COVID-19 Impact on Primary Care Professionals’ Mental Health
Covid-19 Contamination, Changes in Work Routine, and the Impacts on the Mental Health of Primary Care Professionals in Salvador-Ba, Brazil, 2022
Erica Santana D´Agostino1, Amanda Araújo de Carvalho2, Sandra Garrido de Barros3, Maria Isabel Pereira Vianna4, Maria Cristina Teixeira Cangussu4
- Erica Santana D´Agostino PhD in Dental Health at the Federal University of Bahia, School of Dentistry/ UFBA. Rua Araújo Pinho, 6th floor, 62 Canela. Salvador-Ba, Brazil
- Amanda Araújo de Carvalho PhD student in Dental Health at the Federal University of Bahia, School of Dentistry/ UFBA. Rua Araújo Pinho, 6th floor, 62 Canela. Salvador-Ba, Brazil
- Sandra Garrido de Barros Associate Professor in the School of Dentistry / UFBA. Rua Araújo Pinho, 6th floor, 62 Canela. Salvador-Ba, Brazil
- Maria Isabel Pereira Vianna Titular Professor in School of Dentistry / UFBA. Rua Araújo Pinho, 6th floor, 62 Canela. Salvador-Ba, Brazil
- Maria Cristina Teixeira Cangussu Titular Professor in School of Dentistry / UFBA. Rua Araújo Pinho, 6th floor, 62 Canela. Salvador-Ba, Brazil
OPEN ACCESS
PUBLISHED: 31 May 2025
CITATION: D´AGOSTINO, Erica Santana et al. COVID-19 CONTAMINATION, CHANGES IN WORK ROUTINE, AND THE IMPACTS ON THE MENTAL HEALTH OF PRIMARY CARE PROFESSIONALS IN SALVADOR-BA, BRAZIL, 2022. Medical Research Archives, [S.l.], v. 13, n. 5, may 2025. Available at: <https://esmed.org/MRA/mra/article/view/6515>.
DOI: https://doi.org/10.18103/mra.v13i5.6515
ISSN 2375-1924
Abstract
The COVID-19 pandemic was a public health emergency between 2020 and 2022, with a direct impact on the lives of health professionals. The study’s objective was to identify the prevalence of contamination of the disease in primary care professionals in Salvador-Ba, Brazil, work activities changed by the pandemic, and the impacts on the mental health of these professionals. A cross-sectional study was carried out, and the reference population was the universe of professionals with higher and secondary education (N=1675) who worked in the network. An electronic form was applied from December 2021 to April 2022, including socioeconomic and demographic issues, health history and comorbidities, routine and working hours, contamination by COVID-19, and evaluation of the emotional aspects of these professionals through the application of the General Anxiety Disorder- 7 Scale (GAD-7-) and Burnout Syndrome (Maslach Burnout Inventory) questionnaire. A descriptive analysis of the variables of interest was performed using central tendency and dispersion measures as well as absolute and relative frequencies. 321 workers participated in the study, 97.20% with a workload of 40 hours per week. The female gender was the majority, 83.18%, married marital status with 57.94%, and having a postgraduate degree was the most present level of education (48.50%). Among the comorbidities, hypertension had the highest occurrence (10.59%). Most of the health professionals participated in the screening team (reception) of patients with or suspected of COVID-19 and in the organization of vaccination (>80%). Contamination by COVID-19 was 64.79%, and 41.83% attributed it to work activity. Of the total, 67.28% of workers had some type of anxiety intensity. Regarding the Burnout indices, it was observed that 47.06% had a high level of emotional exhaustion, 68.84% had a high level of depersonalization, and 99.06% considered their professional fulfillment low.
