Dynamic Sustainability in Healthcare Ecosystems
Towards a Dynamic Cross-Sector Alignment for Sustainability in Healthcare Ecosystems
Nabil Georges Badr1
- Higher Institute of Public Health, St Joseph University, Beirut, Lebanon
OPEN ACCESS
PUBLISHED: 30 June 2025
CITATION: Badr, NG., 2025. Towards a Dynamic Cross-Sector Alignment for Sustainability in Healthcare Ecosystems. Medical Research Archives, [online] 13(6). https://doi.org/10.18103/mra.v13i6.6630
COPYRIGHT © 2025 European Society of Medicine. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
DOI https://doi.org/10.18103/mra.v13i6.6630
ISSN 2375-1924
ABSTRACT
Healthcare ecosystems face significant challenges in achieving long-term sustainability while addressing public health and social service needs. This paper conceptualizes purpose-aligned systems as a framework for sustainable healthcare, emphasizing cross-sector alignment in governance, financing, data sharing, and stakeholder collaboration. By integrating concepts from the Actor-for-Actor approach, we illustrate a cyclical process of engagement, resource integration, and collective action that reinforces sustainability. The study explores the complex healthcare ecosystem, which includes healthcare practice, public health, and social services, and examines different pathways for achieving cross-sector alignment to improve population health and reduce disparities. The absence of continuity in governance, financial stability, and stakeholder trust presents a key obstacle to sustainability. Leveraging systems theory and service science, the paper argues that sustainability requires both purpose-driven design and effective purpose aligned collaboration, ensuring that healthcare ecosystems evolve dynamically rather than remain static. Using the Actor-for-Actor approach, we emphasize how healthcare system sustainability can be fostered through shared purpose, collaborative governance, and strategic resource allocation. Our proposed model highlights a cyclical value co-creation process, demonstrating how purpose-aligned healthcare ecosystems can optimize decision-making, enhance interoperability, and strengthen systemic resilience. Ultimately, the findings set the stage for further research on sustainable healthcare models, offering a conceptual foundation for continued exploration of sustainable healthcare ecosystems.
Keywords:
Actor-for-Actor approach, Healthcare ecosystem sustainability
Introduction
Service ecosystems are dynamic networks composed of interdependent actors, including businesses, consumers, policymakers, and technology providers. These actors engage in continuous interactions to co-create value and drive sustainability initiatives. However, disruptions—such as economic instability, technological shifts, or policy changes—can fragment these interactions, leading to inefficiencies and unsustainable practices.
A primary challenge in ensuring continuity within sustainable service ecosystems is the potential for disruptions caused by various factors, including economic instability, technological shifts, policy changes, and governance failures. In service ecosystems driven by sustainability principles, continuity ensures that efforts toward environmental, social, and economic sustainability do not experience abrupt disruptions that can impede long-term progress. Disruptions affect the coherence of interactions among stakeholders, reducing their ability to co-create value and align their efforts toward sustainability objectives. The absence of continuity can lead to disjointed service delivery, weakened stakeholder trust, and inefficient resource allocation.
The complex healthcare ecosystem includes domains of healthcare practice, public health, and social services. Organizations across these domains have been exploring collaboration as a way to enhance population health and address health disparities. Organizations approach collaboration from different starting points, influenced by their missions, resources, and roles.
Developing sustainable systems in the four core areas of cross-sector alignment—shared purpose, governance, finance, and shared data is widely recognized as beneficial to collaborations. Despite their differences, these domains of healthcare practice, public health, and social services must work toward a shared goal: building systems that support human health and social welfare without compromising future generations. Lanford et al. emphasize the importance of developing sustainable collaborative systems across these domains, to improve their effectiveness as a complex healthcare ecosystem. A deeper emphasis on sustainability across all core areas is needed to ensure long-term success in cross-sector collaborations. Therefore, they must co-create and maintain a purpose-aligned system, where the purpose is sustainability.
