BNP Levels and Survival in Major Limb Amputation Patients
Brain natriuretic peptide is associated with survival in persons with dysvascular major lower limb amputation
Elebarta J.E. Heida- de Hoop, MD1, Klaske van Kammen, PhD1, Pieter U. Dijkstra, PhD1,2, Jan H.B. Geertzen, MD, PhD1
- University of Groningen, University Medical Center Groningen, Department of Rehabilitation Medicine, Groningen, the Netherlands.
- University of Groningen, University Medical Center Groningen, Department of Rehabilitation Medicine, Groningen, the Netherlands; Sirindhorn School of Prosthetics and Orthotics, Faculty of Medicine Siriraj Hospital, Mahidol University 14 Arunamarin Road, Bangkoknoi, Bangkok, 10700, Thailand.
OPEN ACCESS
PUBLISHED: 30 November 2025
CITATION: HEIDA- DE HOOP, Elebarta J.E. et al. Brain natriuretic peptide is associated with survival in persons with dysvascular major lower limb amputation. Medical Research Archives,. Available at: <https://esmed.org/MRA/mra/article/view/6222>.
COPYRIGHT: © 2025 European Society of Medicine. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ISSN 2375-1924
Abstract
Brain natriuretic peptide (pg/ml) is a cardioprotective hormone released in response to pressure or volume overload of the heart. High preoperative brain natriuretic peptide levels in persons with dysvascular major lower limb amputation may indicate cardiac stress threatening survival. The aim of this retrospective database study was to analyze the association between brain natriuretic peptide, heart failure and survival in persons with dysvascular major lower limb amputation.
Data of persons with dysvascular major lower limb amputations, at Nij Smellinghe Hospital (2010 to 2018), were included. Brain natriuretic peptide levels, determined pre- and/or post-amputation, were collected. Persons were categorized in two groups: ‘low’ brain natriuretic peptide (≤91 pg/ml) and ‘high’ brain natriuretic peptide (>91 pg/ml).
Data of 59 persons (median ge 73, interquartile range 66;80, 42 males) were included. Survivors had a significantly lower preoperative brain natriuretic peptide level (median 46, interquartile range 21;75) compared to non-survivors (median 135, interquartile range 38;316, Mann-Whitney U Test: p=0.029) and postoperative brain natriuretic peptide levels (median 26, interquartile range 16;42) compared to non-survivors (median 176, interquartile range 61;323, p=0.007). The ‘low’ brain natriuretic peptide group lived significantly longer (median 2305 days, interquartile range 1361;2979) than the ‘high’ brain natriuretic peptide group (median 687 days, interquartile range 87;1224, Log Rank=20.843; Kaplan-Meier: p=<0.001). Persons with high brain natriuretic peptide and heart failure lived shorter than those with low brain natriuretic peptide and heart failure (Kruskal-Wallis Test: p=0.008) and those with low brain natriuretic peptide without heart failure (p=0.004). Survival was shortest in the group with the high brain natriuretic peptide levels and heart failure.
In this small study, brain natriuretic peptide levels, also combined with heart failure, were associated with survival in persons with a major lower limb amputation.
Introduction
Major lower limb amputations are secondary to diabetes-related peripheral arterial disease (PAD). Mortality rates after major lower limb amputations (mLLA) at all levels proximal to the ankle are high. The 5-year mortality in persons with mLLA ranges from 52% to 80%. Myocardial infarction or heart failure (HF) are common perioperative complications in persons with a mLLA.
Brain natriuretic peptide (BNP in pg/mL), is a cardioprotective hormone released by cardiomyocytes in response to volume overload or pressure increase for cardiac stress in case of ventricular dysfunction. In persons with open revascularization, the median preoperative BNP levels (10 pg/mL) are significantly higher in non-survivors.
Methods
From the included persons, the following data was extracted from the files: age, gender, Body Mass Index (BMI), BNP levels, medical history and amputation characteristics. Medical history was categorized into PAD, HF, hypertension, DM, renal disease, chronic pulmonary disease, hypercholesterolemia and cerebrovascular accident. Heart failure was dichotomized as yes or no. Amputation characteristics included age and level of amputation and date and level of amputation.