Keywords: COVID-19, workers’ health, occupational risk
Introduction
On January 30, 2020, the World Health Organization (WHO) declared the outbreak of the novel Coronavirus (SARS-CoV-2), originating in Wuhan, China, as a Public Health Emergency of International Concern (PHEIC). This was followed by the declaration of COVID-19 as a pandemic on March 11, 2020, as the disease spread globally. There was a high risk of contamination faced by healthcare professionals, particularly those in emergency and hospital settings. However, that was a limitation of international pandemic responses focused solely on individual hospital care underscored the fundamental role of Primary Health Care (APS) due to its broad scope, including epidemiological surveillance, territorial outreach, and community engagement. 1-3
Primary Health Care is the gateway to the Brazilian health system and represents an important pillar in emergency health situations, such as COVID-19, directly contributing to the reduction of morbidity. 1,2 It is worth reinforcing that, among its principles and guidelines, the territorial and community approach would allow actions to reduce the spread of the disease through health promotion and prevention, primary support for the diagnosis of suspected cases, care for mild and moderate cases of the disease, thus mitigating the collapse of health systems. In addition, it is capable of monitoring cases in isolation at home, supporting communities during social distancing, identifying and managing situations of individual or collective vulnerability, and contributing to access to health care and the necessary referral to specialized services 3- 6.
However, despite the availability of prevention guidelines and recommendations on the control of infection in the pandemic 7,8, studies on the knowledge, attitudes, and occupational risks of health professionals point to a high risk of contamination, either by caring for symptomatic patients, as well as inadequate use of personal protective equipment (PPE) and insufficient supply 9, 10; long hours of work and negligence in washing hands after contact with suspected patients, in addition to the parameters of community or family transmission 11. Contamination of primary care professionals in Brazil described so far ranged from 25%12 % to 41.9% 13, the latter analyzing only nursing professionals.
All these changes in the work routine can have effects that go beyond the physical and physiological spheres and negatively impact the psycho-emotional conditions of workers, compromising their well-being, quality of life, and work performance. 14,15 Direct consequences are psychic stress, which is expressed in generalized anxiety disorder, sleep disorders, depression, chronic fatigue and lack of energy, Burnout Syndrome, with a decrease in alertness, coordination, and efficiency; increased reaction time; impaired cognition, emotional dullness or mood swings, fear of getting sick and dying and fear of contaminating colleagues and family 9,16, 17. Boucher et al14, in a meta-analysis, pointed out that 20% of post-traumatic symptoms and 40% of health professionals manifested burnout symptoms.
Beyond anxiety, the literature also explored depression, insomnia, phobias, obsessive-compulsive symptoms, somatization symptoms, and post-traumatic stress symptoms among healthcare Workers 9. International studies from the US, Australia, and Spain corroborated these findings, revealing substantial rates of anxiety, depression, and stress10. Meta-analyses further supported these elevated levels of mental health issues across different countries12. Notably, some research suggested higher anxiety levels among primary care professionals compared to those in hospital settings. 16,17
In this sense, this study aimed to identify the prevalence of contamination of the disease in primary care professionals in Salvador-Ba, Brazil, work activities changed by the pandemic, and the impacts on the mental health of these professionals.
Methodology
A cross-sectional study was carried out, from December 2021 to April 2022, with the reference population of health professionals (Doctors, Nurses, Nursing Technicians, Dentists, Assistants, and Oral Health Technicians) from the Family Health Units of primary care from Salvador-BA (N= 1675). All professionals who were active during the pandemic period were invited to participate in the study.
A link to an electronic form with a questionnaire was sent electronically (message via cell phone, email) involving 9 blocks of questions: I- socioeconomic-demographic (gender, age, education, income, professional category, household size, household density); II- health history and reported comorbidities; III- work routine (activities performed) and working hours; IV- use of personal protective equipment; V- SARS-CoV-2 contamination; VI-contact tracing, isolation and signs and symptoms of COVID-19; VII- COVID-19 testing and vaccination; VIII-Assessment of Generalized Anxiety Disorder by the GAD-7 Scale; IX- Evaluation of the Burnout Syndrome by the Maslach Burnout Inventory (MBI) scale.
