Global Review of Accountable Care Organizations
A Global Review of Accountable Care Organizations: Design Features and Lessons Learned
Michael D. Finch 1,2, Stephen T. Parente 1, Anna C. Grossbach 3, Daniel K. Zismer 4, Mohammed Alluhidan 5, Abdulrahman Alfaisal 5, Rana Saber 5, Adwa Alamri 5, Yi Zhang 6, Di Dong 6, Christopher H. Herbst 6
- University of Minnesota Minneapolis, MN, USA ; Children’s Minnesota Research Institute, MN USA
- University of Minnesota Minneapolis, MN, USA
- The Medical Industry Leadership Institute, MN, USA
- Health Systems Innovation Network LLC, MN, USA
- Saudi Health Council Riyadh, Saudi Arabia
- World Bank, Washington DC, USA
OPEN ACCESS
PUBLISHED: 31 December 2024
CITATION: FINCH, Michael D. et al. A Global Review of Accountable Care Organizations: Design Features and Lessons Learned. Medical Research Archives, [S.l.], v. 12, n. 12, dec. 2024. Available at: <https://esmed.org/MRA/mra/article/view/6074>.
COPYRIGHT: © 2025 European Society of Medicine. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
DOI: https://doi.org/10.18103/mra.v12i12.6074
ISSN 2375-1924
Abstract
As health systems around the world increasingly adopt accountable care models, certain design features tied to success begin to emerge. This review draws upon lessons learned from three accountable care models: Health Maintenance Organizations, Accountable Care Organizations (ACOs), and Advanced Primary Care.
Five elements are integral to the success of accountable care models. First, continuous strengthening of organizational alignment among health providers within ACOs to achieve shared visions and goals at operational, cultural, and cognitive levels. Second, partnerships to improve the scope of clinical operations (horizontal integration of service lines) to build efficient resource interdependence and collaboration to deliver consistent high-quality care at a scale that includes a full spectrum of clinical services (primary care through long-term care). Third, availability of adequate health information management and health information technology to improve patient management, coordination, and engagement. Fourth, employing risk adjustment models that accurately estimate the cost of the highest-risk patients to ensure sustainable health financing. Finally, using performance benchmarks to incentivize high-performing groups, achieving organizational transformation.
Applying these models’ successes internationally requires leadership to understand cultural and clinical contexts, providers to commit to developing competencies, and governing bodies to address systemic impediments to providers’ ability to work together to improve patient access, experience, and outcomes, while reducing costs.
Keywords
Accountable Care Organizations, Health Maintenance Organizations, Advanced Primary Care, Health Systems, Health Information Technology
Introduction
There is growing global interest in developing models of integrative care as a pathway to increasing access to quality care while slowing the growth of health care spending. The term integrative care has come to describe a broad range of implementations that share little else in common. Back in 2009, Armitage et al. documented over 175 overlapping definitions and concepts of integrated care. In their 2012 evaluation of the United Kingdom’s Department of Health Integrated Care Pilots, RAND went so far as to warn “. . . we take care to avoid confusing and inaccurate generalizations about the merits or otherwise of ‘integrated care’ as though there was some fundamental agreement about its meaning”.
Globally, the design and implementation of models of integrated care is highly heterogenous, which makes comparison of experiences challenging. The heterogeneity between implementations across national comparisons made it difficult to understand which parts of the integrated care model were the most important, the most effective, or the most equitable, as both findings, and the strength of those findings, are not generalizable across countries. In the end, the World Health Organization report on integrated care concluded: “The concept of integrated care is strongly shaped by perspectives and expectations of various users in the health system, making a unified definition difficult. Interestingly, all definitions converge around highlighting the central role of population and individual. Furthermore, adopting a health system perspective, the use of the term ‘integrated health service delivery’ is seen as more reflective of the notion”.
Materials and methods
This review draws on a well-recognized definition of accountable care, which incorporates three of the most recent models that emerged out of the older framework of integrated care. Accountable care is “a system in which a group of providers are held jointly accountable for achieving a set of outcomes for a prospectively defined population over a period of time and for an agreed cost”. This is the definition first used by McClellan et al. after recognizing the heterogeneity of the concept and the resulting complications in a definitive definition. It is this definition that we employ in the remainder of this work. This definition of accountable care incorporates three of the most recent models to grow out of the older integrated care framework: health maintenance organizations (HMOs) (as well as their various incarnations), accountable care organizations (ACOs) (along with implementations of various, but not comprehensive, forms of the original US implementation of ACOs), and advanced primary care practices. Each of these contains the essential elements of an accountable care model but represents different implementations of the model.
