Measuring Hand and Wrist Surgery Outcomes: A New Tool
A Tool to Measure Outcomes in the Hand and Wrist
Ronit Wollstein MD 1,2; Sarah Ewald 3; Esther Vögelin 4
1.Department of Orthopaedic Surgery, New York University School of Medicine, NY, USA
2.Department of Orthopaedic Surgery, UAB Heersink school of Medicine, Birmingham Alabama, USA
3.City Handtherapie, Zurich, Switzerland
4 .nselspital, University Hospital of Bern
* [email protected]
OPEN ACCESS
PUBLISH: 31 July 2025
CITATION Wollstein,R.,Ewald,S., et al., 2025.A Tool toMeasure Outcomes in the Hand and Wrist.Medical Research Archives, [online] 13(7).https://doi.org/10.18103/mra.v13i7.6812
COPYRIGHT© 2025 European Society of Medicine. This is an open-access article distributed under the terms of the Creative Commons AttributionLicense, which permits unrestricted use,distribution, and reproduction in any medium,provided the original author and soure are credited.
DOI:https://doi.org/10.18103/mra.v13i7.6812
ISSN 2375-1924
ABSTRACT
There has been a consistent effort to improve the way we measure outcomes in hand and wrist surgery. The advantages of widely accepted outcome measures include patient specificity and the ability to appropriately compare results. We developed a consensus tool based on subjective and objective measures. All of the tests have been previously validated. We present a series of patients and some preliminary results. It seems that this test allows for a detailed and specific assessment of the patient’s outcome. Further study and policy decision on which tests should be used may enable a more uniform on one hand and patient specific on the other, evaluation of outcomes in the hand and wrist.
Keywords
- Hand surgery
- Wrist surgery
- Outcome measures
- Patient reported outcomes
INTRODUCTION
There has been a consistent trend to try and improve the way we measure outcomes in hand and wrist surgery. The advantages of outcomes measurements that are specific to a patient on one hand, and standardized on the other, include the ability to adequately compare results and the potential to unambiguously differentiate between expected/good outcomes and those that are poorer or less than expected. This evidence can lead to the establishment of generalized guidelines for treatment and rehabilitation as well as may allow for outcomes assessment that is not dependent on fiscal or political considerations but rather on patient well-being as the main goal of treatment.
In an effort to provide standards of care, there has been a push towards high-level randomized clinical trials in medicine in general and in wrist specifically in order to provide standards but most critical analyses demonstrate suboptimal reporting. This endeavor is problematic since the expectations and tasks are so variable—particularly in the hand and wrist—that standardization seems almost an impossible feat. How can we appropriately compare the results of a distal radius fracture treated surgically in an active golf player to a fracture in a musician? We have to account for the fracture characteristics, treatment, including therapy provided, but more importantly the patient characteristics that will determine expectations and function. Many of these variables are impossible to account for at this time.
So, while standardization requires large databases, the challenge of truly evaluating individual outcome is rarely met. Examples of factors we do not account for are patient expectations, differences in occupation, and disparities of social support. While the treating surgeon may evaluate an outcome one way, the patient may see things differently.
The most frequently reported clinical outcomes for hand issues are range of motion (ROM) and grip strength. Though functional scoring systems have been devised and employed to add information, many of these include ROM and grip strength as the only objective measurement. While standardized assessment of grip strength is well described and produces a reliable measurement when performed in the standardized manner, ROM measurements with a goniometer are not standardized, and can result in vastly different results depending on the examiner. This in turn limits their usefulness when comparing outcomes from different studies.
Numerous variations of patient reported outcome (PRO) scores have been developed. These are subjective assessment tools for evaluating the personal perception of a patient’s performance in daily living including work, sports and other activities. Commonly used PRO tools are the Michigan hand questionnaire (MHQ), the patient-rated wrist evaluation (PRWE), and the disabilities of the arm, shoulder, and hand questionnaire (DASH). The manual ability measure (MAM) 16 and 36 scoring systems are also patient rated scales that focus on daily activities. While the most notable advantage of these tools is their ability to provide information in a quantitative format regarding the patient’s satisfaction in his/her daily life performance, the fact that this tool is subjective limits its applicability.