The GAD-7 scale is an instrument with the objective of tracking “Generalized Anxiety Disorder”. This instrument has seven items related to anxiety symptoms that have occurred in the last week, with four response options: 0-not at all, 1- several days, 2- more than half the days, and 3- almost every day, which correspond to the scores of 0, 1, 2 and 3, respectively. Thus, the score can vary from 0 to 21, with values corresponding to no anxiety: 0 to 4 points; mild anxiety: 5 to 9 points, moderate: 10 to 14 points, and severe: 15 to 21 points.16
The Maslach Burnout Inventory (MBI) Scale is aimed at assessing Burnout Syndrome. This instrument assesses how workers experience their work according to the three established dimensions: Emotional Exhaustion (9 items), Professional Fulfillment (8 items), and Depersonalization (5 items), totaling 22 items. 19 The following cutoff points are used: emotional exhaustion (low: zero to 15; medium: 16 to 25; and high: 26 to 54), depersonalization (low: zero to 2; medium: 3 to 8; and high: 9 to 30) and professional achievement (low: zero to 33; medium: 34 to 42; and high: 43 to 48).
The data were exported to an electronic spreadsheet, and the descriptive statistics of the variables were analyzed based on measures of central tendency and dispersion, absolute and relative frequencies. The research was approved by the Research Ethics Committee of the Federal University of Bahia.
Results
The study population consisted of 321 health professionals. Most were female (83.18%), aged between 22 and 65 years, 57.94% were married, and brown – 53.89%. Dentists had a greater participation in the research at 33.64%. Of the total, 66.04% of professionals had a family income greater than 5 minimum wages, and 35.83% of health professionals lived alone or with just one person.
| Variables | n | % | |
|---|---|---|---|
| Gender | Female | 267 | 83.18 |
| Male | 54 | 16.82 | |
| Marital Status | Single | 108 | 33.64 |
| Married (formal or informal) | 186 | 57.94 | |
| Divorced/ widowed | 27 | 8.41 | |
| Race/ Colour of the skin | Black | 81 | 25.23 |
| Brown | 173 | 53.89 | |
| White and others | 67 | 20.87 | |
| Profession | Doctor | 36 | 11.22 |
| Dentist | 108 | 33.64 | |
| Nurse | 69 | 21.50 | |
| Technician | 108 | 33.64 | |
| Higher level education | Pos Graduation | 156 | 48.50 |
| Graduation | 116 | 36.14 | |
| Technician | 49 | 15.26 | |
| House ownership | Own or form somebody in the family | 245 | 76.32 |
| Rent | 76 | 23.68 | |
| Residence footage | More than 100 m2 | 141 | 33.62 |
| Between 50-100 m2 | 146 | 45.48 | |
| Lower 50 m2 | 35 | 10.90 | |
| Family income (in minimum wage- SM) | Until 2 SM | 34 | 10.59 |
| Between 2,1 – 4 SM | 75 | 25.37 | |
| More than 5 SM | 212 | 66.04 | |
| Number of people residing with the professional | 0- 1 | 105 | 35.83 |
| 2 | 94 | 29.28 | |
| 3 or more | 102 | 34.89 |
*The minimum wage in Brazil was about 200 dollars.
On the subject of the history of comorbidities and general health status, hypertension was more frequent (n=34; 10.59%), and 8 of them also had associated diabetes. In total, 12 professionals had diabetes (3.74%). 20.2% made continuous use of medication due to some comorbidity. The use of antidepressants and anxiolytics before the pandemic represented 7.8% and 5%, respectively. During the pandemic, the use of these drugs increased to 8.7% and 10.9%.
As for working hours during the pandemic, the majority (97.20%) worked full-time (40 hours a week). Regarding employment, 76.01% reported being civil servants, while the rest were hired temporarily.
Regarding contamination by COVID-19, 64.79% declared having already been contaminated in one way. As for the signs and symptoms presented, 42.8% reported fever, 62.5% reported sore throat, 33.7% loss of taste, 36.5% loss of smell, 19.7% intestinal problems, 17.8% reported air, and 60.1% reported body aches. Only 4% required hospital care. Regarding vaccination, 77.9% of professionals received the Coronavac vaccine as the first dose (late 2020 and early 2021), and 95.6% already had the third dose administered when the questionnaire was applied.