The absence of continuity in governance, resource management, and stakeholder collaboration poses a significant challenge to maintaining a purpose-aligned system. For instance, in service ecosystems dependent on government regulations, abrupt policy changes can create uncertainty for businesses and consumers. Another major disruption comes from financial instability. Many sustainability-driven service ecosystems rely on continuous funding to support operations, innovation, and stakeholder initiatives. When financial support wavers or investment strategies shift unpredictably, projects and partnerships aimed at sustainability suffer from inconsistency, stalling or failing altogether. Similarly, technological advancements aimed at timely data sharing that do not align with existing ecosystem structures may result in inefficiencies and fragmentation. Without continuity in governance mechanisms, businesses and consumers may struggle to maintain sustainable practices, leading to a decline in ecosystem performance. Therefore, in this paper we study the complex healthcare ecosystem as a purpose-aligned system with sustainability as the purpose. The complex system includes domains of healthcare practice, public health, and social services. We explore different pathways for achieving cross-sector alignment for sustainability. We methodically illustrate an example of a cyclical purpose alignment through the A4A approach, where the purpose is sustainability. Finally, we propose a conceptual model to summarize a cyclical value co-creation process, demonstrating how purpose-aligned healthcare ecosystems can optimize decision-making, enhance interoperability, and build effective purpose aligned collaboration among stakeholders to strengthen systemic sustainability.
Background
PUBLIC HEALTH SUSTAINABILITY
Sustainability in public health, social services, and healthcare practice shares a common foundation of promoting equity, accessibility, and long-term resilience. All three sectors strive to ensure that essential services remain available to all, particularly underserved communities, while integrating environmental responsibility and resource efficiency to secure lasting impact. Each recognizes the interconnectedness between human well-being and environmental health, emphasizing responsible practices that mitigate ecological harm and enhance societal stability. However, though they align around the purpose of human wellbeing, their approaches to sustainability differ based on their primary objectives.
The Sustainable Development Goal 3 (SDG 3) of the United Nations aims to ensure healthy lives and promote well-being for all at all ages by supporting a more equitable and resilient healthcare system worldwide. Public health sustainability complements were not only defined in the context of reducing healthcare’s carbon footprint, responsibly managing medical waste, and preparing for climate-related health challenges. It stipulates that a healthcare ecosystem including healthcare practice, public health, and social services must create a balanced, forward-thinking system that supports human well-being without compromising future generations. These sectors must align on a shared purpose, with clear governance, well-planned financing, and shared data for better health monitoring, improving decision-making, and fostering collaboration among stakeholders. Sustainability in social services, healthcare, and public health revolves around creating long-term, equitable solutions that support communities while preserving resources for future generations. Social services concentrate on fostering community resilience and reducing systemic inequalities through policies that support vulnerable populations. Social services focus on fostering inclusive policies that promote social equity, improve access to essential services like healthcare and education, and address systemic inequalities. They prioritize community welfare, advocate for human rights, and integrate environmental and economic considerations to build resilient societies. In contrast, healthcare practice prioritizes sustainable medical care, optimizing hospital operations, ethical procurement, and minimizing medical waste to ensure effective and responsible patient treatment. Healthcare sustainability ensures that high-quality medical care remains accessible while minimizing environmental impact. Hospitals and clinics adopt greener practices, such as reducing waste, utilizing renewable energy, and conserving water, while cost-effective healthcare models maintain affordability and equity across the ecosystem of public health, social services, and healthcare practice.
SUSTAINABLE HEALTHCARE ECOSYSTEM
A sustainable service ecosystem is a dynamic, interconnected environment where actors—organizations, customers, policymakers, and other stakeholders—continuously interact to create and deliver value. Research often lacks a focus on sustainability, with shared purpose typically seen as static rather than evolving, governance studies tending to prioritize short-term collaboration over institutional stability, and healthcare finance research highlighting difficulties in securing long-term funding without clear sustainability solutions. While shared purpose can help bridge differences, it cannot fully eliminate conflicting goals. On the other hand, financial strategies, particularly those shaped by geopolitical factors, vary widely, as do approaches to shared data, depending on available resources. Shared data, in contrast, is more sustainability-oriented, as its challenges mainly arise during initial implementation, with long-term benefits expected over time.
PURPOSE ALIGNMENT TOWARDS SUSTAINABILITY
A purposeful system is one that inherently possesses purpose, adapting to achieve a certain goal, dynamically based on changing conditions. Purposeful systems theory in healthcare refers to a systems approach that can improve patient care and reduce adverse events. We can therefore depict a purposeful system, is one that inherently possesses purpose, usually, patient outcome. It emphasizes coherence between the system’s components and an overarching objective. For example, a purposeful healthcare system involves adapting and contextualizing principles from systems thinking for quality improvement, and often using information/communications technologies and systems-engineering tools to achieve a patient-centered healthcare.