Interaction effect of preoperative BNP level and level of amputation and date of amputation was analyzed. The median change in BNP level (per- vs. postoperative) was determined.
Results
| Variables | Total group (n=59) | Survivors* | Non-survivors | |
|---|---|---|---|---|
| Males, n (%) | 41 (69) | 9 (69) | 32 (70) | |
| BMI pre-amputation, median (IQR) | 25.22 (22.29) | 25.33 (23.30) | 25.22 (22.29) | |
| Medical history, n (%) | – Peripheral arterial disease (PAD) | 43 (76) | 11 (85) | 32 (70) |
| – Heart failure (HF) | 34 (58) | 6 (46) | 28 (61) | |
| – Hypertension | 29 (49) | 5 (38) | 24 (52) | |
| – Diabetes mellitus (DM) | 25 (42) | 5 (39) | 20 (43) | |
| – Renal disease | 10 (17) | 1 (8) | 9 (20) | |
| – Chronic pulmonary disease | 10 (17) | 1 (8) | 9 (20) | |
| – Hypercholesterolemia | 3 (5) | 0 (0) | 3 (7) | |
| – Cerebrovascular accident | 10 (17) | 1 (8) | 9 (20) | |
| Number of comorbidity, median (IQR) | 3 (2-4) | 2 (1-3) | 3 (2-4) |
| Variables | Preoperative group | BNP level in pg/mL, median (IQR) | Days before amputation determined, median (IQR) | Postoperative BNP |
|---|---|---|---|---|
| BNP level in pg/mL, median (IQR) | 91 (38.37) | 21 (7.5-33.81) | 0.026 | |
| Days after amputation determined, median (IQR) | 16 (16-32) | 0.009 | ||
| Change in BNP level (per-vs postoperative) | 1.5 (1.2-1.4) | n=4 | n=17 |
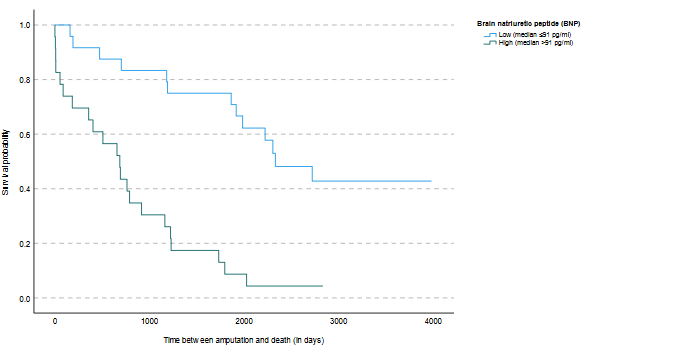
Figure 1: Survival analysis.
The survival time was measured in days from the date of amputation until February 17, 2023. The analysis compares two groups based on brain natriuretic peptide (BNP) levels: those with low BNP (median ≤ 91 pg/ml, n=24) and those with high BNP (median > 91 pg/ml, n=23). The Log-Rank test showed a significant difference between the groups (Log-Rank = 20.843, p < 0.001).
