Leveraging Telementorship to Enhance Emergency Care in Uganda
Bridging Uganda’s Emergency Care Skills Gap: Leveraging Virtual Telementorship for Frontline Providers
Andrew Twineamatsiko, Brian Agaba, Martin Msukwa, Bassim Birkland, Geofrey Ssekalembe, Jimmy Atyera, Prossy Nakattudde, John Baptist Nambohe Waniaye, Irene Atuhairwe
Seed Global Health, Ministry of Health
OPEN ACCESS
PUBLISHED 30 September 2025
CITATION Twineamatsiko, A., Agaba, B., et al., 2025. Bridging Uganda’s Emergency Care Skills Gap: Leveraging Virtual Telementorship for Frontline Providers. Medical Research Archives, [online] 13(9). https://doi.org/10.18103/mra.v13i9.6838
COPYRIGHT © 2025 European Society of Medicine. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
DOI https://doi.org/10.18103/mra.v13i9.6838
ISSN 2375-1924
Abstract
Background: Emergency care conditions, including trauma, acute infections, and obstetric emergencies, significantly contribute to global mortality and morbidity, disproportionately affecting low- and middle-income countries. Uganda, with a predominantly young and rural population of over 46 million, faces a severe shortage of trained emergency care providers, exacerbating mortality rates in emergency units.
Aim: This study aimed to evaluate the Extension for Community Healthcare Outcomes model adopted by Uganda’s Ministry of Health and Seed Global Health in 2021 to bridge the emergency care skills gap among frontline health workers.
Methods: A retrospective program evaluation was conducted using secondary quantitative data analysis covering September 2021 to December 2024 period. Data from participant registrations and pre/post knowledge tests via Zoom sessions were analyzed using Microsoft Excel and Power BI.
Results: Between September 2021 and December 2024, 70 bi-weekly telementorship sessions were conducted to 11,805 participants across all 146 Ugandan districts and 66 additional countries with majority coming from East Africa. Participants included general doctors (38%), nurses and midwives (28%), allied health professionals (27%), specialists (4%), and emergency medical technicians (3%). High repeat participation rates and an average attendance duration of 205.5 minutes per session indicated substantial engagement and perceived program value. Immediate knowledge gains were demonstrated through significant improvements in pre- and post-session assessments from 36% to 65%.
Conclusion: The findings highlight the effectiveness and scalability of virtual telementorship in rapidly enhancing emergency care competencies among diverse health professional cadres. The broad geographical and facility-level reach underscores its potential for bridging critical workforce gaps in resource-limited settings. However, the study noted limitations, including potential participation bias and the absence of long-term knowledge retention and patient outcome assessments. Policy recommendations emphasize integrating virtual telementorship into national workforce development strategies, advocating for dedicated funding and infrastructure support to sustain and expand this impactful approach. This initiative demonstrates a feasible and scalable model for improving emergency care knowledge, with strong potential for replication in similar global health contexts.
Keywords
Emergency care, telementorship, Uganda, healthcare workforce, virtual training
Introduction
Emergency care conditions ranging from trauma, injuries, obstetric and acute infections are the leading cause of mortality and morbidity globally. This is worse for the low and middle income countries.
Building a robust, responsive and competent emergency care systems in Low- and middle-income countries would avert over 24 million deaths and 1 billion disability-adjusted life-years (DALYs) annually. A well-performing health workforce is the core of functional health systems and is not only essential but necessary and play a critical role in improving outcomes for the patients. This also necessitates a health workforce that is competent with required knowledge, experience and skills to handle various emergencies.
The global health workforce shortage with a projected gap of 18 million health workers across all clinical departments will not only hinder progress to attaining Universal Health Coverage but as well slow progress towards reduction of mortality and morbidity due to emergencies much worsened by global pandemics like COVID-19. The low- and middle-income countries are still the most hit yet have the highest burden of disease and emergencies. This severely undermines progress toward national health indicators, targets, and Sustainable Development Goals (SDGs), compromising healthcare access, quality, and outcomes. Therefore, strengthening the skills of the limited healthcare workforce is crucial to reducing preventable deaths and disabilities.
Uganda currently with a population of over 46 million people and mostly predominantly young and rural faces high rates of traumatic injuries attributed to accidents as well as critical conditions and obstetric emergencies. The health system faces significant gaps, including a shortage of trained emergency care providers and limited access to specialist support. The assessment conducted by the Ministry of Health and Seed Global Health showed that only 22.6% of the health workers were trained on Emergency triage assessment and treatment and 36.3% trained on Basic Emergency Care. The country also has one of the youngest emergency care training programs in the region with recent accredited courses for Emergency medical technicians and emergency physicians.