A purpose-aligned system, on the other hand, is one that is designed or structured to align multiple components of a system with a specific purpose or goal. This term suggests that the system is intentionally shaped to serve a particular function. Therefore, we focus on the system’s state of sustainability rather than outcome. In our context, we review a purpose-aligned system, intentionally shaped to serve a particular function, here to be sustainable. Therefore, by definition, in a purpose-aligned system, stakeholders must work toward common goals, effective governance provides leadership and structure, financial sustainability secures ongoing funding for initiatives and shared data and measurement systems help track progress and improve coordination. Sustainability of a system producing the service can be therefore understood through the lens of fitness for use and fitness for purpose. The system is sustainable when it is designed to achieve long-term environmental, social, and economic goals (Fitness for Purpose) and continue to be accessible, beneficial and adaptable to changing conditions (Fitness for Use). In essence, sustainability requires both purpose-driven design (meeting long-term sustainability goals) and practical usability (ensuring adoption and effectiveness). Purpose-aligned sustainable systems must ensure rapid and informed decisions, allocate resources, and manage information in ways that reinforce sustainability. Information flows must include feedback loops that close the cycle on a sustainable healthcare ecosystem.
SUSTAINABILITY THROUGH THE LENS OF SERVICE SCIENCE
The Service-Dominant (S-D) Logic perspective underscores the importance of value co-creation within healthcare ecosystems, where individuals, organizations, and institutions collaboratively engage to generate systemic benefits beyond isolated transactions. Sustainable healthcare systems must evolve continuously, relying on knowledge-sharing, proactive governance, and evidence-based decision-making. In the context of S-D Logic we can emphasize value co-creation through resource integration and service exchange. This leads us to the conversation about actors (businesses and individuals), viewed as interconnected systems, working toward a common goal. This logic is also rooted in a systems theory that examines how socio-economic entities interact to establish sustainable relationships, also referred to as the Viable Systems Approach (VSA). Fundamentally, viable systems maintain structural compatibility (consonance), meaning their components work in synergy, while ensuring adaptive flexibility (resonance), allowing them to evolve in response to emerging challenges. In that context, a sustainable healthcare system prioritizes long-term viability, balancing resources, funding, environmental impact, and equitable access. Sustainable health models focus on preventive care, efficient use of medical supplies, and policies that address socio-economic disparities. These models must be viable and can adapt, maintaining fostering effective connections with other interacting entities while balancing shared objectives and expectations in a harmonious way. A viable healthcare system requires harmonized interactions among diverse actors, including hospitals, primary care providers, social service agencies, and governmental health programs. For instance, in healthcare ecosystems, viable systems incorporate integrative healthcare models, aligning social services, clinical practices, and public health initiatives to ensure holistic well-being rather than fragmented interventions. VSA reinforces that systems must manage complexity through self-regulation, meaning sustainable structures evolve via resource integration, feedback loops, and dynamic learning mechanisms rather than rigid, top-down control. By applying VSA principles to sustainability, organizations, policymakers, and communities can transition toward resilient, purpose-aligned systems, ensuring that their efforts lead to long-term viability rather than short-term fixes. For example, in pandemic response strategies, hospitals, public health agencies, and social services must align efforts to optimize resource allocation, preventive care, and crisis management, fostering resilience and adaptability.
Discussion
From the perspective of value-based healthcare, we can frame the concept of a purpose-aligned healthcare ecosystem through the lens of the Actor-for-Actor (A4A) approach. To elucidate purpose-alignment, for this paper we use the Actor-for-Actor (A4A) approach perspective that emphasizes the dynamic interactions between actors in a service ecosystem, recognizing all actors contribute to value co-creation (here sustainability is the value outcome) regardless of their formal roles.
UNDERSTANDING PURPOSE ALIGNMENT THROUGH THE A4A APPROACH
The Actor-for-Actor (A4A) approach provides a compelling lens through which to examine complex ecosystems, emphasizing systemic interactions that drive emergence, adaptation, and sustainability. Unlike traditional dyadic exchanges, A4A relationships operate within multi-layered ecosystems, where diverse actors—including individuals, communities, institutions, and environmental systems—engage not merely for personal benefit but to sustain the viability of the overall system. These relationships facilitate resource integration, mutual adaptation, and emergent behaviors, ensuring the resilience of ecosystems despite external pressures, thus enhancing the sustainability of the service system.