The association between HF and survival was nearly significant (p = 0.07). Persons without HF had a significantly lower preoperative BNP level (median 42, IQR 14;134) compared to persons with HF (median 145, IQR 49;417, p = 0.008). The change in BNP levels, pre- and postoperatively, in persons with HF (median 8, IQR 81;193) and without HF (median 18, IQR 9;172) did not differ significantly (p = 0.205). Survival duration (in days) was significantly (p < 0.001) different between the four groups: low BNP without HF (median 2306, IQR 1866;2724), high BNP without HF (median …
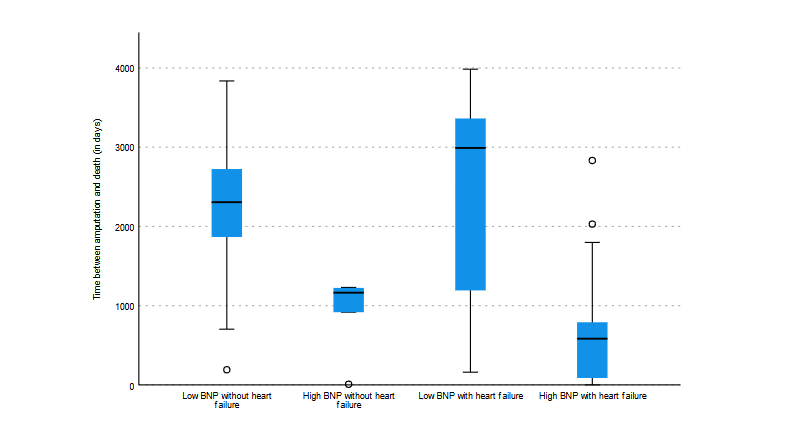
Figure 2: Boxplot Kruskal Wallis Test for BNP level, heart failure and survival.
Figure 2 shows a boxplot of brain natriuretic peptide (BNP) levels, heart failure and survival. There were four groups: low BNP without heart failure (n = 14), high BNP without heart failure (n = 5), low BNP with heart failure (n = 9), and high BNP with heart failure (n = 18). The statistical analysis revealed a significant difference between the ‘low BNP without heart failure’ and ‘high BNP with heart failure’ groups (adjusted p = 0.004), as well as between the ‘low BNP with heart failure’ and ‘high BNP with heart failure’ groups (adjusted p = 0.008). The median is shown by the line within each box, the interquartile range (IQR) by the box itself (25th to 75th percentiles). Outliers: O. BNP refers to brain natriuretic peptide.
Discussion
The results of this study showed that survivors had lower pre- and postoperative BNP levels compared to non-survivors. In addition, individuals with dysvascular mLLA and with preoperative BNP levels ≤91 pg/ml lived 1618 (median) days longer than those with preoperative BNP levels median >91 pg/ml. Our results on preoperative BNP levels are in line with the findings of a pilot study. The preoperative NT-proBNP levels in survivors (n = 15) were also lower than in non-survivors (30 days, n = 4) in that study, but the difference was not significant. The level of NT-proBNP can also be elevated in kidney failure, because the kidneys do not excrete NT-proBNP properly. In BNP this phenomenon occurs to a lesser extent.
Elimination of BNP occurs cellularly by endocytosis and only partially through the kidneys.
In a study involving persons undergoing cardiac surgery with cardiopulmonary bypass, no association was found between preoperative BNP levels and mortality but postoperative BNP levels (≥484 pg/mL) were strongly associated with mortality. In contrast, another study found that higher preoperative (NT-pro)BNP values in vascular surgery patients were associated with a higher risk for perioperative cardiovascular complications. Additionally, a retrospective cohort study (median follow-up of 7 years) among persons with cardiovascular disease found that mortality rates increased gradually with increasing BNP levels. In a meta-analysis it was suggested determining.
preoperative (NT-pro) BNP levels may facilitate risk stratification of patients undergoing noncardiac surgery. An elevated BNP level was 2 powerful predictors of adverse cardiovascular outcomes at 30 days, independent of other conventional risk factors.” A recent study supports these findings for both preoperative and postoperative BNP values.”
