Balancing Drug Efficacy and Safety in Polypharmacy
What Comes First to Your Mind: Drug Efficacy or Drug Safety?
Veronique Michaud, B.Pharm., PhD., 1 Mark Munger, PharmD, 2 and Jacques Turgeon, B.Pharm., PhD 3
- President and co-founder, GalenusRx Inc, Montverde, Florida, USA Adjunct Professor, Faculty of Pharmacy, Université de Montréal, Quebec, Canada Associate researcher, Centre de Recherche du Centre Hospitalier de l’Université de Montréal, Montreal, Quebec, Canada
- Professor, Pharmacotherapy and Adjunct Professor, Internal Medicine Salt Lake City, University of Utah, Utah, USA Fellow, American College of Cardiology Fellow, Heart Failure Society of America
- Chief Executive Officer and co-Founder, GalenusrRx Inc, Montverde, Florida, USA; Professor Emeritus, Université de Montréal; Fellow, Canadian Academy of Sciences; Fellow, Académie nationale de médecine, France
OPEN ACCESS
PUBLISHED: 31 May 2025
CITATION: Michaud, V., Munger, M., et al., 2025. What Comes First to Your Mind: Drug Efficacy or Drug Safety? Medical Research Archives, [online] 13(5). https://doi.org/10.18103/mra.v13i5.6551
COPYRIGHT: © 2025 European Society of Medicine. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
DOI https://doi.org/10.18103/mra.v13i5.6551
ISSN 2375-1924
ABSTRACT
Disease-treatment guidelines are most often implemented clinically as part of comprehensive medication management to ensure patients receive the most effective and evidence-based care. Post-marketing pharmacovigilance programs are the main source of medication safety monitoring. However, pharmacovigilance programs have multiple problems including underreporting of adverse drug events (ADEs), inconsistent reporting standards, and difficulties in data analysis and interpretation making it difficult to examine safety information. Patients with multiple chronic diseases leading to polypharmacy are at an increased risk of ADEs. There are various elements that constitute a successful approach while balancing efficacy and safety including: 1) Medication-related problems and ADE risk identification, prevention, and management; 2) Interdisciplinary collaboration; 3) Beneficiary-centered personalized care; 4) Technology integration; 5) Outcome evaluation and quality improvement; and 6) Pre-emptive pharmacovigilance studies by the virtual addition of drugs to patients’ drug regimen. In conclusion, medications generally enter the market with proven efficacy but often lack short- and long-term safety information. A personalized transformative approach leveraging innovative clinical science-based technology and medication safety experience can create a more effective, patient-centered approach to managing complex medication regimens, ultimately improving patient safety and outcomes.
Keywords
Drug efficacy, Drug safety, Pharmacovigilance, Polypharmacy, Medication management
Main text
We believe in a paradigm shift from promoting drug adherence to achieve efficacy to promoting adherence to a safe drug regimen: What if we make sure that the entire drug regimen of patients with polypharmacy is safe, appropriate and that there are no conditions predisposing to adverse drug events (ADEs) that could be prevented, before patient drug administration.
The path of medications under development by the pharmaceutical industry, particularly in clinical phases (Phases I-IV), is focused on efficacy as required by regulatory bodies. In the absence of evidence of substantial benefits (efficacy) towards a targeted condition or untoward adverse effects, the development of the potential medication is ended and the search for another lead compound is launched.
Clinical trials fuel evidence-based medicine, marketing strategies to health care providers and direct-to-consumer information (in the United States of America), that all play a significant role in promoting the benefits of drugs and drug combinations for specific conditions. Post-marketing, comprehensive medication management is focused on the implementation of disease-treatment guidelines published by scientific communities, clinical experts or healthcare organizations to ensure patients receive the most effective and evidence-based care.
The missing link of data from most clinical trials is our lack of understanding of drug safety in multi-drug regimens, or polypharmacy, in patients with multiple chronic diseases as those “real-world patients” are often excluded from clinical trials and are not required for drug regulatory approval. Thereby new drug approval pharmacovigilance programs become a main source for monitoring medication safety post-marketing.