Furthermore, continuity in a sustainable service ecosystem is not merely a desirable feature but an essential foundation for long-term success. Disruptions in governance, stakeholder collaboration, resource management, or financial stability can hinder sustainability efforts, making continuity a critical factor in ensuring resilience and adaptability. As service ecosystems become increasingly interconnected, stakeholders must adopt strategies that foster continuity across different domains. Whether through stable governance, technology integration, institutional memory retention, or financial stability, ensuring seamless interactions is key to maintaining sustainability objectives. A4A helps identify the cyclical focus on foundational conditions for actor engagement and relationships, followed by an assessment of systemic factors and their role in fostering alignment to purpose, where the aim of equity is a catalyst for alignment and sustainability. Hence, the cyclical characteristic of these interactions, illustrated in Figure 1, demonstrates the systemic continuity that propels the collaboration into a value creating feedback loop, as the ecosystem converges to align to the purpose of sustainability.
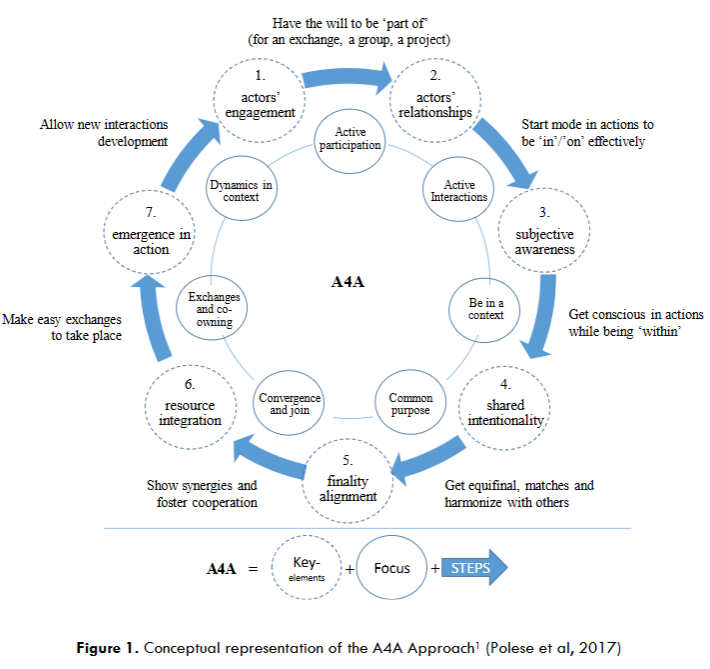
Complex ecosystems, whether social, economic, or ecological, are characterized by interdependencies among actors whose interactions generate value beyond the sum of their individual contributions. In an A4A-driven healthcare ecosystem, actors do not merely fulfill predefined roles; they adapt, share knowledge, and co-create solutions tailored to evolving contextual challenges. Each actor becomes invested and actively involved in a defined role within the healthcare ecosystem [A4A-1. Actors’ engagement]. The Actor-for-Actor (A4A) approach aligns closely with the concept of purpose-aligned systems, where interconnected entities collaborate based on a common goal or higher-order purpose, optimizing collective impact rather than fragmented, independent actions. Once the initial connection among key actors is established, engagement begins, leading to continuous interactions driven by aligned objectives and shared goals [A4A-2. Actors’ relationship]. Within a complex ecosystem populated by diverse participants whose behaviors can directly or indirectly influence engagement, awareness emerges as a crucial factor in recognizing different dimensions of alignment that shape the ecosystem’s success [A4A-3. Subjective awareness]. At the core of alignment lies the notion of shared intentionality [A4A-4. Shared intentionality], wherein actors recognize their interdependence and direct their efforts toward a coherent, system-wide finality. In these settings, A4A relationships encourage shared intentionality—where actors align their decisions with the collective survival and co-evolution of the system rather than acting in isolation. Collaboration among all actors, guided by shared intentionality and the belief in mutual benefit, allows for the achievement of common goals and the resolution of systemic gaps. Cooperation leads to mutual satisfaction and focuses on collective goals [A4A-5. Finality alignment]. Every component of the healthcare system—from providers and patients to caregivers, information networks, regulatory frameworks, financial systems, service delivery models, assessment mechanisms, patient empowerment, education, and research—must be aligned to advancing the value and fairness of healthcare during the next phase of transformation. Within A4A, this is termed resource integration [A4A-6. Resource Integration]. Resource integration is essential to mobilizing a system of actors into action [A4A-7. Emergence in action]. The cyclical characteristic of these interactions, illustrated in Figure 1, propels the collaboration into a value creating feedback loop, as the ecosystem converges to align to the purpose of sustainability.