Other functional scores such as the Mayo wrist score and the Gartland & Werley tests, are performed by the physician. These theoretically include the advantage of a more objective evaluation but the evaluator may not always be disinterested and still relies on the patient’s articulation of parameters such as pain, stiffness, and function.
More detailed/task specific functional evaluation systems have been described. There are multiple tests of manual dexterity that are valid and reliable, many of these tests however have the drawback that they do not utilize items from everyday life. An example of such test would be the functional dexterity test, which primarily measures in-hand manipulation abilities and thus has limited application for evaluating the wrist. Other tests such as: the Sollerman test of hand function or the Jebsen-Taylor test of hand function or the sequential occupational dexterity test (SODA), evaluate hand function during specific functional tasks. These tests aim to more specifically evaluate everyday functions of the hand and fingers and indirectly evaluate the wrist, as the wrist serves as a foundation to position the hand optimally to perform a task efficiently and effectively. However, except for the functional dexterity test, the tests of function require the proper equipment and are time intensive to perform (upwards of 20 minutes or more) and often do not stress the wrist sufficiently to accurately reflect everyday hand use. Thus, because the tasks are fairly easy to perform and do not require specialized movement and load, such as removing coins from a coin purse in the Sollerman test, the true impact of a wrist condition upon hand function is not exposed.
It is likely that the tasks evaluated should be specific not only to the patient and his/her needs but also to the particular pathology addressed. In the study of the thumb carpometacarpal joint osteoarthritis, the investigators evaluated key pinch, cylindrical grasp and jar twist as means of evaluating function specific to the joint.
In an attempt to address this challenge, a group of wrist researchers, therapists and surgeons have agreed on a collection of already proven/validated tests to address patient specific outcomes. This tool allows for a visual representation of the measurements and has been modified in response to feedback from patients and therapists and includes objective and subjective measurement tools. This will likely help in providing shared decision making since both the patient and the treating therapist and surgeon evaluate the patients’ results the same way and see the same graph (visual representation) of outcome.
The purpose of this series is to present the tool and a series of patients evaluated by utilizing it.
METHODS:
THE EVALUATION TOOL:
The evaluation tool was established by a group of international hand surgeons, hand therapists and researchers in the field. In a meeting in Bern Switzerland in 2020, a consensus of already validated tests for outcome measurement in the wrist was achieved. In an attempt to provide a testing tool that would be patient specific and truly reflect patient outcome, the tool consists of 2 parts. One part includes questionnaires the patient answers (PROMs) and the second part includes objective measurements performed by the evaluator. When entering the results, the scores of every evaluation time point are automatically plotted on a spider diagram to allow visualization of weaker areas that should be addressed in therapy or surgery and to allow the patient and the evaluator to visualize progress along the time points. (Supplementary material includes the tests, the excel file to upload the scores and a user manual that includes instructions for the individual tests that are included)
RESULTS:
In a preliminary pilot study, the tool was found to be patient and condition specific, and the patients and providers felt that the tool was able to reflect true results. It was not difficult to apply in multiple health environments and countries. The evaluation tool allowed for easy shared decision making since both the patient and the provider see the same visual representation of the measured tests.