The (NT-proBNP is an emerging tool for screening and a guide to start a treatment in subclinical HF.” Cardiac disease may be underdiagnosed in persons with a dysvascular mLLA, Limb pain may limit their physical activity below the levels necessary to provoke symptoms of cardiac disease BNP levels also appear to be elevated in persons with asymptomatic left systolic dysfunction.” A high BNP level may assist physicians in early diagnosing and managing
cardiac stress’ in persons with dysvascular mLLAto prevent complications in the perioperative and rehabilitation phase. People with a mLLA have significantly higher energy cost of walking compared to people without an amputation.* High preoperative BNP levels in dysvascular mLLA may indicate the potential presence of a serious ventricular disease, with
implications for rehabilitation, particularly when persons begin walking with @ prosthesis resulting in additional cardiac strain. This underscores the ventricular persons with need for careful cardiac monitoring and
management in this population to. improve perioperative and rehabilitation outcomes. Persons without HF had a significantly lower preoperative BNP level compared to persons with HF. Sensitivity of BNP in diagnosing HF is much
better than its specificity which means that the test is better at ruling out HF than confirm it.” As hypothesized, our results show a significant difference between the group with a low BNP. without HF and the group with a high BNP with HF,
with a better survival for the group with a low BNP and without HF. These results suggest that the absence of (sub)clinical HF is positively linked with survival duration. Less obvious is the significant difference between the group with low BNP with HF and the group with high BNP with HF. Especially since a low BNP would exclude HF in a large proportion of cases. An expert review study showed that BNP levels are proportional to the severity of HF.” Our results showed that there is an interaction effect, where the effect of BNP is the largest. In future study also the possible treatment of HF and its effect should be monitored,
Our results showed or significant difference in change score of pre- and postoperative BNP between survivors and non-survivors. This outcome could be the effect of lack of observations or lack of an association. Arguably, the BNP level may change after amputation, because the part of the leg that is poorly perfused or infected is amputated, which can affect the load and/or stress on the heart. Furthermore, (NT-pro)BNP has a high intraindividual biological variation, which may hamper the interpretation of changes in (NT-pro)BNP levels for the detection of disease progression and their use in (NT-pro)BNP-guided treatment.”
The median survival duration for the total group is 1195 days (3.3 years, IQR 1.0;6.3), this is much higher than a mean survival of 273 days (0.75 year) in a previous study.” Consequently the 1-year survival of 75% is also higher than the 52% and 56%” in other studies or 66% in that study.” These differences might be related to the fact that in our study more knee disarticulations were performed, 42%, than in a previous study, 7%, and relatively few transfemoral amputations, 10%, and 47% in that study.” Transfemoral amputations are associated with higher perioperative cardiac event rates and higher mortality rates.2°”* Of those undergoing a mLLA, 17% had an ipsilateral reamputation. This is similar to previous studies which reported 9-26% ipsilateral reamoutations after 2 mLLA.’ These data show that the percentage of complications of the residual limb after amputation in our study is similar to previous studies.
A limitation of this study is the small sample size since BNP levels were not routinely determined in all persons to be amputated at Nij Smellinghe Hospital, possibly limiting generalization of our outcomes. However, compared to a multicente; study in the North of the Netherlands, of population appears to be similar in terms of ai (73 years versus 72 years) and gender (male 71% versus 65%).” Future research is needed to confirm or refute our results in a larger study population. A prospective multicenter study is expected to provide a larger study sample Another limitation is that the timing of the BNP determination was less standardized than anticipated. To test robustness of our outcomes, we reanalyzed our data including only those data when BNP was determined 14 days before and
after amputation. In this post-hoc analysis our reported results were confirmed (Appendix 1). Future research should prospectively measure BNP with standardized measurement protocol with BNP measurements both pre- and postoperatively, taken close to the amputation. Additionally, combined measurements of NT-proBNP and BNP
(NT-proBNP/BNP ratio’ may enhance prognostic accuracy in predicting adverse outcomes among hospitalized patients with HF.°>
Finally, we were not aole to analyze whether persons were treated for HF and whether that treatment affected survival. For future research it would be interesting whether treatment affects outcomes for this population.
Conclusion
The study highlights the importance of BNP as a promising biomarker for cardiac stress and its potential role in predicting survival outcomes in individuals with mLLA. High levels of BNP, also in combination with HF, were predictive for poorer
survival in persons with dysvascular mLLA. Elevated BNP levels in persons with a mLLA may indicate the presence of serious ventricular disease, which can complicate rehabilitation due to the increased cardiac strain associated with the higher energy
Conflict of Interest
The authors have no conflicts of interest to declare.
Funding Statement
None.