PURPOSE ALIGNED HEALTHCARE ECOSYSTEM FOR SUSTAINABILITY
As discussed, the Actor-for-Actor (A4A) lens enhances the understanding of healthcare ecosystems by emphasizing collaborative resource integration among diverse stakeholders—including healthcare professionals, policymakers, social workers, community organizations, and patients—to promote equitable access, holistic care, and long-term sustainability. Through the A4A lens, using a system dynamics approach, we can identify aspects of purpose aligned healthcare ecosystems. Notably, notions of proactivity, the convergence of ideas and values, shared intentionality, focusing on equifinality, cognitive alignment, participating in resource integration, then emergence in action, and viability.
| A4A Cycle | Indications for alignment |
|---|---|
| A4A-1. Actors’ engagement | Initiate and Collaborate – Actors work together and collaborate toward a shared objective maximizing their collective influence rather than operating as isolated, independent units. |
| A4A-2. Actors’ relationship | Form Relationships aligned to the purpose – The relationships among actors extend beyond traditional patient-provider interactions, incorporating community health workers, non-profit organizations, and policymakers to address health holistically. |
| A4A-3. Subjective awareness | Transform to merge in context – Relationships are not merely transactional but transformative, allowing actors to participate in shaping emergent value propositions that benefit all stakeholders. |
| A4A-4. Shared intentionality | Establish Trust – Trust-based collaboration is essential. Therefore, understanding the factors and limitations affecting each actor fosters the creation of a collective purpose that is essential to alignment. |
| A4A-5. Finality alignment | Focus on sustainability – Actors become aware that they must align their individual priorities with systemic sustainability. |
| A4A-6. Resource Integration | Timely, effective and efficient use of resources – Resources must be coordinated to ensure sustained and accessible care for all patient groups regardless of geographical, social, or logistical barriers that could hinder their ability to reach care facilities. |
| A4A-7. Emergence in action | Act, transform, learn, adapt and re-engage – Emergence in action fosters systemic viability by ensuring that social services address determinants of health, healthcare providers deliver direct patient care, and public health initiatives focus on preventive strategies and population health management. |
In a healthcare ecosystem, one that is aligned for sustainability, actors engage as interconnected entities work together toward a shared objective or overarching mission, maximizing their collective influence rather than operating as isolated, independent units. The relationships among actors extend beyond traditional patient-provider interactions, incorporating community health workers, non-profit organizations, and policymakers to address health holistically. As healthcare systems evolve amidst demographic shifts, technological advancements, and global health challenges, adopting viable system thinking ensures resilient, equitable healthcare delivery that safeguards public health for future generations.
In such ecosystems, relationships are not merely transactional but transformative, allowing actors to participate in shaping emergent value propositions that benefit all stakeholders. Whether examining urban development, digital economies, or ecological sustainability, our lens of the A4A framework illustrates how actors contribute to the self-regulation, knowledge sharing, and iterative evolution of ecosystems in response to complexity. Cultural differences among actors should be nurtured through trust and empathy to maintain shared goals. Aside of shared vision, values and goals of stakeholders, trust is important to reach consensus and alignment among all stakeholders. This evolves into setting collective goals, upholding agreed-upon ethical values, and fostering an environment of trust, which is often enriched by previous collaborative endeavors and partnerships. Trust-based collaboration is essential in preventive care, mental health services, and chronic disease management, where social support systems significantly influence health outcomes. Therefore, understanding the factors and limitations affecting each actor fosters the creation of a collective purpose that is essential to alignment.