CASE SERIES:
CASE 1:
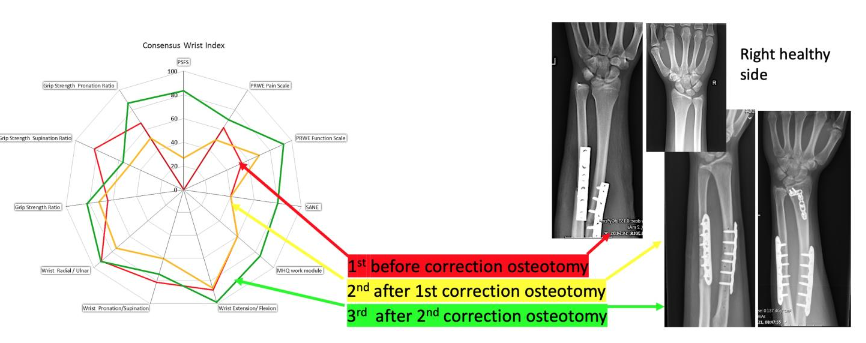
A 15-year-old, female presented with a malunion of the left forearm 2 years after a forearm shaft fracture. This had initially been treated with plate osteosynthesis. The radial plate was removed 1 year following the original fracture surgery. She presented with a Madelung-like deformity and pain (though stating that the pain had existed some years prior to the fracture).
She underwent 2 subsequent surgeries due to continued pain and loss of motion. The first surgery included a navigated correction osteotomy of the radius and ulna, with removal of the ulnar plate, and the second (4 months later) included an additional intra-articular correction osteotomy of the radius to address an additional intra-articular malunion of the lunate fossa.
Summary of wrist index: (Figures 1a and 1b). There are moderate changes in measurements for hand function before and after the first 2 surgeries. In contrast, PROM’s only improved at 6 months after the second correction osteotomy. This illustrates that PROM’s were more rigorous in providing the true outcome of the involved hand by measuring subjective values compared to the objective measurements of force, range of motion and 2-point discrimination.
CASE 2:
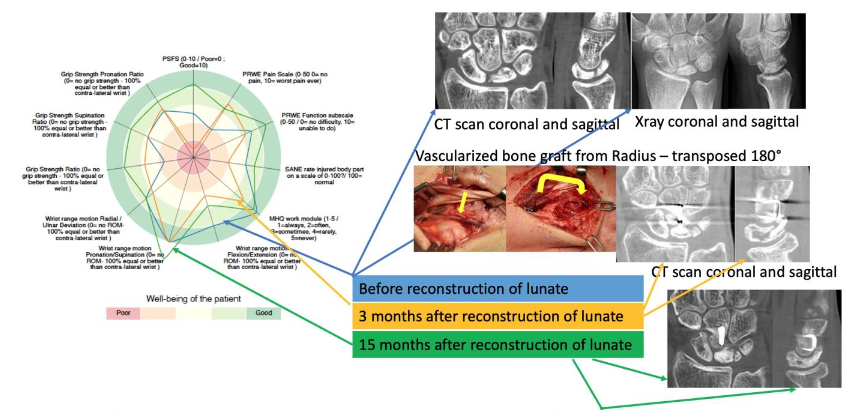
A 33-year-old, male, biology student, presented with Kienböck’s disease (avascular necrosis of the lunate bone) Lichtman stage IIIA with reduced carpal height and partial fragmentation of the lunate. Despite conservative treatment, he developed increasing pain with inability to bike, climb and strength-train. Since he was ulna-neutral and a had a lunate Type II, surgical treatment included a vascularized bone graft from the radius (septal pedicle 4/5) and a capitate shortening. Healing was uneventful with some clinical improvement.
Summary of wrist index: (Figures 2a and 2b) The range of motion in flexion remained markedly reduced despite intensive hand therapy and progressive splinting. PROM’s improved. The wrist index shows that despite suboptimal objective improvement, his PROM’s did improve. Since he was painfree, and could perform all activities.
CASE 3:
A 37 year-old, female, office worker, presented with a painful intraosseous cyst in the distal third of the scaphoid associated with swelling over the 2nd and 3rd extensor compartments. The pain significantly limited her function. She was treated with a bone graft from the radius, fixed with an intraosseous screw. Evaluation 6 months after surgery demonstrates improvement in pain but at 12 and 24 months post surgery despite healing of the cyst, she continued to complain of significant disability related to the use of her thumb. Further investigation using ultrasound demonstrated scarring and adherence of the extensor pollicis longus tendon (EPL) irritating a branch of the superficial radial nerve.