Pharmacovigilance programs have multiple problems including underreporting of ADEs, inconsistent reporting standards, and difficulties in data analysis and interpretation making it difficult to examine safety information. ADEs stem from a variety of factors including drug interactions, inappropriate prescribing, medication administration issues, and individual factors. ADEs are a significant healthcare problem, contributing to morbidity and mortality, increased healthcare costs, and reduced quality of life. ADEs lead to increased healthcare services utilization, including hospitalizations, emergency department visits, additional medical appointments, medication-related interventions, indirect costs, productivity losses due to missed workdays, caregiver burden, diminished quality of life for individuals and their families, physical discomfort, psychological distress, functional impairment, and decreased adherence to treatment regimen. The economic and personal burden of ADEs underscores the importance of comprehensive safety medication management to minimize these risks.
In contrast, managing ADEs, especially when polypharmacy is present requires a more scientific-based approach. When individuals take multiple medications, it can be incredibly complex and the ability to understand pharmacokinetics, pharmacodynamics and pharmacogenomic interactions remain beyond reach of most app-based programs. A more centralized approach to appropriate medication safety management is crucial for effectively managing all the medications these patients receive, including deprescribing and ensuring patient safety. Medication management can improve patients’ outcomes, reduce healthcare costs, enhance the quality of care, and reduce ADEs by optimizing the safety and efficiency of medication use and addressing any potential issues or concerns.
There are various elements that could constitute a successful approach while balancing efficacy and safety:
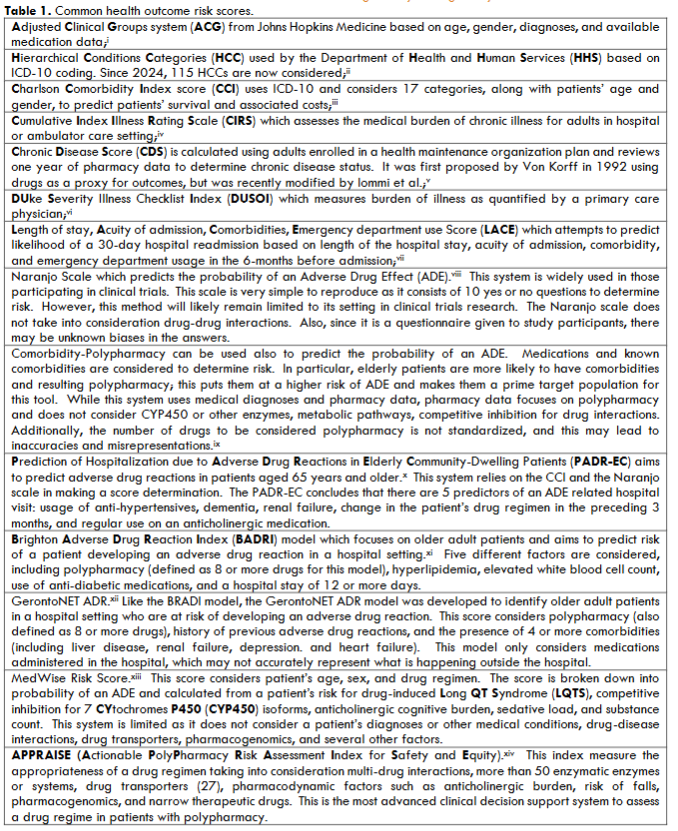
- Medication-related problems and ADE risk identification, prevention, and management. Several risk scales have been developed over the years to predict or assess various patients’ clinical outcomes. A non-exhaustive list is presented in Table 1. From this list, 9 risk scoring systems consider, to some extent, the presence of medications to predict various patients’ outcomes. These include ACG, CDS, the Naranjo scale, Comorbidity-Polypharmacy, PADR-EC, BADRI, GerontoNET, MedWise Risk Score and APPRAISE™. APPRAISE solution fulfills the comprehensive list of elements envisioned almost 10 years ago as constituting the ideal advanced clinical decision support system. Patient-centric-based practices implemented to prevent and manage medication-related problems and ADEs, including robust medication reconciliation protocols, personalized medication therapy management services, and education initiatives mitigate risks and ensure optimal medication use.