Actors become aware that they must align their individual priorities with systemic survival. Purpose-aligned systems offer a structured mechanism to achieve this alignment by embedding shared values and collective governance models into their operational logic. The need for adaptability underscores the importance of tailoring health integration strategies to local conditions, the market dynamics or specific regional factors, such as institutional context, organizational structure, demographic, economic, political, legal, ecological, socio-cultural, and technological factors, in the environment where integration will take place. It’s about ensuring relevance and responsiveness.
An effective Healthcare Service Ecosystem must emphasize the notion of well-being co-creation which entails a dynamic interplay of actors, in face of the challenges, with their ability to use the available resource pools, at the different system levels, especially in cases of pandemic response, that require agility in resource realignment. Once a healthcare decision is made, resources must be coordinated to ensure sustained and accessible care for all patient groups, regardless of geographical, social, or logistical barriers that could hinder their ability to reach care facilities. Long-term strategy for resource integration ensures adaptation while keeping actors engaged in shared goals, mobilizing a system of actors into action. Another catalyst to integration is the co-location of resources emphasizing the importance of placing health service providers in shared or nearby locations and ensuring that every stakeholder in the health system understands their specific functions and responsibilities as they emerge in action.
Emergence in action fosters systemic viability by ensuring that social services address determinants of health, healthcare providers deliver direct patient care, and public health initiatives focus on preventive strategies and population health management. Whether in corporate organizations, social networks, or economic systems, purpose-aligned frameworks promote ethical decision-making and long-term sustainability, ensuring that the value generated benefits all stakeholders rather than favoring select participants. Instead of competing for limited resources, actors in purpose-aligned systems embrace collaborative governance, allowing for self-regulation, knowledge-sharing, and iterative innovation that strengthens the entire network. This dynamic interplay fosters system emergence, where interconnected actors continuously redefine and enhance their roles in response to environmental complexity.
DEVELOPING SUSTAINABLE SYSTEMS
For sustainability, Landers et al. identify four core areas of cross-sector alignment—shared purpose, governance, finance, and shared data. From our review, we develop a high-level discussion on the four areas as they connect to ecosystem sustainability.
PURPOSE-ALIGNED HEALTHCARE ECOSYSTEMS
Ultimately, understanding A4A relationships represents a foundational paradigm for understanding adaptive ecosystems, reinforcing that systemic viability relies on cooperation, shared purpose, and value co-creation across diverse entities. As global challenges—such as climate change, socio-economic inequalities, and technological disruptions—require ecosystem-wide responses, A4A offers a pathway to rethinking sustainability, fostering collective action, and ensuring the long-term survival of complex systems. By embracing collective responsibility, and aligning the commitment to the cyclical A4A model, actors in healthcare ecosystems foster sustainable health equity, reducing disparities while enhancing service accessibility.
Purpose-Aligned healthcare ecosystems must tackle challenges like fragmented care, inefficiencies, and escalating costs. By fostering interoperability and collaboration among stakeholders, these systems enhance treatment optimization, improve disease management, streamline healthcare processes, and promote healthier lifestyles. Additionally, they drive innovation and progress by strengthening coordination and leveraging data effectively across partners.
A sustainable service ecosystem thrives on the seamless integration of resources, actors, and processes, all working toward a shared purpose. It ensures continuous healthcare service, a service that is uninterrupted, coordinated, and accessible medical care for individuals across different stages of their health journey. It integrates preventive, acute, chronic, and rehabilitative care to provide seamless support without gaps in treatment. Disruptions in service delivery, stakeholder engagement, and resource allocation can hinder long-term sustainability efforts. Service ecosystems risk fragmentation, inefficiencies, and failure to achieve their purpose-aligned goals. Furthermore, a sustainable healthcare service ensures that medical care meets present needs without compromising environmental, economic, or social resources for future generations. It integrates efficiency, resilience, and ethical practices to create a healthcare system that is both effective and enduring. To clarify, a resilient healthcare service is one that can withstand, adapt to, and recover from disruptions while maintaining quality care for patients. It ensures that healthcare systems remain functional during crises such as pandemics, natural disasters, cyberattacks, or economic downturns. Nevertheless, due to its lack of clarity, the existing conceptualization of health systems resilience impedes progress in expanding knowledge, refining analytical tools, and enhancing communication.