Regarding the work routine, the results are shown in Table 2 – 80.7% participated in the screening and reception team for patients with or suspected of COVID-19, and 52.3% took rapid tests. However, only 28.7% stated that they received training to manage these patients. The continuity of routine care during the pandemic was maintained by 63.2% of professionals, and 70.4% indicated that new assignments were requested. Home visits were carried out by 29.3% of health professionals.
| Variables | n | % | |
|---|---|---|---|
| Received training in the management of patients with or suspected of having COVID-19 | Yes | 92 | 28.70 |
| No | 229 | 71.30 | |
| Participated in the screening team of patients with suspected COVID-19 | Yes | 259 | 80.70 |
| No | 62 | 19.30 | |
| Continuity of routine care during the pandemic | Yes | 203 | 63.20 |
| No | 118 | 36.80 | |
| Was part of the testing team (rapid tests)? | Yes | 168 | 52.30 |
| No | 153 | 47.70 | |
| Conducted home visits in the community during the pandemic | Yes | 94 | 29.30 |
| No | 227 | 70.70 | |
| New assignments beyond your routine were requested. | Yes | 226 | 70.40 |
| No | 95 | 29.60 |
When analyzing the impacts of the pandemic on the mental health of workers, 34.27% state that for many days they feel nervous, anxious, or on edge and 41.43% that they are not able to stop and control the worry at all, and 35.83% stated that they worried about many different things for many days, and found it difficult to relax.
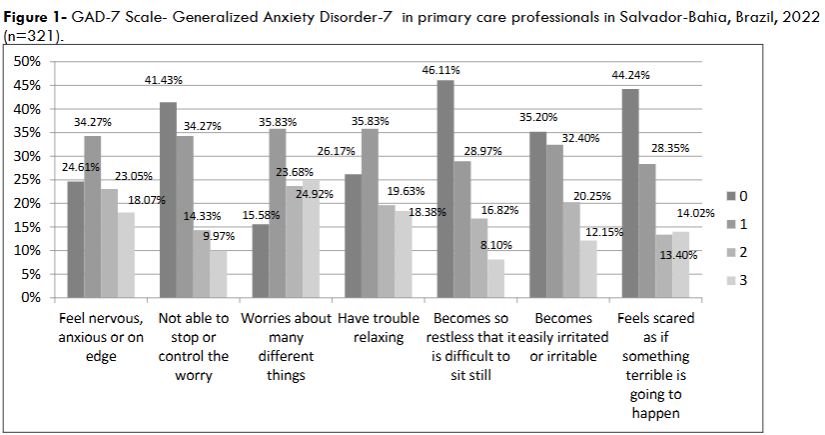
When evaluating the intensity of anxiety among health professionals, the results showed that 32.71% were without anxiety, 27.41% with a mild degree of anxiety, 24.61% with moderate anxiety, and 15.26% with a severe degree of anxiety.
To evaluate Burnout Syndrome, through the Maslach Burnout Inventory Scale (MBI), the final results are presented in Table 3.
| Variables | n | % | |
|---|---|---|---|
| Level of emotional exhaustion | Low | 87 | 27.08 |
| Average | 83 | 25.85 | |
| High | 151 | 47.07 | |
| Level of depersonalization | Low | 15 | 4.67 |
| Average | 85 | 26.48 | |
| High | 221 | 68.85 | |
| Level of personal achievement | Low | 318 | 99.07 |
| Average | 2 | 0.62 | |
| High | 1 | 0.31 |
Discussion
The prevalence of self-reported contamination by health professionals in this study was 64.79%. This percentage was high when compared to the results of international studies that evaluated the contamination rate among professionals working in PHC in Barcelona- 30.8% with positive RT-PCR 20 and Algado-Selles et al 21, also in Spain, with 14.7% in primary care.
It was also higher when compared to national studies, such as the one by Gallasch et al. 22, covering professionals from different spheres of Health Care – 30.89%, with 27% working in PHC; and those of Ferreira23, which revealed 25% of contaminated professionals throughout Brazil. Still in Brazil, Correia et al. 11 obtained a positive IgG result of 30%.
The heterogeneity between these results can be attributed to the different collection strategies used (serological tests X self-reported disease), different sample sizes, and different types of populations. It is emphasized that the production of knowledge on this subject is timely, especially since it is precisely in this sector that the responsibility for the care of patients with sequelae of the COVID-19 disease and the continuity of the planning of preventive actions in the community lies.