References
- Bernatchez J, Mayo A, Kayssi A. The importance of B-type natriuretic peptides (BNP) and their prognostic value after major limb amputation. Seminars Vasc Surg. 2021;34:58-68. doi:10.1053/j.semsurgs.2021.04.002.
- Cruz CP, Eltit JF, Capps C, Kirtley L, Moursi MM. Major lower extremity amputations at a Veterans Affairs hospital. Am J Surg. 2003;186(5):449-454. doi:10.1016/j.amjsurg.2003.07.027.
- Stien JR, Wong CE, Yerokun MB, et al. A meta-analysis of long-term mortality and associated risk factors following lower extremity amputation. Surg Infect. 2017;22:322-327. doi:10.1089/sur.2016.0278.
- Fortington LV, Geertzen JH, van Netten JJ, Postema K, Rommers GM, Dijkstra PU. Short and long term mortality rates after a lower limb amputation. Eur J Vasc Endovasc Surg. 2013;46(1):124-131. doi:10.1016/j.ejvs.2013.03.024.
- Maris K, Manthou D. Diagnostic and prognostic values of B-type natriuretic peptides (BNP) and N-terminal fragment brain natriuretic peptides (NT-proBNP). Cardiovasc J Afr. 2013;24(7):286-289. doi:10.5830/CVJA-2013-055.
- Ruten JH, Boomsma F, Van den Meiracker AH. Diagnostische en prognostische waarde van b-type natriuretische peptide bij hartfalen en bij aanliggende aandoeningen. Ned Tijdschr Geneeskd. 2013;157:A105.
- Subramonian B, Ponsiello F, Talord D, Park KW. Perioperative and long-term morbidity and mortality after above-knee and below-knee amputations in diabetics and non-diabetics. Anesth Analg. 2005;100(5):1241-1247. doi:10.1213/01.ANE.0000147705.87938.31.
- Wang Y, Zhang R, Huang Y, et al. Combining the use of aminoterminal pro-B-type natriuretic peptide in the prognosis of hospitalized heart failure patients. Clin Chim Acta. 2019; Apr;491:8-14. doi: 10.1016/j.cca.2018.12.125.
Appendix 1: BNP measurements in the total groups, survivors and non-survivors
| Variables | Total group | Survivors* | Non-survivors | p-value |
|---|---|---|---|---|
| Preoperative BNP | n = 38 | n = 11 | n = 27 | |
| BNP level in pg/ml, median (IQR) | 93 (32; 201) | 42 (20; 69) | 145 (41; 417) | 0.017 |
| Days before amputation determined, median (IQR) | 1 (0; 2) | 1 (1; 2) | 1 (0; 2) | — |
| Postoperative BNP | n = 32 | n = 5 | n = 27 | |
| Median level in pg/ml, median (IQR) | 145 (30; 324) | 26 (16; 42) | 239 (48; 343) | 0.009 |
| Days after amputation determined, median (IQR) | 1 (1; 5) | 1 (1; 4) | 2 (1; 5) | — |
| Change in BNP level (pre- vs postoperative) | n = 21 | n = 4 | n = 17 | |
| Median change in level in pg/ml, median (IQR) | 15 (1; 152) | 10 (0; 19) | 17 (1; 212) | 0.370 |
*Survival determined at February 17, 2023
IQR = interquartile range
Key Findings from the Text
- Preoperative BNP:
Persons without heart failure (HF) had a significantly lower preoperative BNP (median = 43 pg/ml, IQR 21–135) compared to those with HF (median = 145 pg/ml, IQR 47–423; p = 0.05). - Change in BNP levels:
The change in BNP levels between pre- and postoperative measurements was not significantly different between persons with HF (median = 7 pg/ml, IQR -2;161) and without HF (median = 16 pg/ml, IQR 9;173) (p = 0.573). - Survival duration:
- Significantly different between the four groups defined by BNP level and HF status (p = 0.001).
- Significant differences remained in post-hoc pairwise comparisons between:
- “Low BNP without HF” and “High BNP with HF” (adjusted p = 0.007)
- “Low BNP with HF” and “High BNP with HF” (adjusted p = 0.014)