GOVERNANCE FOR SUSTAINABILITY
Effective governance in integrated health systems relies on structured leadership, including governing boards, leadership assemblies, and steering committees. These elements ensure smooth coordination, timely policy updates, and a clear strategic direction. Strong cooperation fosters shared satisfaction and keeps the focus on collective goals. Among other notions, the literature conceptualizes health system integration as the alignment of stakeholders; that is the strategic engagement and alignment of all parties involved in health care. Including community engagement which is about proactively drawing the broader community into the health system integration process. Governance structures that involve crafting and implementing an organizational blueprint consisting of governing boards, leadership assemblies, and steering committees’ structures are imperative to guaranteeing smooth coordination, policy updates, and setting the strategic course in integrated health environments. It emphasizes the importance of strong relationships among health providers, organizational members, and decision-makers. Stakeholders must guide, support, and implement changes to achieve successful health system integration and alignment.
FINANCIALS ALIGNMENT
The literature advocates for structural changes, including investment in digital infrastructure, clinician training, and data transparency to mitigate healthcare inequities. To achieve resource integration, adequate funding must be sourced, often from varied channels, both public and private, and leveraging a combination of monetary and non-monetary incentives to intentionally align health system integration endeavors effectively. With regular engagements, efficient data transmission, and structured technology integrations, it aims to promote a cohesive team-oriented approach. To reach and maintain alignment, an essential care must facilitate dialog, communication and coordination capabilities of the care team, this can be achieved by collecting the necessary data from the treatment protocol and translating feedback from treatment information to provide a learning opportunity for the care team.
DATA & TECHNOLOGY
The continuous exchange of information and resources is crucial for sustained value despite ecosystem changes. By integrating digital health technologies, telemedicine, and community-based interventions, these, now aligned, relationships create harmonized networks that optimize resource utilization and systemic durability. Embracing emerging technologies and evolving healthcare models to meet changing needs. The creation and effective use of shared technological platforms ensure consistent and efficient sharing of vital information, ranging from medical records to clinical data, promoting better communication and a streamlined delivery of services. These principles create a healthcare ecosystem that is not just reactive but proactive, ensuring better health outcomes and long-term sustainability. Research has conceptualized equitable service provisioning and delivery using digital health technology in a smart health ecosystem, powered by knowledge integration in smart cities. For example, telehealth-based services are proclaimed to improve accessibility, especially in underserved areas, to meet patient needs. Virtual care will persist to build the needed foundation for safe and effective care with the right clinician, at the right time, and at the convenience of the patient. The provision of health care services through telehealth technologies has revealed a reassuring effect in the lives of patients. It has the potential to offer safe, timely and effective interaction with the healthcare provider at the convenience of the patient (according to his or her time schedule, saving travel time for those in rural areas).
CONCEPTUALIZED REPRESENTATION
In the following section, we build on the framework proposed by Landers et al. and incorporate concepts from our analysis of the cyclical value derived from the A4A approach, to strengthen the sustainability of a healthcare ecosystem. This theory of change builds upon established public health and social change models, specifically addressing how healthcare, public health, and social services can collaboratively meet community needs in a sustainable manner. The components of cross-sector alignment operate at individual, organizational, and systemic levels, driven by community participation. Other external factors may serve as drivers of alignment, while elements such as trust, engagement, accountability, and evidence influence its moderation. However, alignment does not always require extensive resources—rather, the level of sophistication should be adapted to contextual constraints.
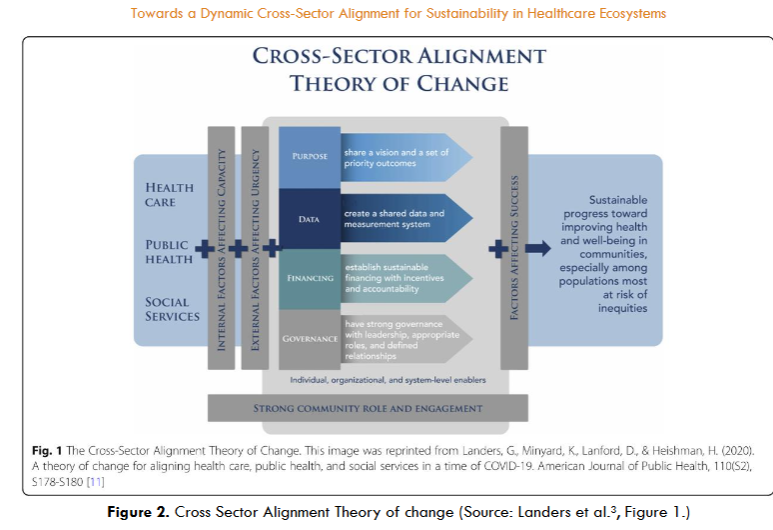
Given the complexity and variability of collaboration, different pathways to cross-sector alignment will emerge, each with distinct challenges. It is crucial to formally define these pathways to equip individuals and organizations with the tools to navigate relevant obstacles and opportunities. Furthermore, the core components of alignment are interdependent, reinforcing one another both immediately and over time. Shared purpose does not necessarily imply a singular priority, as each partner brings unique motivations to a collaboration. Establishing shared goals is important, but so is the management of divergent priorities.