Results
This section describes the development of three main accountable care models and their early implementations. They are HMOs, ACOs, and advanced primary care providers.
HEALTH MAINTENANCE ORGANIZATIONS
An HMO features a network of health care providers that treat a voluntary patient population for a prepaid cost. As such, HMOs combine financing and care delivery, creating an incentive to provide cost-efficient quality care. Thus, the HMO acts as both service provider and insurer. In contrast to the traditional fee-for-service (FFS) system, where providers decide what care to administer and then seek payment for that care from insurers, the HMO receives a capitated payment (a fixed payment) for each member in the organization. In the United States, HMOs are funded by contracts with public entities such as Medicaid/Medicare in the US, or private entities such as employers. These entities usually compete by offering low overall costs for a defined population while ensuring acceptable access to care, quality services, and positive population health outcomes. The HMO model is designed to incentivize and maximize the quality and efficiency of service delivery. The very design of an HMO incentivizes the plan to engage high-quality care for its members while stressing prevention and patient self-management as well as eschewing expensive hospital care by substituting more efficient modes of care delivery and avoiding unnecessary care. For example, if a patient with a chronic illness such as diabetes regularly undergoes blood tests to check their hemoglobin A1c, some of the more severe conditions associated with out-of-control diabetes (such as skin ulcers, blindness, or amputation) could be avoided. Doing so would substantially decrease the costs to the HMO, which is ultimately responsible for managing care and paying the medical bills.
There are four generally recognized models of HMOs, which vary in design. In the so-called group model, the HMO contracts with a group of physicians for a set fee per patient to provide many different health services in a central location. The group of physicians determines the compensation of each individual physician. In the individual practice association (IPA) model, the HMO contracts with a private practice physician or physician group to provide health care services in return for a negotiated fee. The IPA then contracts with physicians who continue in their existing individual or group practice. In a network model, the HMO contracts with a variety of physician groups and other providers in a network of care with organized referral patterns. In a staff model, the physicians are salaried staff of the HMO and provide care exclusively for the HMO’s population.
HMOs can also be categorized by the constraints they impose on their population. An exclusive provider organization provides benefits only if care is rendered by providers within a specific network, while some HMOs offer point-of-service. These HMOs allow members to receive care from both network providers and out-of-network providers. Typically, there are fewer covered benefits associated with using out-of-network providers. In addition, members usually pay substantially higher out-of-pocket costs when seeking care from out-of-network providers.
HMO models are a mainstay of health care coverage in the United States; these models have evolved over the past decades to meet critical challenges. Their success in meeting these challenges has been mixed. Medicare instituted HMOs in 1985, and the HMO model has been, and remains, a central component of health care coverage in the United States, evolving to meet the criticisms of both its members and the policy community. While several staff model HMOs are healthy and thriving, network models with point-of-care options are now the norm. However, the dual agency involved in both acting as a service provider and acting as an insurer has taken its toll. HMOs must master the key competencies of both health care provider and insurance company. Christenson et al. examined HMO failures from 1981 through 1989, a period of rapid growth in the nascent HMO environment. They reported that HMO failures “. . . increased from one between June 1984 and June 1985 to fifty-three in 1988, while mergers rose from two to forty-five in the same period”. Some considered this to be a shake-out period, where HMOs lacking expertise in both realms exhibited a tendency to underestimate their incurred-but-not-reported claims or overestimate their receivables, often leading to bankruptcy or acquisition. At the same time, these HMOs lacked avenues for subsequent cost savings through cost shifting. Browen et al., in their 1993 paper, concluded that HMOs had not saved money for Medicare even though HMOs were able to reduce hospital days by 16 percent (however, they were not able to reduce hospital admissions).