Most patients with acute conditions first present to lower-level facilities staffed by healthcare workers, who often lack knowledge, skills and confidence in managing life-threatening scenarios such as severe trauma, acute respiratory distress, and obstetric hemorrhage along with other obstetric complications. The disparity between need and capacity causes critical delays in emergency care, contributing to poor outcomes, with 18% of patients dying within 24 hours of admission to emergency units. The World Health Organization emphasizes the need for innovative workforce development such as telehealth strategies to bridge gaps in pre-hospital care, particularly in rural and peri-urban areas under low resource settings. One of such is the Extension for Community Healthcare Outcomes (ECHO) model, a telementorship model which offers a scalable approach to upskill frontline providers through regular, case-based, expert-led virtual sessions. It was first developed to improve access to care for underserved populations with complex health problems such as hepatitis C virus (HCV) infection.
In 2021, Uganda’s Ministry of Health and Seed Global Health launched an Emergency Medical Services ECHO program, aimed at equipping frontline healthcare workers with essential emergency care skills to improve patient outcomes. This telementorship program connects frontline providers with emergency medicine experts via videoconferencing, case-based learning, and interactive sessions. Evaluations show significant improvements in providers’ knowledge and skills, a sense of community, and reduced professional isolation (66%). Notably, it achieves this using existing internet connectivity and low-cost platforms.
This article examines the progress, outcomes, and impact of the EMS ECHO program since its launch in 2021, highlighting policy implications and recommendations for scaling health workforce capacity in resource-limited settings like Uganda.
Methods
STUDY DESIGN
We conducted a retrospective program evaluation using secondary quantitative data analysis to assess the impact of the EMS ECHO tele-mentorship program from its inception in September 2021 through December 2024.
SETTING AND PROGRAM DESCRIPTION
The EMS ECHO Uganda initiative operates a “hub-and-spoke†model. A central “hub†of emergency medicine specialists at Seed Global Health, Uganda delivered bi-weekly virtual mentorship sessions via Zoom to “spoke†participants mainly health workers across Uganda’s health system levels and global participation. The curriculum was adapted from the African Federation of Emergency Medicine (AFEM) handbook and experts for each session are selected from the health facilities within Uganda. Each session lasted approximately two hours and included:
- A brief introduction and housekeeping updates
- A case-based discussion
- An expert-led didactic presentation
- Interactive Q&A and summary of key learning points
PARTICIPANTS
All health workers who registered for EMS ECHO sessions during the evaluation period were included. No additional inclusion or exclusion criteria were applied beyond attendance. Registration captured:
- Cadre/Professional role
- Gender
- Health facility level
- District of practice
- Country of practice
Participants could join individually or as part of a group using one device; however, only registered individual logins were captured in the dataset.
DATA SOURCES AND VARIABLES
Data were extracted from Zoom registration records, attendance reports, and pre/post-session knowledge assessments administered via the Zoom polling function. The dataset included: Attendance counts and frequency per participant, geographical distribution by district and country, facility level and cadre, pre-and post-test scores for knowledge gain analysis.
DATA MANAGEMENT AND ANALYSIS
Data were downloaded from Zoom, exported to Microsoft Excel, cleaned for duplicates, and analyzed in Excel and Microsoft Power BI. Descriptive statistics: Counts, percentages, means ± standard deviation (SD), and medians with interquartile ranges (IQR) were used. Knowledge gain analysis: Paired-sample t-tests (p < 0.05 considered significant) compared pre- and post-test scores for participants who completed both assessments. Visual presentation: Tables and charts were produced in Microsoft Excel and Power BI to illustrate trends, cadre distribution, and geographic reach.
ETHICAL CONSIDERATIONS
All data used was secondary and extracted from the previous participant registrations for the sessions. It was de-identified before being exported for analysis. This review did not require ethical approval as it only required review of previous program data from registrations. No interviews with patients or health workers were conducted.