It is important to plan actions to support and strengthen the local area in the fight against COVID-19 within the scope of Primary Health Care in the Municipality, with measures to prevent and manage occupational risks, considering that it is precisely these professionals who are responsible for the early detection of the disease through rapid tests, tracking of identified cases, supervision, and care of sick patients, preparation of referral flows, referrals, and counter-referrals, educational activities in the territory and awareness of the population, as well as application of the vaccine, assistance to patients with sequelae of the disease, 1,4,5 in addition to continuity of care for other patients with chronic diseases, prenatal care, and child care. 2,6,24
A reformulation and/or improvement of existing surveillance actions was necessary to expand care to the community and to face the pandemic 5,24,25, which meant that they had to reconcile the updating of new routines with the demands that emerged with the pandemic and the continuity of their regular activities. 2.26
This was a highlight of this work. The reorganization of services was a reality in the municipality’s PHC – 70.4% of professionals highlighted that new attributions were requested during their workday, 80.70% needed to be part of the reception team for patients suspected of having the disease, and 52.3% were part of the testing team and reported work overload. This reality was repeated in many other locations. 20,24,25,26.
In this study, the majority (63.2%) maintained the exercises of their routine assignments, validating the importance of maintaining care for the general health of the population 26,27, but on the other hand, few professionals (29.3%) remained with the home visiting activities. It is also observed that, in general, in the European Union, face-to-face consultations have decreased, and there has been an increase in teleconsultations. 5
The modality of care through these was not evaluated in this study, but it is worth emphasizing that it was a fundamental tool, applied by several countries, 3,26,27 as a measure of organization of assistance to patients for their care and follow-up. However, even with some limitations, such as digital exclusion 25 and lack of physical contact 2,28, it was guaranteed by Ordinance No. 467, of March 20, 2020, by the Brazilian Ministry of Health. 29
In the assessed group, 67.28% of health professionals had some degree of anxiety. It is worth noting that the data showed that 8.7% began using antidepressants and 10.9% anxiolytics with the onset of the pandemic. When compared to other investigations, Shi et al. 30, 2022, in China, presented similar results – 68.1%. Lower prevalences were found in studies by Lobo et al. 31 in Brazil, in which 52% had anxiety, up to 8.3%. Described in the study by Maroto et al. 32, among physicians working in Primary Care in Spain.
In Brazil, high degrees of mental disorders and impact on quality of life have also been described in Recife. 17
Regarding the measurement of Burnout Indexes, the results presented in this study indicate that the level of emotional exhaustion in its largest scale was 47.06%, with 68.84% of depersonalization at the high level, and 99.06% considered the level of low professional achievement. When compared to studies carried out in PHC in Brazil, it was observed that results in the studies by Ferreira et al 23 showed that 52.9% of health professionals in PHC in Montes Claros-MG had Burnout Syndrome, with higher prevalence in the high level with 54.8% for exhaustion, 77.6% for depersonalization and a value close to 98.6% for low personal fulfillment. Pedrosa et al 33 had higher results for the high level of exhaustion with 59.2%, however, lower values for depersonalization with 29.6%, and only 1.4% did not feel professionally fulfilled among doctors and nurses in primary care to health in the city of Recife, PE. Although the studies by Santos et al. 34 in the Amazonia present a lower prevalence of 33.5% when compared to exhaustion at a high level, their results are superior with 84.8% of depersonalization at a high level and with the proximity in low professional achievement with 93.3%.
When compared to studies involving Burnout Syndrome in health professionals working in PHC, from other parts of the world, it was observed that in studies by Baptista et al 35, evaluating primary care physicians in Portugal, they presented high levels in the 3 dimensions of Burnout: 65.9% personal, 68.7% work-related, and 54.7% patient-related. Smaller results were reported in the studies by Lasalvia et al. 36, in Italy, with a general prevalence of 25.4% of Burnout Syndrome, also in the medical category of the APS. Apaydin et al. 37 identified that 43.4% of health professionals working in PHC had the syndrome.