Beyond the lack of financial success of many Medicare HMOs, there is limited evidence that HMOs have increased quality of care. Miller and Luft reviewed literature on HMO performance from 1997 to 2001 and found that HMOs’ care quality was comparable to that of traditional FFS approaches, while HMOs lowered the use of hospital and other expensive resources. At the same time, HMOs reduced many measures of access to care and were associated with lower levels of enrollee satisfaction than non-HMOs. Quality-of-care research results, however, are particularly heterogeneous, which suggests that quality varies greatly among providers, plans (HMO and non-HMO), and geographic areas. Their conclusion was prophetic: “The consistently mixed quality-of-care results for HMO versus non-HMO plans over the past two decades suggests that for HMOs to meet the vision of their advocates and, as a whole, outperform PPO and indemnity plan quality of care, nothing less than a systematic revamping of health care information systems, incentives, and clinical processes may be required. It remains to be seen whether such a revamping will occur. If it does not, HMOs will likely be but a footnote in the history of U.S. health care.”
ACCOUNTABLE CARE ORGANIZATIONS
The concept of ACOs has existed for 50 years. The birth of ACOs was foreshadowed in 1970 by Paul Ellwood, who coined the term health maintenance organization at the Jackson Hole Group. The influence of the Jackson Hole Group on demand-side health care policy and the evolution and implementation of HMOs in the United States was evident in both the Clinton-era health care reform effort and the Obama-era Affordable Care Act, which institutionalized the development of ACOs. The goal of ACO development was to improve quality of and access to care while holding constant, or reducing, the volume of care. This was to be accomplished through bonus payments for meeting quality targets and lower payments for not meeting the targets. The Medicare Payment Advisory Commission (MedPAC), in their 2009 report to Congress, described an ACO as consisting of “. . . primary care physicians, specialists, and at least one hospital. It could be formed from an integrated delivery system, a physician–hospital organization, or an academic medical center. The defining characteristic of ACOs is that a set of physicians and hospitals accept joint responsibility for the quality of care and the cost of care received by the ACO’s panel of patients.” Two ACO models were described: one in which providers volunteer to form an ACO and one in which participation from providers is mandatory.
In the United States, the design and implementation of ACOs followed several core features. ACOs were implemented as groups of clinicians, hospitals, and other health care providers who came together voluntarily to give coordinated high-quality care to a designated group of patients. Under this arrangement, ACOs first received FFS payments for actual service provided. Patients could also receive care from providers who are not part of the ACOs. At the end of year, ACOs also included bonus payments for upside savings but no penalty for down-side losses (though two-sided risk was eventually introduced). Savings were defined as the estimated average per capita expenditures under the ACO below the applicable benchmark, with adjustment for beneficiary clinical characteristics.
The definition of accountable care used in this policy note encompasses both the older HMO model and the ACO model, which exhibit several similarities. The similarities between HMOs and ACOs include a host of tools currently employed in most integrated or managed care practices. These include, but are not limited to, tools that are identify at-risk individuals using comprehensive data sources; focus on prevention and wellness; establish electronic, searchable patient registries that enable the management of health care services; provide appropriate follow-up; identify gaps in patient care; offer care coordination that focuses on patient and family-centered care; track and coordinate care setting transitions; integrate direct communication between primary care physician (PCP) and care coordinator so they work together to ensure consistency and continuity of care; provide care plans for selected patients with a chronic or complex condition, involving the patient and, if appropriate, the patient’s family; and establish and maintain relationships with community partners to connect patients with needed resources.
Some pivotal differences between HMOs and ACOs also exist. First, HMOs are paid a fixed, per member fee that reflects the actuarial risk of their population. ACOs negotiate a total cost of care (TCOC) for their population for a fixed period of time (typically one year) and a risk-sharing arrangement. Risk sharing can be sharing just the upside risk, splitting any savings from the negotiated TCOC in an agreed upon percentage, or it can entail both upside and downside risk. In this case, the ACO may be accountable for some percentage of any losses (that is, any expenses in excess of the negotiated TCOC). Second, HMOs provide financial disincentives for members to receive their care outside the HMOs’ contracted providers with whom they have negotiated prices. Non-emergency care received from outside the contracted network is typically paid out-of-pocket by the member or requires cost sharing on the part of the member. ACOs are responsible for all covered services regardless of where they are received, and members have no constraints on where they receive care.