Results
SESSION IMPLEMENTATION
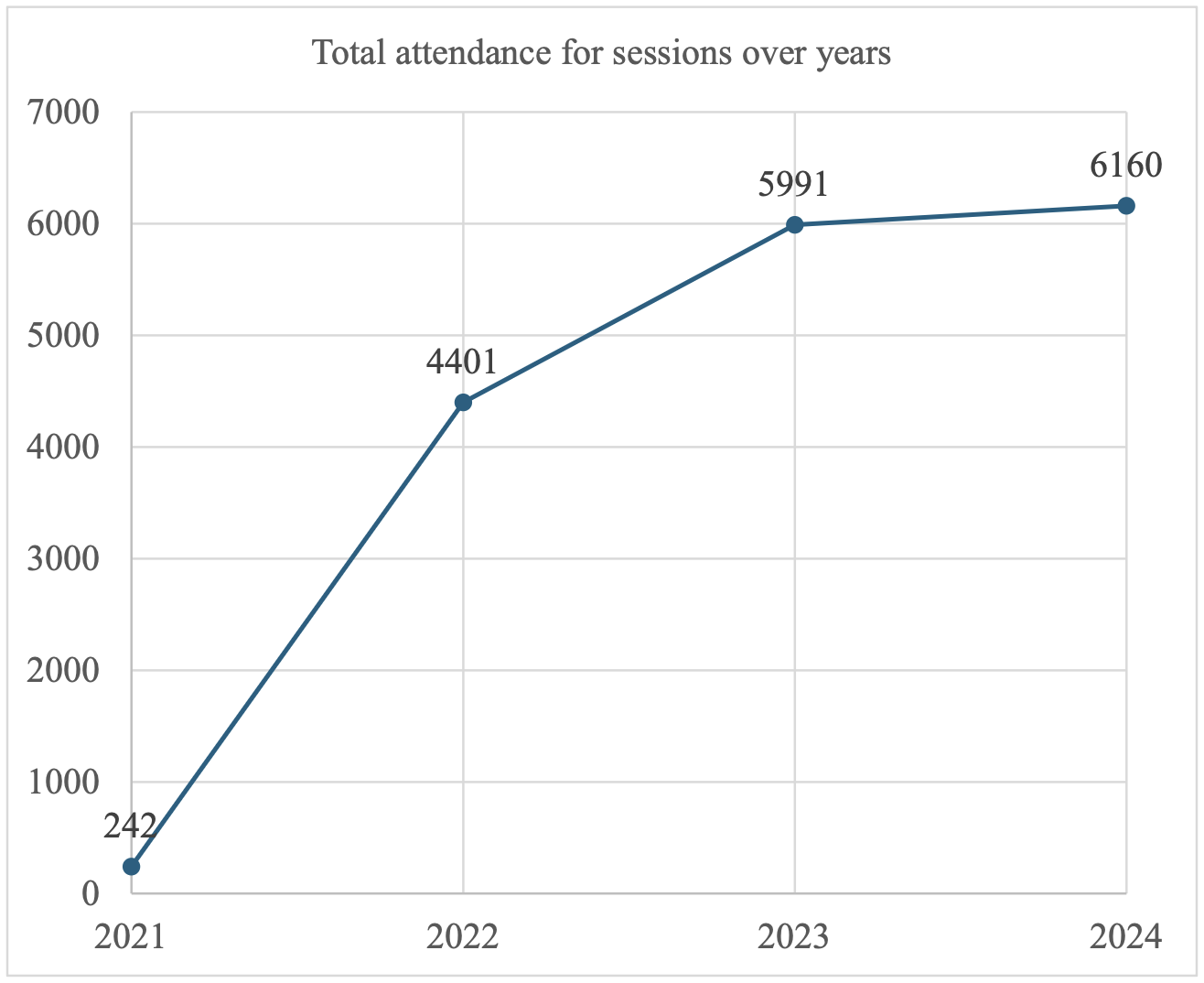
Between September 2021 and December 2024, the EMS ECHO Uganda program delivered a total of 70 tele-mentorship sessions using the “hub-and-spoke” model as indicated in Table 1 below. Sessions were offered on a bi-weekly basis and organized into six progressive phases (0-5). Early phases focused on foundational topics such as governance, airway management, and shock recognition while later modules addressed practical emergency response skills, including trauma care, obstetric emergencies, pediatric resuscitation, and advanced airway techniques as adopted from AFEM handbook.
| Year | Total |
|---|---|
| 2021 | 1 |
| 2022 | 21 |
| 2023 | 25 |
| 2024 | 23 |
| Total | 70 |
Note: EMS ECHO = Emergency Medical Services Extension for Community Healthcare Outcomes. Data source: EMS ECHO program database, 2021-2024.
PARTICIPANT CHARACTERISTICS
Professional cadre: A total of 11,805 individual attendees were recorded across all sessions. As illustrated in Figure 1, participants represented five professional groups: General doctors (38%), Nurses and midwives (28%), clinical officers (27%), Specialists (4%) and Emergency medical technicians (3%) as indicated in figure 1 below. This balanced mix ensured that both frontline and specialist providers could share perspectives and learn from one another, strengthening inter-professional collaboration in emergency care.