It is evident that limitations exist in this study – it is a study based on cross-sectional data, with a limited sample and asymmetrical participation between different geographic areas and professional categories in the municipality. The option to search only health professionals who worked in the Family Health Units also does not represent the entire PHC in the municipality. In addition, the data obtained through the questionnaire may have biases, either due to memory or the voluntary omission of the respondent. However, it is worth noting that this is one of the few works on the contamination of Primary Health Care workers in the municipality. It highlights important elements of the work and health of health workers during the pandemic and can, therefore, provide elements that contribute to the workers’ health surveillance.
Conclusion
Based on the findings of this study, healthcare professionals in the Family Health Strategy (ESF) experienced a high rate of COVID-19 contamination. The pandemic led to significant work overload and modifications in their routines. Furthermore, the study revealed insufficient protective measures and a lack of adequate support, contributing to the increased risk of infection. Consequently, there was a notable impact on the mental health of these professionals, with high levels of anxiety and burnout observed. This research underscores the need for enhanced surveillance, support systems, and preventive strategies to safeguard the health and well-being of primary care workers during public health emergencies.
References
- Cangussú LR, Do Nascimento JAS, de Barros IRP, Cavalcanti RL, Dantas FG, Araujo DN, Silva JFC et al. Effects of primary health care and socioeconomic aspects on the dispersion of COVID-19 in the Brazilian Northeast: Ecological study of the first pandemic wave. PLoS One. 2024;19(3):e0296837. https://doi,org/10.1371/journal.pone.0296837
- Botacin GW, Gonçalves DM. Estratégia de Saúde da Família: atuação e desafios frente ao cenário de COVID-19. Cad Ibero-Am Dir Sanit. 2022;11(4):67–85. https://doi.org/10.17566/ciads.v11i4.872
- Kozhekenova N, Moiynbayeva S, Jeremic D, Dinic M, Semenov P, Nurgaliyeva Z et al. The burden of COVID-19 in primary care of Almaty, Kazakhstan, 2021-2022. Sci Rep. 2025;15(1):5186. https://doi.org/10.1038/s41598-025-89707-5
- Guimarães FG, Carvalho TML, Bernardes RM, Pinto J. A organização da atenção Primária à Saúde de Belo Horizonte no enfrentamento da Pandemia Covid-19: relato de experiência. APS Rev. 2020;2(2):74–82. https://doi.org/10.14295/aps.v2i2.128
- Ares-Blanco S, Guisado-Clavero M, Del Rio LR, Larrondo IG, Fitzgerald L, Adler L et al. Clinical pathway of COVID-19 patients in primary health care in 30 European countries: Eurodata study. Eur J Gen Pract. 2023;29(2):2182879. https://doi.org/10.1080/13814788.2023.218287
- Fernandez M, Fernandes LDAMM, Massuda A. A atenção Primária à Saúde na pandemia da COVID-19: uma análise dos planos de resposta à crise sanitária no Brasil. Rev Bras Med Fam Comunidade. 2022;17(44):3336. https://doi.org/10.5712/rbmfc17(44)3336
- Centers for Disease Control and Prevention. Interim US guidance for risk assessment and public health management of healthcare personnel with potential exposure in a healthcare setting to patients with coronavirus disease (COVID-19). Published March 7, 2020. Accessed April 2025. https://www.cdc.gov/coronavirus/2019-ncov/hcp/guidance-risk-assesment-hcp.html