Third, HMOs must manage their balance sheet to a monthly payment (their per member per month (PMPM) capitation rate multiplied by the number of members). ACOs accept upside risk (or both upside and downside risk) for their FFS costs below (or above for downside risk) relative to a benchmark. Medicare currently uses risk-adjusted, projected FFS cost and a quality benchmark based on 23 quality measures spanning four quality domains: patient/caregiver experience, care coordination/patient safety, preventive care, and at-risk population management. As ACOs get paid through FFS, they accumulate revenue on a continuous basis, and those in the Basic Track (one-sided risk model) can earn up to 10 percent of savings and be held accountable for up to 4 percent on losses.
Fourth, back-office costs (accounting, financial functions, enrollment tracking and verification, and so on) for HMOs are higher than they are for ACOs.
With those caveats in mind, the application of the ACO model could be quite useful for health care delivery systems facing increasing utilization, cost, and access disparities. Indeed, many countries with social insurance programs tied, directly or indirectly, to care delivery have been using a population-based approach to health care provision—a primary feature of ACOs as well as the managed care insurance models of the 1970s and 1980s in the US.
ACOs have been shown to obtain modest reductions in costs. This is primarily due to reductions in the use of facility-based outpatient services, which is an arrangement specific to the US health care system. ACOs have seen evidence of modest cost savings, which are largely attributable to savings in outpatient expenses among medically complex patients and reductions in the delivery of low-value services. Most of the experience with ACOs comes from the US experience. There are two limitations to extrapolating the US experience: ACOs are paid on an FFS basis rather than on an insurance basis (as is the case of relationships based on fixed budgets or capitated payments); and the United States implemented the voluntary form of ACOs (for both patients and providers), which limits generalizability to single-payer systems.
ACOs have also been shown to reduce the utilization of certain types of health care services and improve the prevention and management of chronic diseases. To date, the most consistent associations between ACO implementation and ACO outcomes across payer types are reduced inpatient use, reduced emergency department visits, and improved measures of preventive care and chronic disease management. ACO models met most quality measures, performing better than their FFS counterparts.
ADVANCED PRIMARY CARE
Advanced Primary Care—a program within the Centers for Medicare & Medicaid Services (CMS)—aims to reduce total cost of care by increasing patient access to primary care. It is sometimes referred to as a Primary Care Medical Home (PCMH), which was the first iteration of CMS’s Advanced Primary Care program. PCMHs include a full range of primary care providers, specialized physicians, nurse practitioners, and advanced-practice nurses, all with the goals of improving quality of care and patient satisfaction and reducing expenditures by increasing patient access to advanced primary care services. PCMHs also incorporate non-traditional modes of primary care service delivery, including remote clinics, mobile clinics, and telehealth. PCMHs leverage electronic health records (EHRs) to develop disease/condition registries and individual patient risk profiles. They facilitate access to and integration of specialty care services and heavily invest in case management to enhance care coordination.
CMS has modified the PCMH model under its Advanced Primary Care program to now use the Primary Care First (PCF) model. PCF focuses on five primary care functions: access and continuity; care management; comprehensiveness and coordination; patient and caregiver engagement; and planned care and population health. Under an Advance Primary Care model, patients are assigned to a PCF based on their geography. Patients can either select a primary care practice or, absent from that, be assigned to the primary care practice whom they saw most in the last two years. Under an Advanced Primary Care program, the PCF providers are paid through three revenue streams. The first revenue stream is the Professional Population-Based payment, which is a lump sum per beneficiary per month (PBPM) payment based on the practice’s risk group. The practice’s risk is calculated using the Hierarchical Condition Category (HCC) risk adjuster. The average risk for the practice’s patients places the practice into one of four risk categories. This per-member-per-month payment increases as risk levels increase. The second revenue stream is the Flat Primary Care Visit Fee, which is a flat fee for primary care face-to-face encounters that is lower than the FFS payment for a face-to-face encounter. The underlying logic of this revenue stream is to balance the incentive to avoid face-to-face encounters engendered by capitated payments and the need to provide patient-centered care through face-to-face encounters. The third revenue stream is a quarterly performance-based adjustment to total revenue. This is defined as the total Professional Population-Based payment plus the Flat Primary Care Visit Fee. The adjustment is based on the practice’s ability to reduce costs and improve quality. The performance-based adjustment provides an upside of up to 50 percent, as well as a downside of up to 10 percent, of quarterly payments to the practice.