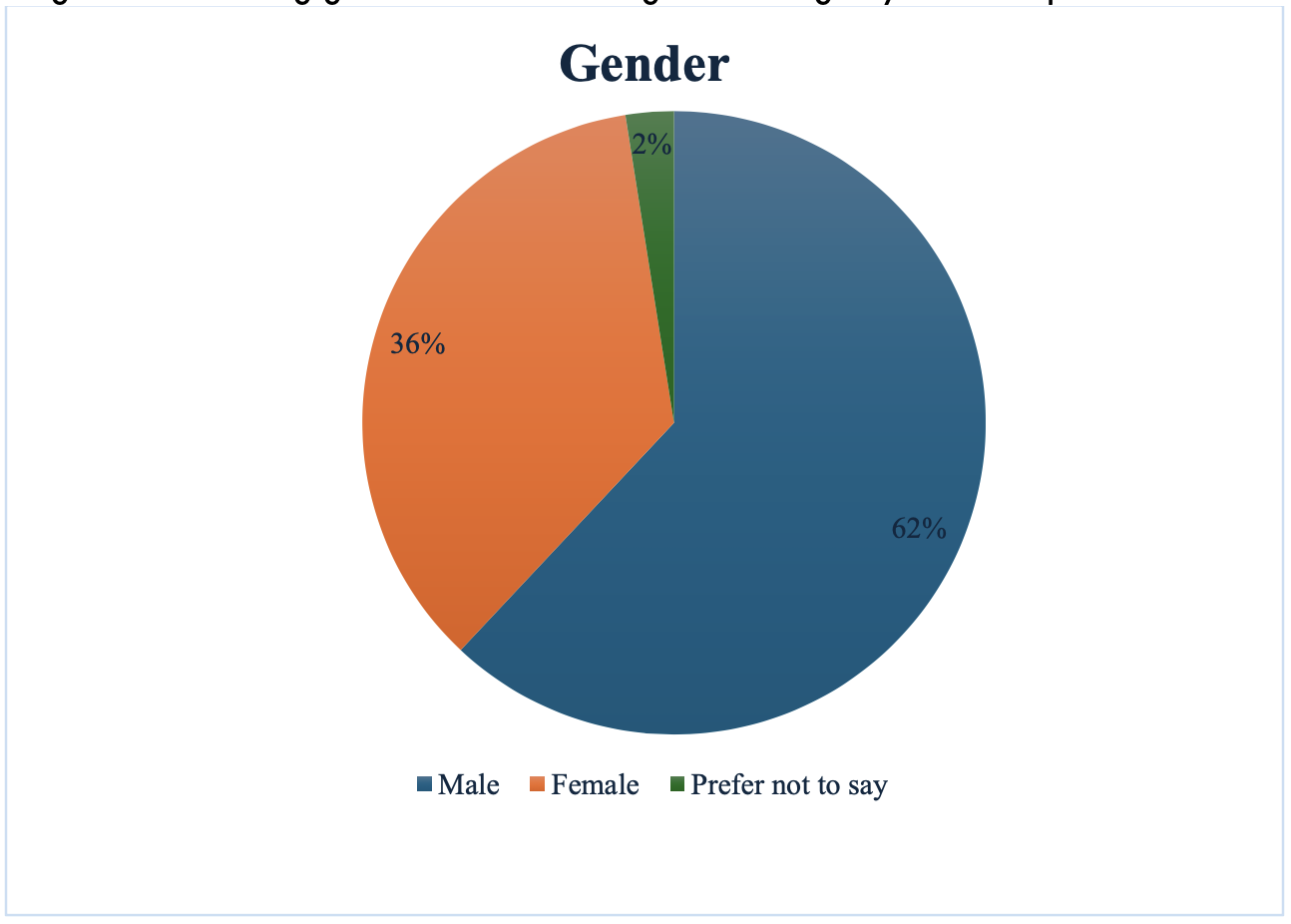
GENDER DISTRIBUTION
Both male (62%) and female (36%) health workers actively participated throughout all phases, contributing diverse insights and fostering gender-inclusive dialogue in emergency medicine practice as shown in figure below.