- World Health Organization. Operational considerations for case management of COVID-19 in a health facility and community: interim guidance. Published March 19, 2020. Accessed April 2025. http://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid19/technical-guidance/2020/operational-considerations-for-case-managementof-covid-19-in-health-facility-and-community-interim-guidance,-19-march-2020
- Santos RPO, Nunes JA, Dias NG, Lisboa AS, AntunesVH, Pereira EV et al. Condições de trabalho na atenção primária à saúde na pandemia de COVID-19: um panorama sobre Brasil e Portugal. Cienc Saude Colet. 2023;28(10):2979–2992. https://doi.org/10.1590/1413-812320232810.10002023
- Ziani JS, Harter J, Zuge BL, Pellegrini DCP, Busanelo J, Herrera KHS. Infection and the use of personal protective equipment among Primary Health Care workers during the COVID-19 pandemic. Rev Lat Am Enfermagem. 2024;32:e4290. https://doi.org/10.1590/1518-8345.6870.4290
- Ran L, Chen X, Wang Y, Wu W, Zhang L, Tan X. Risk factors of healthcare workers with coronavirus disease 2019: a retrospective cohort study in a designated hospital of Wuhan in China. Clin Infect Dis. 2020;71(16):ciaa287. https://doi.org/10.1093/cid/ciaa287
- Fio Cruz. Pinto F. COVID-19: Estudo avalia condições de trabalho na Saúde. Accessed April 2025. https://www.fiocruzbrasilia.fiocruz.br/covid-19-estudo-avalia-condicoes-de-trabalho-na-saude/
- Correia RF, Da Costa ACC, Moore DCBC, Gomes Junior SC, Oliveira MPC, Zuma MCC, Galvani RG et al. SARS-CoV-2 seroprevalence and social inequalities in different subgroups of healthcare workers in Rio de Janeiro, Brazil. Lancet Reg Health Am. 2022;7:e100170. https://doi.org/10.1016/j.lana.2021.100170
- Boucher VG, Dahl M, Lee J, Faulkner G, Beauchamp MR, Puterman E. An umbrella review and meta-analysis of 87 meta-analyses examining healthcare workers’ mental health during the COVID-19 pandemic. J Affect Disord. 2025;375:423–436. https://doi.org/10.1016/j.jad.2025.01.109
- Aragones E, Cura-Gonzales ID, Hernandez-Rivas L, Polentinos-Castro E, San-Martín MIF, López-Rodriguez JA et al. Psychological impact of the COVID-19 pandemic on primary care workers: a cross-sectional study. Br J Gen Pract. 2022;72(720):e501–e510. https://doi.org/ 10.3399/BJGP.2021.0691.
- Denning M, Goh ET, Tan B, Kanneganti A, Almonte M, Scott A, Martin G et al. Determinants of burnout and other aspects of psychological well-being in healthcare workers during the COVID-19 pandemic: a multinational cross-sectional study. PLoS One. 2021;16(4):e0238666. https://doi.org/10.1371/journal.pone.0238666
- Cohen M, Cruz LN, Cardoso RB, Albuquerque MFPM, Montarroyos UR, Souza WV et al. Impact of the COVID-19 pandemic on the mental health of frontline healthcare workers in a highly affected region in Brazil. BMC Psychiatry. 2023;23(255). https://doi.org/10.1186/s12888-023-04702-2
- Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–1097. https://doi.org/10.1001/archinte.166.10.1092
- Maslach C, Jackson SE. The measurement of experienced burnout. J Organ Behav. 1981;2(2):99–113. https://doi.org/10.1002/job.4030020205
- Garcia-Sierra RMG, Perich EB, Dominguez JMM, Milalan NM, Cintas VS, Martínez MR et al. Descriptive study of the health services of a primary care department confined by COVID-19. Rev Esp Salud Publica. 2020;94:e202009106. PMID: 32880381
- Algado-Selles N, Gras-Valenti P, Chico-Sanchez P, Mora-Muriel JG, Soler-Molina VM, Maldonado MH et al. Frequency, associated risk factors, and characteristics of COVID-19 among healthcare personnel in a Spanish Health Department. Am J Prev Med. 2020;59(6):e221–e229. https://doi.org/10.1016/j.amepre.2020.07.014