- Interdisciplinary Collaboration: A successful approach emphasizes collaboration among organizations, healthcare prescribers, pharmacists, and other stakeholders to coordinate care and enhance medication safety. The aim is to streamline medication management processes, care coordination, and improve beneficiary outcomes by fostering interdisciplinary communication and teamwork. Further, local community pharmacists’ engagement with patients when they present medication fills and refills is central to optimal medication use. However, adoption of telepharmacy practice can bridge this engagement gap and play a crucial role in improving patient health outcomes.
- Beneficiary-Centered Personalized Care: A focus on personalized patient-centered care should be part of a successful approach. Leveraging pharmacogenomic testing and genotyping which are powerful tools can help personalize complex medication regimens. Empowering patients to take an active role in their treatment plans and medication management is also important and can lead to better health outcomes and increased satisfaction. Patient education, counseling, and engagement initiatives help promote medication adherence and foster ownership over health decisions. Advanced training in pharmacogenomics and the use of solutions considering factors like phenoconversion and individualized patient conditions are key for making appropriate medication recommendations.
4. Technology Integration: Leveraging healthcare technologies like electronic health records (EHRs) and clinical decision support systems (CDSS) is key to enhance medication safety through real-time alerts, medication reconciliation tools, and data-driven actionable insights. By harnessing the power of innovative technology and science with the proper tool that considers the entire drug regimen, not only using the antiquated one-drug-to-one-drug drug interaction systems, the integration of such tool can also more effectively identify and prevent medication-related problems and ADEs.
5. Outcome Evaluation and Quality Improvement: Continuous monitoring and evaluation of interventions is essential for measuring impact and driving quality improvement. Performance metrics should be implemented, conducting regular assessments and refining strategies based on feedback and results to ensure ongoing effectiveness. This requires proper documentation and coding such as more elaborated SNOMED (Systematized NOmenclature for MEDicines) codes for clinical pharmacy services.
6. Pre-emptive pharmacovigilance studies by the virtual addition of drugs to patients’ drug regimen. Database rich real-world data for millions of individuals can be used to simulate the impact of adding a drug to the drug regimen of patients with various patient characteristics. To assess the risk of ADEs, a fictitious claim for the tested drug (or drug combination) could be added to the actual drug regimen for each subject. Following the addition of a drug, a new medication safety score could be derived for each individual. These quasi-mechanistic approaches allow for the prospective estimation of risk, without exposing patients to drugs and side effects. Quantitative analyses can be conducted for sub-populations of patients which can provide valuable insights into specific conditions that increase risk.
Science-driven, precision risk targeting and medication risk reduction and optimization encompasses many of the core tenets of standard medication management, appropriate medication usage, improved adherence, and overall enhancement of patient well-being. Advanced medication safety needs to provide medication reconciliation, personalized medication reviews, patient education, outcome monitoring, and seamless care coordination among healthcare providers. By optimizing medication use and addressing potential ADE and medication-related concerns, clinicians can improve patients’ outcomes, reduce healthcare costs, and elevate the quality of care.
In conclusion, medications generally enter the market and our pharmacological armamentarium with proven efficacy but often lack short- and long-term safety information. A transformative approach to medication risk reduction leveraging deep innovative clinical science, technology and medication safety experience is essential, especially in patients dealing with polypharmacy. Combining strategies can create a more effective and patient-centered approach to managing complex medication regimens, ultimately improving patient safety and outcomes.
References
- https://crib.pharmacy.purdue.edu/research/how-many-fda-approved-drugs-have-been-withdrawn-and-why-are-aspiring-drugs-abandoned
- “Pharmaceuticals: The Good and the Bad.” Nationalacademies.org/hmd/-Informing the Future: Critical Issue in Health. Fourth Edition. Institutes of Medicine. National Academy of Sciences. 2007. Pp.13-17. Accessed 03/21/2025
- Ciapponi A, Fernandez Nievas SE, Seijo M, Rodríguez MB, Vietto V, García-Perdomo HA, Virgilio S, Fajreldines AV, Tost J, Rose CJ, Garcia-Elorrio E. Reducing medication errors for adults in hospital settings. Cochrane Database Syst Rev. 2021 Nov 25;11(11):CD009985. doi: 10.1002/14651858.CD009985.pub2.