There are similarities and differences between the PCF model and the HMO and ACO models. Similarities between all three models include the host of tools currently employed by both ACOs and HMOs mentioned above. Like ACOs and HMOs, PCF also has a defined population for whom they are responsible for a fixed period of time. Beyond those elements, the PCF model selectively borrows components from the ACO and HMO models.
The inclusion of a PMPM capitated up-front payment harkens to the HMO model, which provides more cash on hand. This allows the practice some flexibility in budgeting, withstanding unexpected costs, and simplifying billing. Like ACOs, PCF bills FFS for face-to-face encounters, thus increasing access to appropriate care, increasing patient satisfaction, and providing a springboard for higher-quality care. Furthermore, like ACOs, PCF providers accept upside and downside risk based on performance. But there are also several nuanced differences. ACOs are paid through FFS with annual adjustments to total payment linked to performance. HMOs’ payments are capitated. PCF providers are paid both through FFS and capitated payments, and their performance adjustments are made quarterly rather than annually. ACOs and HMOs are responsible for all covered services. Under the PCF model, practices are responsible only for primary care services (though performance adjustments include non–primary care services). ACO and HMO membership is voluntary. PCF membership is both voluntary and assigned based on previous patterns of care. The PCF model is just now being implemented, and thus little is known about its efficacy or effectiveness at this time.
Discussion
Based on the experience with implementation and performance of accountable care models, five critical elements for success can be distilled. These are discussed below. The first three critical elements are within the control of the accountable care practice. The final two are policy issues external to the organization and require the attention of the governing body.
ACOs require strong organizational alignment in culture and operations to drive performance and achieve their overarching goals. Hilligoss et al. performed qualitative case studies of four ACOs over a two-year period. While they concluded that organization within an ACO is an ongoing process, they also noted similarities between all four organizations. Perhaps most important was their identification of cognitive (for example, understandings and attention) and cultural (for example, trust and values) levels of alignment; this is in addition to operational levels of alignment (such as organizational structures, processes, and incentives). They label these cooperative alignment (the “alignment of interests, goals, or rewards”), to enable the will to work together, and coordinative alignment (the “alignment of actions or operations” or the “ability to work together”).
Forming partnerships to maximize resource interdependencies and collaboration among providers is critical. Partnership scope refers to the resource interdependencies and collaboration among providers across the care continuum. In ACOs and HMOs, in particular, the need to access additional capabilities—such as adding post-acute care to an organization that currently has primary care and hospital services resources—is common in the early development of the organization and is most often obtained through partnerships. Increasing scope results in more services and care activities being provided by the organization. This, in turn, results in increasing the partners’ shared knowledge. This typically results in improved patient care management with providers playing a more active role in collaborating across the patient journey.
Partnership scale refers to the extent of resource interdependence and collaboration necessary to deliver high-quality care. Lan et al. argue that there is “a diminishing return from increasing partnership scale. In other words, increasing the number of same-stage providers benefits ACO performance, but, at a certain point, these benefits grow progressively incremental.”
ACOs and HMOs need well-developed information technology (IT) systems and data structures. ACOs have greater health IT capabilities, on average, than non-ACO organizations. This is reflected in the findings from a national survey of providers from 2015 in which 92 percent of physicians in an ACO reported using a certified EHR, while this number was only 68 percent in physicians not participating in ACOs. While EHRs are an essential component of any accountable care entity, they are not the only information system necessary for success.