- Gallasch CH, Silva RFA, Faria MGA, Lourenção DCA, Pires MP, Almeida MCS et al. Prevalence of COVID-19 testing among health workers providing care for suspected and confirmed cases. Rev Bras Med Trab. 2021;19(2):209–213. https://doi.org/10.47626/1679-4435-2020-722
- Ferreira ARB, Neves JV, Lucas VM, et al. Prevalência da Síndrome de Burnout em profissionais da Atenção Primária durante a pandemia do Covid-19. Rev Bras Qual Vida. 2022;14:e14995. https://doi.org/10.3895/rbqv.v14n0.14995
- Krist AH, Devoe JE, Cheng A, Ehrlich T, Jones SM. Redesigning primary care to address the COVID-19 pandemic amid pandemic. Ann Fam Med. 2020;18(4):349–354. https://doi.org/10.1370/afm.2557
- Oliveira LMS, Gomes NP, Oliveira ES, Santos AA, Pedreira LC. Estratégia de enfrentamento para Covid-19 na atenção primária à saúde: relato de experiência em Salvador-BA. Rev Gaúcha Enferm. 2021;42:e20200138. https://doi.org/10.1590/1983-1447.2021.20200138
- Sarti TD, Lazarini WS, Fontenelle LF, Almeida APSC. What is the role of Primary Health Care in the COVID-19 pandemic? Epidemiol Serv Saude. 2020;29(2):e2020166. https://doi.org/10.5123/s1679-49742020000200024
- Silva BRG, Correa APV, Uehara SCDSA. Primary health care organization in the COVID-19 pandemic: scoping review. Rev Saude Publica. 2022;56:94. https://doi.org/10.11606/s1518-8787.2022056004374
- Lourenço GM, Stefanello S, Kawanishi JY, Da Luz JAB, Silva GQ, Neto PP. A experiência de telemonitoramento por equipes de saúde da família em uma Unidade Básica de Saúde: breve relato. J Manag Prim Health Care. 2021;13:e019. https://doi.org/10.14295/jmphc.v13.1168
- Brazil. Medida Provisória nº 970, de 22 de março de 2020. Accessed April 2025. http://planalto.gov.br/ccivil_03/_ato2019-2022/mpv/mpv927.htm
- Shi LSB, Xu RH, Xia Y, Chen DX, Wang D. The impact of COVID-19-related work stress on the mental health of primary healthcare workers: the mediating effects of social support and resilience. Front Psychol. 2022;12:800183.
- Lobo BLV, Almeida PC, Cabral M. COVID-19 e a saúde mental de médicos residentes na atenção primária: medo, ansiedade e depressão. Rev Bras Med Fam Comunidade. 2022;17(44):e3163. https://doi.org/10.5712/rbmfc17(44)3163
- Maroto MAM. Resilience as a predictor of the negative impact (depression, anxiety, and stress) of COVID-19 in primary care physicians. Med Fam Semergen. 2022;48(7):e101813. https://doi.org/10.1016/j.semerg.2022.101813
- Pedrosa AN, Bitencourt L, Fróes ACF, Cazumbá MLB, Campos RGB, Brito SBCS, Silva ACS. Emotional, behavioral, and psychological impact of the COVID-19 pandemic. Front Psychol. 2020;11:566212. https://doi.org/10.3389/fpsyg.2020.566212
- Santos HMM, Fontes CJF, Lima DS. Síndrome de Burnout e qualidade de vida dos profissionais da atenção primária à saúde durante a pandemia de COVID-19, em município da Amazônia Brasileira. Debates em Psiquiatria. 2022;12:1-19. https://doi.org/10.25118/2763-9037.2022.v12.410
- Baptista S, Teixeira A, Castro L, Cunha M, Serrão C, Rodrigues A et al. Physician burnout in primary care during the COVID-19 pandemic: a cross-sectional study in Portugal. J Prim Care Community Health. 2021;12:1-9. https://doi.org/10.1177/21501327211008437
- Lasalvia A, Rigon G, Rugiu C, Negri C, Del Zotti F, Amaddeo, Bonetto C. The psychological impact of COVID-19 among primary care physicians in the province of Verona, Italy: a cross-sectional study during the first pandemic wave. Fam Pract. 2022;39(1):65-73. https://doi.org/10.1093/fampra/cmab080
- Apaydin EA, Rose DE, Yano EM, Shekelle PG, McGowan MG, Antonini TL et al. Burnout among primary care healthcare workers during the COVID-19 pandemic. J Occup Environ Med. 2021;63(8):642-645. doi:10.1097/JOM.0000000000002220