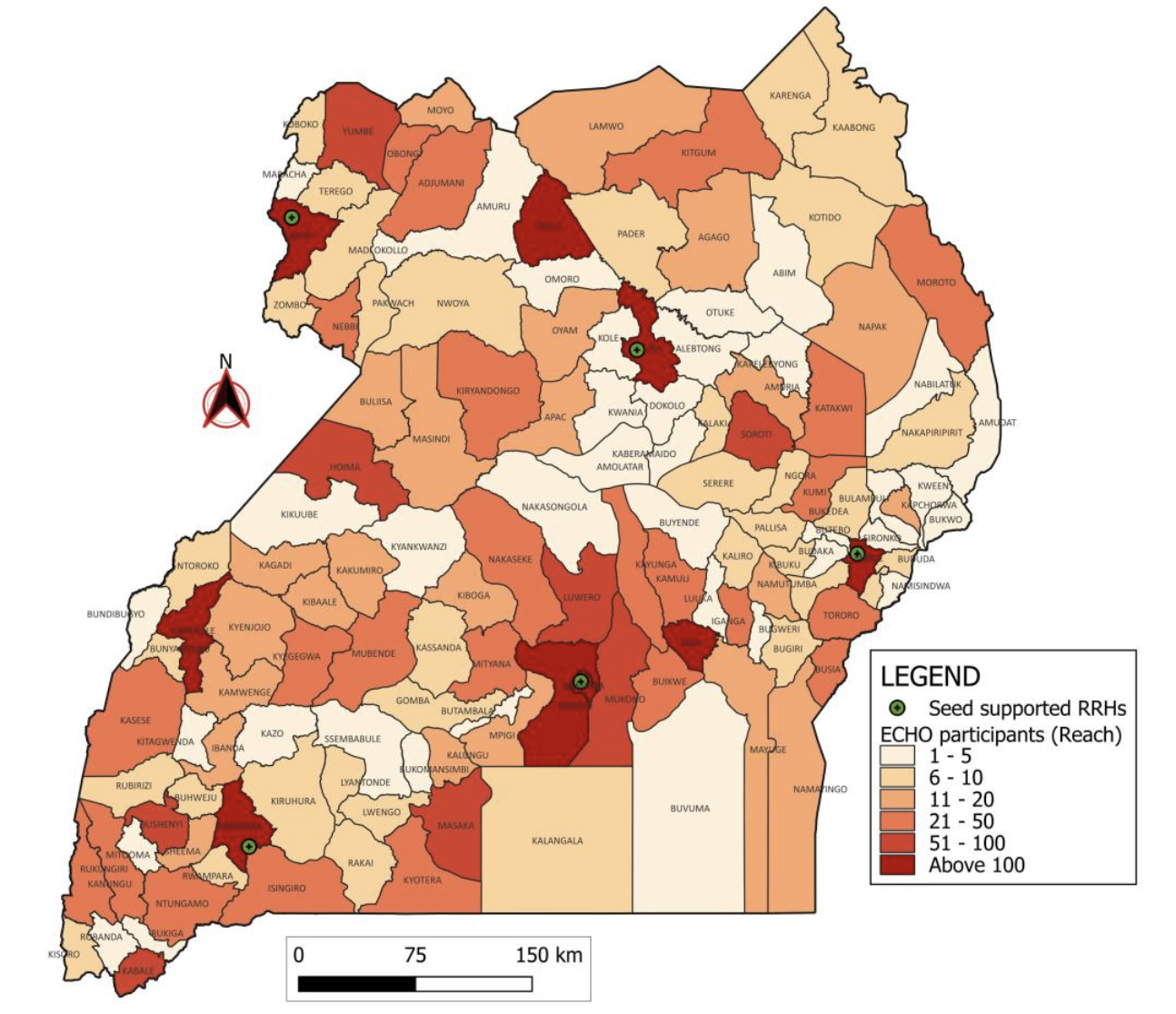
GEOGRAPHIC COVERAGE
Health workers from all 146 districts of Uganda attended at least one session, demonstrating genuine nationwide coverage and the ability of the virtual ECHO platform to bridge geographical barriers as shown in figure 3 below. Additionally, participants from 66 countries mostly from East and Central Africa logged into various sessions; these are spread across all continents.