Summary of wrist index: (Figures 3a and 3b)
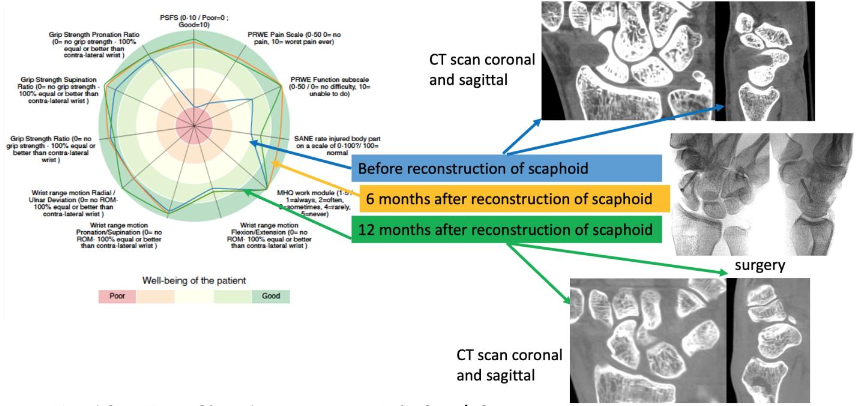
Subjectively, the patient worsened over time especially in the patient specific testing. Despite a good range of motion and grip strength after surgery, again the PROM’s were worse 1 year after surgery. The tool was able to assist in identifying a different problem affecting the patient’s outcome.
DISCUSSION:
Multiple factors affect hand and wrist function. These include factors that we are able to account for such as injury severity and age, but also many factors such as social support, occupational and other specific functional expectations, that we are unable to account for. As a result, our ability to evaluate and ultimately compare and communicate true patient outcomes remains limited.
This consensus outcome tool that we present seems to address the issue of patient and condition specificity. Incorporating multiple areas for patient input may enable measurement of true outcome. It has the advantage of incorporating already used and validated tests and seems to be fairly easy to integrate into diverse health care settings, though further study is needed to substantiate this aspect of the outcome tool.
Another area that still needs to be investigated is the question of whether a condition-specific amendment to the tool should be added to adjust for particular issues related to certain conditions (for example measuring pinch strength in thumb carpometacarpal joint osteoarthritis as opposed to measuring grip strength that would be less specific to the condition).
Despite the push for personalized medicine and decision sharing between the provider and the patient, in many health environments, there remains a need to standardize the way we measure outcomes. These are used to determine compensation and to provide guidelines for care. The question therefore remains, how do we on one hand measure true patient outcomes but on the other provide standards? We believe the way to do this is to use a large number of individual outcomes analyzed using big data. Big data is defined as “extremely large data sets that may be analyzed computationally to reveal patterns, trends, and associations, especially relating to human behavior and interactions.”
In order to be able to do this there is first a need to come up with an agreed upon number of tests or tools that could be used by many. We believe that an understanding would need to obtained across countries and health systems to achieve the goal of uniformity in assessment and the ability to accurately compare outcomes.
In summary, we present an attempt to provide a consensus patient specific outcome measure. Further study is needed but further policy decisions can aid in our ability to not only evaluate our care correctly, but also to control the narrative in our respective healthcare specialties and environments.
