. 2020 Jun 1;20(1):157. doi: 10.1186/ s12903-020-01150-2. PMID: 32487153; PMCID: PMC7268758.
25. Jeong M, Radomski K, Lopez D, Liu JT, Lee JD, Lee SJ. Materials and Applications of 3D Printing Technology in Dentistry: An Overview. Dent J (Basel). 2023 Dec 19;12(1):1. doi: 10.3390/ dj12010001. PMID: 38275676; PMCID: PMC108 14684.
26. Voet VSD, Guit J, Loos K. Sustainable Photopolymers in 3D Printing: A Review on Biobased, Biodegradable, and Recyclable Alternatives. Macromol Rapid Commun. 2021 Feb;42(3):e200 0475. doi: 10.1002/marc.202000475. Epub 2020 Nov 18. PMID: 33205556.
27. Nadagouda MN, Ginn M, Rastogi V. A review of 3D printing techniques for environmental applications. Curr Opin Chem Eng. 2020;28:173-178. doi: 10.1016/j.coche.2020.08.002. PMID: 343 27115; PMCID: PMC8318092.
28. Chýlek R, Kudela L, Pospíšil J, Šnajdárek L. Parameters Influencing the Emission of Ultrafine Particles during 3D Printing. Int J Environ Res Public Health. 2021 Nov 6;18(21):11670. doi: 10.3390/ijer ph182111670. PMID: 34770184; PMCID: PMC858 2798.
29. Rogers HB, Zhou LT, Kusuhara A, Zaniker E, Shafaie S, Owen BC, Duncan FE, Woodruff TK. Dental resins used in 3D printing technologies release ovo-toxic leachates. Chemosphere. 2021 May;270: 129003. doi: 10.1016/j.chemosphere.2020.129003. Epub 2020 Dec 7. PMID: 33515896; PMCID: PMC7957323.
30. Taştan, M.; Gökozan, H. Real-Time Monitoring of Indoor Air Quality with Internet of Things-Based E-Nose. Appl. Sci. 2019, 9, 3435. https://doi.org/10.3390/app9163435
31. Tian Y, Chen C, Xu X, Wang J, Hou X, Li K, Lu X, Shi H, Lee ES, Jiang HB. A Review of 3D Printing in Dentistry: Technologies, Affecting Factors, and Applications. Scanning. 2021 Jul 17;2021:9950131. doi: 10.1155/2021/9950131. PMID: 34367410; PMCID: PMC8313360.
32. Spagnuolo G, Sorrentino R. The Role of Digital Devices in Dentistry: Clinical Trends and Scientific Evidences. J Clin Med. 2020 Jun 2;9(6):1692. doi: 10.3390/jcm9061692. PMID: 32498277; PMCID: PMC7356564.
33. Shinkai RSA, Biazevic MGH, Michel-Crosato E, de Campos TT. Environmental sustainability related to dental materials and procedures in prosthodontics: A critical review. J Prosthet Dent. 2023 Sep 12:S0022-3913(23)00370-0. doi: 10.1016 /j.prosdent.2023.05.024. Epub ahead of print. PMID: 37709614.
34. Author 1, A.B. Title of Thesis. Level of Thesis, Degree-Granting University, Location of University, Date of Completion.
35. Title of Site. Available online: URL (accessed on Day Month Year).