We suggest a model for healthcare ecosystem sustainability through a conceptual theory of change. This model emphasizes four key components: purpose, data, financing, and governance. Purpose refers to the focus of cross-sector efforts that are informed by and supportive of community voices. Data must be shared in a way that is meaningful to all partners, enabling effective coordination and measurement of progress. Long-term financing should support partnerships through incentives and accountability, while governance structures need to be robust, inclusive, and representative of local communities.
The main premise of this model is the cyclical value co-creation produced by an effective purpose aligned collaboration focused on maintaining a sustainable Healthcare Ecosystem. We illustrate an engagement model of purpose aligned collaboration where actors initiate and collaborate as they work toward a shared objective maximizing their collective influence rather than operating as isolated, independent units. They form relationships aligned to the purpose (here establish and maintain a sustainable ecosystem). The relationships among actors extend beyond traditional patient-provider interactions, incorporating community health workers, non-profit organizations, and policymakers to address health holistically. Relationships are not merely transactional but transformative, allowing actors to participate in shaping emergent value propositions that benefit all stakeholders as they transform to merge in context. The collaborating actors establish trust and foster the creation of a collective purpose that is essential to alignment. Actors become aware that they must align their individual priorities with systemic sustainability. Timely, effective and efficient use of resources must be coordinated to ensure sustained and accessible care for all patient groups regardless of geographical, social, or logistical barriers that could hinder their ability to reach care facilities. The collaboration culminates as collaborators act, transform, learn, adapt and re-engage. Emergence in action fosters systemic viability by ensuring that social services address determinants of health, healthcare providers deliver direct patient care, and public health initiatives focus on preventive strategies and population health management.
Healthcare Equity as a Sustainable Healthcare Ecosystem
Healthcare equity relies on complex systems design principles that encompass leadership, sustainable collaboration, consistent data collection, performance measure stratification, enhanced care delivery, effective communication, and strategic implementation to address the needs of special populations. By integrating leadership, sustainable collaboration, and data-driven decision-making, healthcare systems can improve care delivery and communication while addressing disparities in special populations. The strategic implementation of these principles ensures that performance measures are effectively utilized, ultimately enhancing equitable access to quality healthcare. Therefore, a purpose-aligned healthcare ecosystem focused on maintaining sustainability should be built on principles that ensure equitable, efficient, and sustainable healthcare delivery.
Conclusion
This paper presents a conceptual framework for sustainable healthcare ecosystems, emphasizing a cyclical approach to maintaining sustainability in complex healthcare environments. By applying the Actor-for-Actor (A4A) methodology, we propose a value co-creation model that reinforces systemic resilience through purpose-aligned collaboration, shared governance, financial stability, and integrated data practices.
While this paper offers a foundational perspective, it is important to acknowledge its limitations. As a conceptual framework, its insights remain theoretical and require empirical validation. Future research should aim to operationalize and test these concepts within real-world healthcare systems, assessing their effectiveness in fostering sustainability. Despite these limitations, the framework significantly contributes to the literature by offering a structured lens to examine healthcare sustainability through dynamic, iterative engagement.
By providing a novel perspective on cyclical purpose-alignment, this paper sets the stage for further scholarly inquiry into sustainable healthcare models. We encourage researchers and practitioners to expand upon this concept, exploring new methodologies and practical applications to strengthen the adaptability and long-term viability of healthcare ecosystems.
Ultimately, the findings set the stage for further research on sustainable healthcare models, offering a conceptual foundation for continued exploration of sustainable healthcare ecosystems.
Conflict of interest
The authors have no conflicts of interest to declare.