REFERENCES:
- Ziebart C, Mehta SP, MacDermid J. Measurement Properties of Outcome Measures Used to Assess Physical Impairments in Patients After Distal Radius Fracture: A Systematic Review. Phys Ther. Feb 27 2021;doi:10.1093/ptj/pzab080
- Spanswick PJC, Whittier DE, Kwong C, Korley R, Boyd SK, Schneider PS. Improvements in radiographic and clinical assessment of distal radius fracture healing by FE-estimated bone stiffness. Bone Rep. Jun 2021;14:100748. doi:10.1016/j.bonr.2021.100748
- Rosvall F, Jedeskog U, Andersson JK, Soderberg T, Hagert E. Intrarater reliability test of the ISOmetric power device-A new instrument for assessment of isometric force in six directions of wrist motion. Journal of hand therapy : official journal of the American Society of Hand Therapists. Jan-Mar 2021;34(1):100-108. doi:10.1016/j.jht.2019.12.013
- Karantana A, Davis T, Kennedy D, et al. Common hand and wrist conditions: creation of UK research priorities defined by a James Lind Alliance Priority Setting Partnership. BMJ Open. Mar 26 2021;11(3):e044207. doi:10.1136/bmjopen-2020-044207
- Wilkinson CP. Evidence-based medicine regarding the prevention of retinal detachment. Trans Am Ophthalmol Soc. 1999;97:397-404; discussion 404-6.
- Becker A, Blumle A, Momeni A. Evidence-based Plastic and Reconstructive Surgery: developments over two decades. Plastic and reconstructive surgery. Oct 2013;132(4):657e-663e. doi:10.1097/PRS.0b013e31829fe0f7
- Slutsky DJ. Editorial. J Wrist Surg. Aug 2013;2(3):195-6. doi:10.1055/s-0033-1351376
- Dario P, Matteo G, Carolina C, et al. Is it really necessary to restore radial anatomic parameters after distal radius fractures? Injury. Dec 2014;45 Suppl 6:S21-6. doi:10.1016/j.injury.2014.10.018
- Carter TI, Pansy B, Wolff AL, et al. Accuracy and reliability of three different techniques for manual goniometry for wrist motion: a cadaveric study. J Hand Surg Am. Oct 2009;34(8):1422-8. doi:10.1016/j.jhsa.2009.06.002
- Paranaiba VF, Santos J, Raduan Neto J, Moraes VY, Belotti JC, Faloppa F. PRWE application in distal radius fracture: comparison and correlation with established outcomes. Rev Bras Ortop. May-Jun 2017;52(3):278-283. doi:10.1016/j.rboe.2016.07.007
- Shauver MJ, Chang KW, Chung KC. Contribution of functional parameters to patient-rated outcomes after surgical treatment of distal radius fractures. J Hand Surg Am. Mar 2014;39(3):436-42. doi:10.1016/j.jhsa.2013.11.015
- Aaron DH, Jansen CW. Development of the Functional Dexterity Test (FDT): construction, validity, reliability, and normative data. J Hand Ther. Jan-Mar 2003;16(1):12-21.
- Poole JL, Huffman M, Hunter A, Mares C, Siegel P. Reliability and validity of the Manual Ability Measure-36 in persons with Charcot-Marie-Tooth disease. J Hand Ther. Oct-Dec 2015;28(4):364-7; quiz 368. doi:10.1016/j.jht.2015.04.003
- Dacombe PJ, Amirfeyz R, Davis T. Patient-Reported Outcome Measures for Hand and Wrist Trauma: Is There Sufficient Evidence of Reliability, Validity, and Responsiveness? Hand (N Y). Mar 2016;11(1):11-21. doi:10.1177/1558944715614855
- van Lankveld W, van’t Pad Bosch P, Bakker J, Terwindt S, Franssen M, van Riel P. Sequential occupational dexterity assessment (SODA): a new test to measure hand disability. J Hand Ther. Jan-Mar 1996;9(1):27-32.
- Prada V, Robbiano G, Mennella G, et al. Validation of a new hand function outcome measure in individuals with Charcot-Marie-Tooth disease. J Peripher Nerv Syst. Dec 2020;25(4):413-422. doi:10.1111/jns.12421
- Ladd AL. The Teleology of the Thumb: On Purpose and Design. J Hand Surg Am. Mar 2018;43(3):248-259. doi:10.1016/j.jhsa.2018.01.002