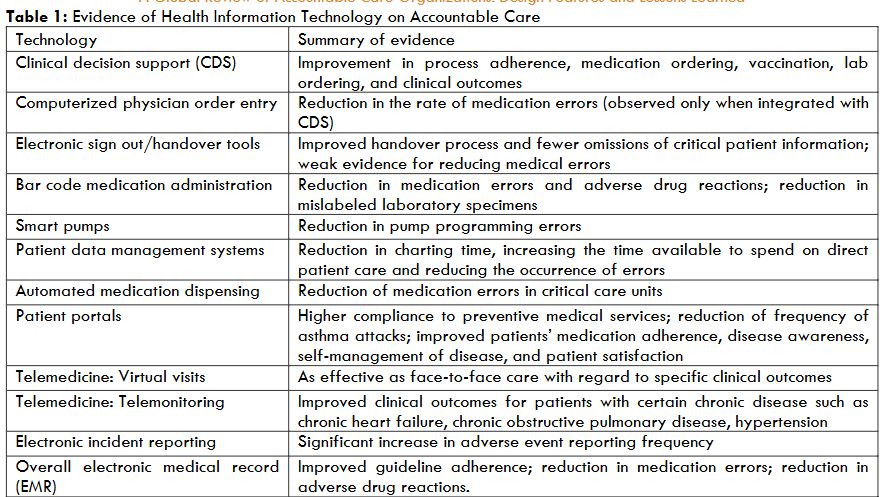
Health information management (HIM) and health care information technology (HIT) have been shown to be essential (if not the most essential) building blocks in any effort to achieve accountable care. HIM and HIT allow organizations to avoid medical errors, use resources more efficiently, accelerate the diffusion of knowledge, implement evidence-based care (by reducing the variability of care), advance the consumer’s role in health care (through patent portals), promote public health and preparedness, and strengthen patient privacy. HIM is traditionally defined as the collection, analysis, storage, and protection of quality patient health information, while HIT has been defined as “the application of information processing involving both computer hardware and software that deals with the storage, retrieval, sharing, and use of health care information, data, and knowledge for communication and decision making.” Alotaibi and Federico detailed the effectiveness of these approaches in their review of the literature, which are adapted and shown in Table 1. Absent an adequate, well-articulated, well-maintained information system with an emphasis on training in HIM, an organization will not be able to implement the more nuanced aspects of an accountable care model.
Adequate risk adjustment is also critical for the success of ACOs. Risk adjustment is improving but it still does not adequately level the playing field. The long-term financial sustainability of ACOs require a deeper comprehension of the risk characteristics of the population for which they are accountable. Community rating of risk is a viable alternative for setting prices for organizations with sizable enrollment. However, many implementations employ experience rating to determine prices.
Health care costs for an individual are composed of two components: a stochastic component and a deterministic component. Appropriate risk adjustment of payment to reflect the health risk and associated resource requirements is essential for equitable health financing and the financial resilience of ACOs. The stochastic component is an insurable event and can be priced using traditional insurance approaches. However, the deterministic component is dependent on several externalities. We only have data on a few of these externalities, which explain only about 20 percent of the health care cost. The remaining 80 or so percent cannot be foreseen by either the individual or an accountable care practice because they are random. Numerous studies have demonstrated that costs are non-linear and higher costs lead to higher heteroscedasticity. Thus, a patient’s underlying risk increases while the adequacy of the payment for that patient is less precise and generally underestimates their true risk, resulting in underpayment for higher-risk patients. This puts the organization with higher-than-average risk at a severe disadvantage.
Numerous studies have evaluated health risk assessment models. In the 1980s, Duan et al. demonstrated that the maximum percentage that one should expect to explain the deterministic component is about 20 percent; McCall and Wai estimated it to be 14 percent. In 2007, the Society of Actuaries commissioned a study entitled A Comparative Analysis of Claims-Based Tools for Health Risk Assessment, which examined the performance of common risk adjustment tools including ACG, CDPS, 3M’s Clinical Risk Groups, three versions of the Dx3G, MedicaidRx, Ingenix’s ImpactPro and Ingenix ERG. They found the proportion of variance of health care costs explained by these to be between 14.9 percent and 27.4 percent.
Implementing appropriate performance benchmarks to motivate high-performing ACOs is imperative for the transformation of the health system. For ACOs, becoming more efficient is a non-linear process with a ceiling effect. How much better can high-performing organizations become? Reimbursement policies that require a percentage increase in quality or decrease in utilization and/or cost put high-performing organizations at a disadvantage. But so do benchmark approaches. Bleser et al. reported that a $1,000 decrease in per capita benchmark was associated with a 25 percent increased risk of the ACO exiting the ACO market. ACOs with higher Hierarchical Condition Categories medical risk scores (sicker patients) also had shorter survival in the Medicare Shared Savings Program. These risk scores are used to adjust payments back to the ACO. One existing concern is that the current Hierarchical Condition Categories risk-adjustment system does not adequately account for very sick or frail patients; that is, it underpays ACOs. Likewise, benchmarks based on an ACO’s past performance also can lead to perverse incentives. One solution, suggested by Douven et al. (2015), is to employ what they call yardstick competition. Yardstick competition could take many forms. One form would be to use both an ACO’s current performance and that of other ACOs in the market. A second, more straightforward approach would be to compare the performance of the ACO with the overall performance of all ACOs in the market. This approach would result in more efficient ACOs realizing savings more easily.