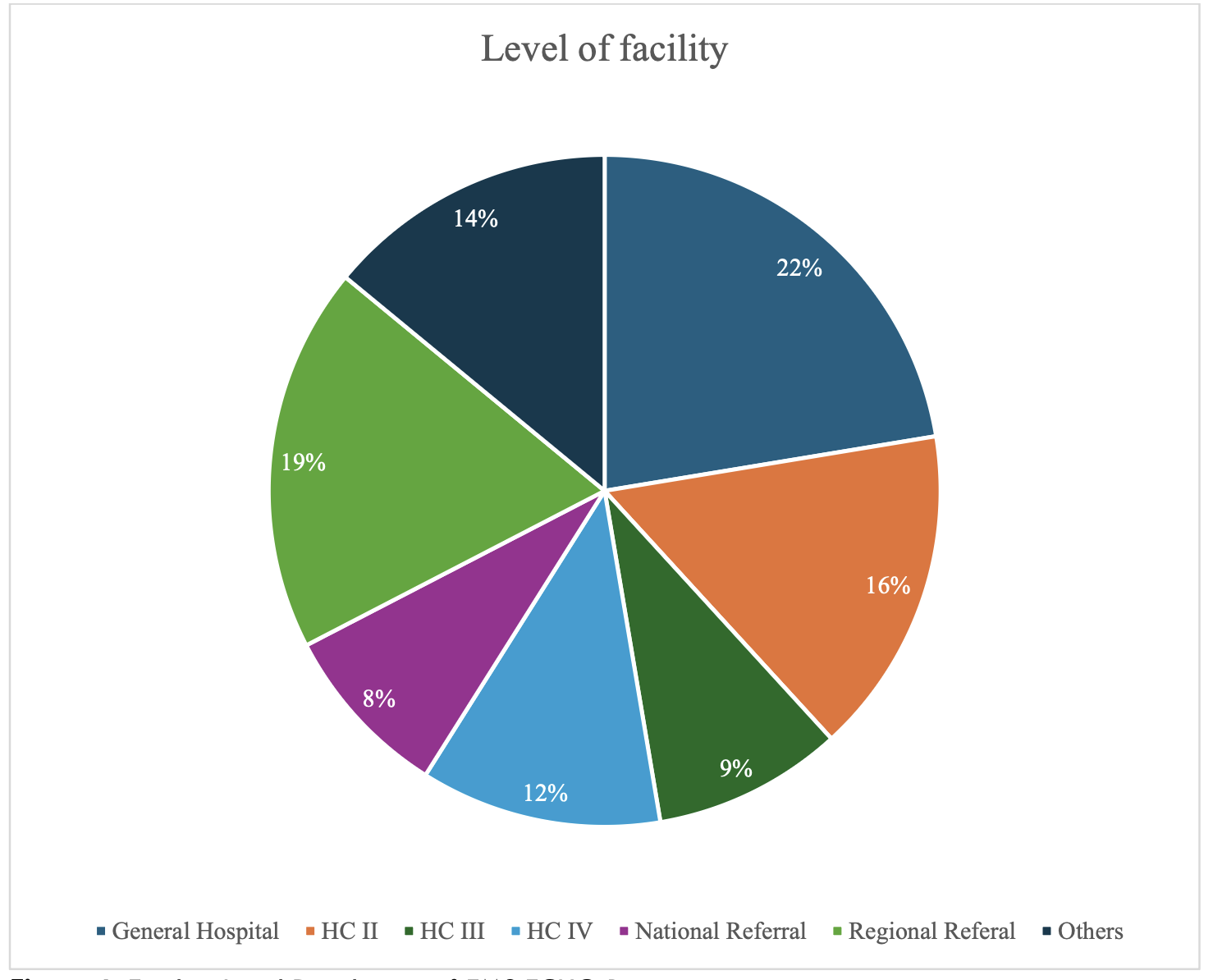
FACILITY-LEVEL REACH
Participants came from across the health system hierarchy in Uganda, from the Health Center IIs that are entry into the health system up to National referral hospitals that provide specialized care. This broad inclusion ensured that capacity building ensured engagement across primary, secondary, and tertiary care settings. Figure 4 below shows that majority of the participants (22%) were from General hospitals, a level of care that also serves as the main referral point for majority of the patients in Uganda.
KNOWLEDGE GAIN
There was a significant immediate knowledge gain (P=0.000) from an average score of 36% in pre-tests assessment to 65% in the post tests done across the sessions done among the participants that did both tests.
ENGAGEMENT AND RETENTION
Repeat participation: Approximately 400 unique participants attended more than 20 sessions each, underscoring strong individual commitment to continuous learning and the perceived value of the ECHO curriculum.
AVERAGE DURATION PER PARTICIPATION: Across all sessions, learners spent a cumulative 2,623,676 minutes in live tele-mentorship, with an average attendance duration of 205.5 minutes per session well beyond the scheduled two-hour meetings indicating high engagement with didactic presentations and case discussions.
ATTENDANCE TRENDS: Growth over time: From a single pilot session in late 2021, the program rapidly scaled to over 20 sessions annually in 2022 and 2023, maintaining this intensity through 2024. This sustained delivery reflects both logistical feasibility and consistent demand among Uganda’s emergency care providers.
STABILITY AND SUSTAINABILITY: Despite reaching a mature phase of implementation by 2023, session frequency remained robust, and retention metrics (repeat logins and extended participation times) suggest the model remains both relevant and valued across varied contexts.
Discussion
The EMS ECHO Uganda initiative has demonstrated significant potential to bridge critical gaps in emergency medical skills among frontline health workers in Uganda, as evidenced by its substantial nationwide reach, participant diversity, and sustained engagement levels. This discussion contextualizes the key findings, evaluates their implications, explores the broader impact on emergency care delivery, and outlines policy recommendations for scaling telementorship initiatives in similar resource-limited settings.