- Martin F, Susan SM. Improving the external validity of clinical trials: the case of multiple chronic conditions. J Comorbidity. 2013 Dec 24;3(Spec Issue):30–5.
- Endale Biru S, Wallelign TM, Gedif Fenta T. Implementation Status and Challenges of Pharmacovigilance Program in Ethiopia: A Mixed-Methods Study. Inquiry. 2024 Oct 7;61:00469580241287752
- Louis Palatty P, Sacheendran D, Jayachandran M (2024) Mitigating Challenges in Pharmacovigilance. Pharmacovigilance – Facts, Challenges, Limitations and Opportunity [Working Title]. IntechOpen. Available at: http://dx.doi.org/10.5772/intechopen.1005978.
- Turgeon J, Munger MA. Guest Column: FAIL SAFE. Changing a broken approach to medication safety. Drug Store News 2022 July 20. https://issuu.com/ensembleiq/docs/dsn-0722?fr=sYjJkOTgwODQ2MQ.
- Munger MA, Turgeon J, Pace W. Op-Ed: Why we need a modern act to prevent harm from medications. The Hill 2022
- Kommu A, Carter C, Whitfield P. Adverse Drug Reactions. StatPearls January 10, 2024. https://www.ncbi.nlm.nih.gov/books/NBK599521/#:~:text=%5B1%5D%20Additionally%2C%20in%20the%20efforts%20to%20prevent%20their%20occurrence.
- Turgeon J, Michaud V. Clinical decision support systems: great promises for better management of patients’ drug therapy. Expert Opin Drug Metab Toxicil 2016;12(9):993-995. doi.org/10.1517/17425255.2016.1171317
- Bankes D, Pizzolato K, Finnel S, Awadalla MS, Stein A, Johnson J, Turgeon J. Medication-related problems identified by pharmacist in an enhanced medication therapy model. Am J Manag Care 2021;27:S292-S299
- Stein A, Finnel S, Bankes D, Jin H, Awadalla MS, Johnson J, turgeon J. Health outcomes from an innovative enhanced medication therapy management model. AM J Manag Care 2021;27:S300-S308.
Table 1 References
- https://www.johnshopkinssolutions.com/wp-content/uploads/2016/08/ACG-System-Brochure.pdf.
- https://insideangle.3m.com/his/blog-post/risk-adjustment-a-look-at-version-28-2024/#:~:text=Several%20changes%20to%20the%202024%20risk%20adjustment%20model,blood%2C%20ampuation%2C%20neurological%2C%20diabetes%2C%20kidney%2C%20psychiatric%20and%20musculoskeletal.
- https://www.mdcalc.com/calc/3917/charlson-comorbidity-index-cci
- Salvi, F.; Miller, M.D.; Grilli, A.; Giorgi, R.; Towers, A.L.; Morichi, V.; Spazzafumo, L.; Mancinelli, L.; Espinosa, E.; Rappelli, A.; et al. A Manual of Guidelines to Score the Modified Cumulative Illness Rating Scale and Its Validation in Acute Hospitalized Elderly Patients. J. Am. Geriatr. Soc. 2008, 56, 1926–1931
- https://journals.plos.org/plosone/article/file?id=10.1371/journal.pone.0240899&type=printable
- https://link.springer.com/referenceworkentry/10.1007/978-94-007-0753-5_3510
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9024499/pdf/jpm-12-00545.pdf
- Naranjo CA, Busto U, Sellers EM, Sandor P, Ruiz I, Roberts EA, Janecek E, et al. A method for estimating the probability of adverse drug reactions. Clin Pharmacol Ther. 1981;30:239–45
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5087856/pdf/pone.0165757.pdf
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4214735/pdf/pone.0111254.pdf
- file:///C:/Users/JacquesTurgeon/Downloads/s40266-016-0428-4.pdf
- https://www.galenusrx.com