Conclusions
This policy note reviewed the global experience with developing accountable care systems, aiming to distill some of the key findings and lessons that may be of use to architects of health system reform. In order to shed light on the benefits and effectiveness of ACOs and identify critical elements for the success of ACOs, the policy note provided a comprehensive scoping review of the relevant literature to date on the application of the accountable care design on a global scale in terms of effectiveness and generalizability for broader application.
Acknowledgements
This paper was produced by the Saudi Health Council (SHC), with technical support from the World Bank (WB). The authors are grateful for the support provided by Nahar Alazemi (Secretary General, Saudi Health Council), Taghred Alghaith (Saudi Health Council), Rekha Menon (Practice Manager, Health Nutrition and Population, Middle East and North Africa region, World Bank) and Issam Abousleiman (Country Director, Gulf Cooperation Council countries, World Bank). The findings, interpretations, and conclusions expressed in this work are those of the authors, and do not necessarily reflect the views of the Saudi Health Council or the World Bank, their Boards of Directors, or the governments they represent.
Funding
Financing was provided by the Saudi Health Council and the Saudi Ministry of Finance under the Health, Nutrition and Population Reimbursable Advisory Services Program (P172148) between the World Bank and the Saudi Health Council.
Declarations, and Ethics and Consent statement
Our study did not require an ethical board approval because we completed a review of existing literature.
References
- Armitage GD, Suter E, Oelke ND, Adair C. Health systems integration: state of the evidence. International Journal of Integrated Care. 2009 June 17; Vol. 9.
- Europe, RAND and Ernst & Young LLP. National Evaluation of the DH Integrated Care Pilots. Santa Monica, CA: RAND Corporation, 2012. 131 p.
- World Health Organization. Integrated care models: an overview. Europe: World Health Organization, 2016. 41 p.
- McClellan M, Kent J, Beales SJ, Cohen SIA, Macdonnell M, Thoumi A, Abdulmalik M, Darzi A. Accountable Care Around the World: A Framework to Guide Reform Strategies. Health Aff. 2014 September; Vol. 33, No. 9.
- Gruber LR, Shadle M, Polich CL. From movement to industry: the growth of HMOs. Health Aff (Millwood). 1988 Summer;7(3):197-208.
- Morrison EM, Luft HS. Health maintenance organization environments in the 1980s and beyond. Health Care Finance Rev. 1990 Fall;12(1):81-90.
- Brook RH. Ensuring Delivery of Necessary Care in the United States: Testimony Presented to the Senate Committee on Health, Education, Labor, and Pensions. Santa Monica, CA: RAND Corporation, 1999. 16 p. https://www.rand.org/content/dam/rand/pubs/testimonies/2006/CT152.pdf
- Christenson JB, Wholey DR, Sanchez SM. State Responses to HMO Failures. United States: The People to People Health Foundation, Inc., Project HOPE Health Affairs, 1991. Vol.10 (4), p.78-92.
- Browen RS, Clement DG, Hill JW, Retchin SM, Bergeron JW. Do health maintenance organizations work for Medicare?. Health Care Finance Rev. 1993;15(1):7-23.
- Miller RH, Luft HS. HMO Plan Performance Update: An Analysis of The Literature, 1997-2001. Bethesda: Health Affairs, 2002-07-01, Vol.21 (4), p.63-86.
- Ellwood Jr. PM, Anderson NN, Billings JE, Carlson RJ, Hoagberg EJ, McClure W. Health Maintenance Strategy. Medical Care. Lippincott Williams & Wilkins. 1971 May-June; 8 (3): 291-298.
- MedPAC June 2009 Report to the Congress: Improving Incentives in the Medicare Program: Chapter 2.
- Impact of Provider Participation in ACO Programs on Preventive Care Services, Patient Experiences, and Health Care Expenditures in US Adults Aged 18–64. Medical Care. 2018 August; Volume 56, Number 8.