NATIONWIDE REACH AND SCALABILITY
The findings show that the EMS ECHO Uganda program successfully leveraged virtual platforms to achieve comprehensive geographic coverage, reaching health workers from all 146 districts across Uganda. Telehealth and e-health initiatives like ECHO have proven highly effective in overcoming geographical barriers, providing crucial support and continuous medical education to health workers in remote and underserved regions. The rapid scale-up of this Uganda program from an initial pilot in 2021 to regular bi-weekly sessions reflects the adaptability and potential scalability of this model within resource-constrained environments. This is consistent with World Health Organization recommendations advocating innovative approaches, including digital health strategies, to strengthen emergency and pre-hospital care, particularly in rural and peri-urban settings.
ENGAGEMENT AND RETENTION
High retention rates, indicated by repeat attendance and extended participation durations, highlight substantial learner engagement and perceived program value. Notably, approximately 400 participants consistently attending more than 20 sessions each demonstrate a strong commitment, suggesting high relevance and effectiveness in addressing the urgent need for emergency care competencies. These robust engagement indicators further validate the interactive and case-based pedagogical approach inherent in the ECHO model, which promotes active learning through peer-to-peer interactions and practical applications. Such interactive methodologies have been shown to foster vibrant communities of practice, enhancing sustained professional development and retention of critical knowledge and skills.
PROFESSIONAL DIVERSITY AND INTER-PROFESSIONAL COLLABORATION
The EMS ECHO initiative brought together a diverse range of professionals, including doctors, nurses, midwives, allied health professionals, specialists, and emergency medical technicians, fostering valuable interdisciplinary collaboration and dialogue. This diverse professional representation addresses previously reported gaps where frontline, non-specialist healthcare workers lacked sufficient confidence and competencies to manage complex emergencies effectively, contributing significantly to high early mortality rates in emergency departments. Strengthening interdisciplinary collaboration through the structured virtual interactions inherent in the sessions fosters coordinated emergency responses, potentially reducing emergency-related mortality and morbidity significantly. Similar inter-professional education and collaboration models have been widely recognized as crucial elements for effective healthcare delivery and improved patient outcomes.
ADDRESSING IMMEDIATE KNOWLEDGE GAPS
The substantial immediate knowledge gains, as evidenced by improved pre- and post-session assessments, demonstrate the effectiveness of the EMS ECHO model in transferring critical emergency care skills rapidly. However, the reliance solely on immediate post-session assessments highlights a limitation concerning the evaluation of sustained knowledge retention and real-world clinical practice changes. Future evaluations should integrate longitudinal follow-up assessments and incorporate qualitative methodologies such as in-depth interviews, focus group discussions, and observational studies to capture the changes in clinical behaviors, practices, and health outcomes comprehensively. Additionally, comparative studies measuring patient-level outcomes such as morbidity, mortality, and quality of emergency care before and after implementation could offer critical insights into the tangible clinical impact of this model.
POLICY AND PROGRAMMATIC IMPLICATIONS AND RECOMMENDATIONS
Given the demonstrated effectiveness and scalability of the initiative amidst Uganda’s substantial shortage of trained emergency care providers, telementorship offers a cost-effective, scalable method to rapidly enhance workforce competencies. The success of the EMS ECHO initiative also emphasizes the importance of integrating telehealth strategies into national health workforce development policies. Policy-level support and strategic investments should prioritize integrating telementorship models into national emergency care training frameworks. These frameworks should explicitly support the expansion and institutionalization of virtual training platforms, ensuring sustainability through dedicated funding streams and infrastructure support, including robust internet connectivity and equipment at health facilities. Furthermore, aligning telementorship initiatives with national continuing professional development (CPD) policies and emergency care guidelines could institutionalize and enhance the long-term sustainability of this impactful approach.
Conclusion
The EMS ECHO Uganda initiative provides a compelling model for addressing the emergency care skills gap through scalable, interactive virtual mentorship. Its demonstrated feasibility, extensive coverage, and strong participant engagement reinforce the potential of telementorship to transform emergency medical education and practice in resource-constrained settings. Sustained policy support and comprehensive evaluations will be essential to maximize its long-term impact and scalability across similar environments globally.
Limitations
This evaluation had several limitations.
- Pre-posttests measured immediate knowledge acquisition but not long-term retention or changes in clinical practice.
- Self-selection into sessions may introduce participation bias toward more motivated learners.
- Reliance on Zoom platform data limited verification of individual-level attendance beyond login metrics.