- Wilson M, Guta A, Waddell K, Lavis J, Reid R, Evans C. The impacts of accountable care organizations on patient experience, health outcomes and costs: a rapid review. Journal of Health Services Research & Policy. 2020; Vol. 25(2) 130–138.
- Williams JM, Chen AJ. Understanding The Latest ACO “Savings”: Curb Your Enthusiasm and Sharpen Your Pencils—Part 1. Health Affairs. 2020 November 12.
- CMS. Primary Care First Model Options. Baltimore, MD: U.S. Centers for Medicare & Medicaid Services; 2021 March 26. Available from: https://innovation.cms.gov/innovation-models/primary-care-first-model-options.
- Hilligoss B, Song PH, McAlearney AS. Aligning for accountable care: Strategic practices for change in accountable care organizations. Philadelphia: Lippincott Williams & Wilkins. Health care management review. 2017; Vol.42 (3), p.192-202.
- Shortell S, Gillies R, Anderson D, Mitchell J, Morgan K. Creating organized delivery systems—the barriers and facilitators. Hospital Health Services Admin. 1993; 38(4):447–466.
- De Block C, Meijboom B, Luijkx K, Schols J, Schroeder R. Interfaces in service modularity: A typology developed in modular health care provision. Journal of Operations Management. 2014; Volume 32, Issue 4.
- Lewis VA, Tierney KI, Colla CH, Shortell SM. The new frontier of strategic alliances in health care: new partnerships under accountable care organizations. Soc Sci Med. 2017; 190:1-10. doi:10.1016/j.socscimed.2017.04.054.
- Oxley JE, Sampson RC. The scope and governance of international R&D alliances. Strategic Management. 2004 J; 25(8-9): 723–749.
- Lan Y, Chandrasekaran A, Goradia D, Walker D. Collaboration Structures in Integrated Healthcare Delivery Systems: An Exploratory Study of Accountable Care Organizations. Manufacturing & Service Operations Management [Internet]. 2022 Jan [cited 2022]; 0, 0. Available from https://pubsonline.informs.org/doi/10.1287/msom.2021.1038.
- Electronic Health Record Use among Physicians Participating in Delivery Reform Programs [Internet]. Office of the National Coordinator for Health Information Technology. 2016 [cited 2018 Dec 15]. Available from: https://dashboard.healthit.gov/quickstats/pages/FIG-EHR-Use-Physicians-Participating-Delivery-Reform.php.
- Brailer JD. The Decade of Health Information Technology: Delivering Consumer-centric and Information-rich Health Care. US Department of Health and Human Services. July 2004.
- Alotaibi YK. Federico F. The impact of health information technology on patient safety. Saudi Med. 2017 J; Vol. 38 (12).
- Veazie PJ, Manning WG. Improving Risk-Adjustment for Medicare Capitated Reimbursement Using Nonlinear Models. Medical Care. 2003 July; 41(6):741-52.
- Duan N, Manning WG, Morris C, Newhouse JP. A comparison of alternative models of the demand for medical care. Santa Monica, CA: Rand; 1982. Report no. R-2754- HHS.
- McCall N, Wai HS: An analysis of the use of Medicare services by the continuously enrolled aged. Medical Care. 1983 June; 21(6):567-585.
- Winkelman R, Mehmud S, Wachenheim L. A Comparative Analysis of Claims-Based Tools for Health Risk Assessment. United States: Society of Actuaries; 2007 April 20. 70 p.
- Bleser W, Muhlestein D, Saunders R, McClellan M. Half a decade in, Medicare accountable care organizations are generating net savings: part 1. Health Affairs [blog on the Internet]. 2018 Sep 20 [cited 2019 Mar 5]. Available from: https://www.healthaffairs.org/do/10.1377/hblog20180918.957502/full/
- Douven R, McGuire TG, McWilliams JM. Avoiding Unintended Incentives in ACO Payment Models. Health Affairs. 2015 Jan; 34 (1).
- Bleser WK, Saunders RS, Muhlestein DB, McClellan M. Why do accountable care organizations leave the Medicare shared savings program? United States: The People to People Health Foundation, Inc., Project HOPE, Health Affairs. 2019 May, Vol.38 (5), p.794-803.