- Verification of Attendance; Logging in and fully listening and participating fully was hard to measure and participants who may join as a group but in the same physical room could not have their details captured.
Conflicts of Interest Statement
There are no conflicts of Interest.
Funding Statement
No funding for the study.
Acknowledgments
We acknowledge the EMS ECHO participants over the years, the experts, case presenters and moderators for the commitment to voluntarily deliver the virtual education sessions.
References
- Chang CY, Abujaber S, Reynolds TA, Camargo CA, Obermeyer Z. Burden of emergency conditions and emergency care usage: new estimates from 40 countries. Emerg Med J. 2016;33(11):794-800.
- Razzak J, Usmani MF, Bhutta ZA. Global, regional and national burden of emergency medical diseases using specific emergency disease indicators: analysis of the 2015 global burden of disease study. BMJ Glob Health. 2019;4(2):e000733.
- Hansoti B, Aluisio AR, Barry MA, et al. Global health and emergency care: defining clinical research priorities. Acad Emerg Med. 2017;24(6):742-753.
- Walsh L, Subbarao I, Gebbie K, et al. Core competencies for disaster medicine and public health. Disaster Med Public Health Prep. 2012;6(1):44-52.
- Lohela TJ, Nesbitt RC, Manu A, et al. Competence of health workers in emergency obstetric care: an assessment using clinical vignettes in Brong Ahafo region, Ghana. BMJ Open. 2016;6(6):e010963.
- Czabanowska K, Kuhlmann E. Public health competences through the lens of the COVIDâ€19 pandemic: what matters for health workforce preparedness for global health emergencies. Int J Health Plann Manage. 2021;36(S1):14-19.
- Liu JX, Goryakin Y, Maeda A, Bruckner T, Scheffler R. Global health workforce labor market projections for 2030. Hum Resour Health. 2017;15:1-12.
- Al-Worafi YM. Healthcare workforce issues in developing countries: Public health and others. In: Handbook of Medical and Health Sciences in Developing Countries: Education, Practice, and Research. Springer; 2023:1-25.
- UBOS. Demographic and Health survey. Published online 2022. Accessed July 1, 2025. https://www.ubos.org/wp-content/uploads/publications/UDHS-2022-Report.pdf
- Seed Global Health. Emergency care systems in Uganda. Published online 2024. Accessed July 1, 2025. https://seedglobalhealth.org/wp-content/uploads/2025/03/Final-Report-Assessment-of-Ems.pdf
- Kamukama A, Kwesiga B, Migisha R, et al. Assessment of emergency medical services, Uganda, 2020–2023.
- Böbel S, Verhoeven J, Scholz M, et al. Strengthening the WHO Emergency Care Systems Framework: insights from an integrated, patient-centered approach in the Copenhagen Emergency Medical Services system—a qualitative system analysis. BMC Health Serv Res. 2025;25(1):401.
- Arora S, Thornton K, Murata G, et al. Outcomes of treatment for hepatitis C virus infection by primary care providers. N Engl J Med. 2011;364(23):2199-2207.
- Atuhairwe I, Ngabirano AA, Ahaisibwe B, et al. Leveraging tele-mentoring and remote learning to strengthen the emergency care capacity of health workers in Uganda. Afr J Emerg Med. 2023;13(2):86-93.
- Scott RE, Mars M. Telehealth in the developing world: current status and future prospects. Smart Homecare Technol TeleHealth. Published online 2015:25-37.
- Arora S, Kalishman SG, Thornton KA, et al. Project ECHO: a telementoring network model for continuing professional development. J Contin Educ Health Prof. 2017;37(4):239-244.
- Struminger B, Arora S, Zalud-Cerrato S, Lowrance D, Ellerbrock T. Building virtual communities of practice for health. The lancet. 2017;390(10095):632-634.
- Kevin O’Neill D. Building social capital in a knowledge-building community: Telementoring as a catalyst. Interact Learn Environ. 2004;12(3):179-208.
- Moss P, Nixon P, Baggio S, Newcomb D. Turning strategy into action–using the ECHO model to empower the Australian workforce to integrate care. Int J Integr Care. 2023;23(2):16.
- Thistlethwaite JE. Interprofessional education and the basic sciences: Rationale and outcomes. Anat Sci Educ. 2015;8(4):299-304.
- Wanjiku G, Dreizler L, Bell G, Wachira B. Feasibility of project ECHO telementoring to build capacity among non-specialist emergency care providers. Afr J Emerg Med. 2022;12(4):352-357.
- Bamberger M. Introduction to mixed methods in impact evaluation. Impact Eval Notes. 2012;3(3):1-38.

