Minimally Invasive Glaucoma Surgery: Techniques and Insights
Angle-based Minimally Invasive Glaucoma Surgery-procedures in glaucoma treatment
Karsten Klabe1 and Andreas Fricke2
- Karsten KlabeInternationale Innovative Ophthalmochirugie GbR; Martin-Luther-Platz 22/26; 40212 Düsseldorf, Germany
- Andreas FrickeInternationale Innovative Ophthalmochirugie GbR; Martin-Luther-Platz 22/26; 40212 Düsseldorf, Germany
OPEN ACCESS
PUBLISHED: Jul 25, 2025
CITATION: Klabe K and Fricke A, 2025. Angle-based Minimally Invasive Glaucoma Surgery-procedures in glaucoma treatment. Medical Research Archives, [online] Volume 10 Issue 7. https://doi.org/10.18103/mra.v10i7.2671
COPYRIGHT: © 2025 European Society of Medicine. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
DOI: https://doi.org/10.18103/mra.v13i7.6761
ISSN 2375-1924.
ABSTRACT
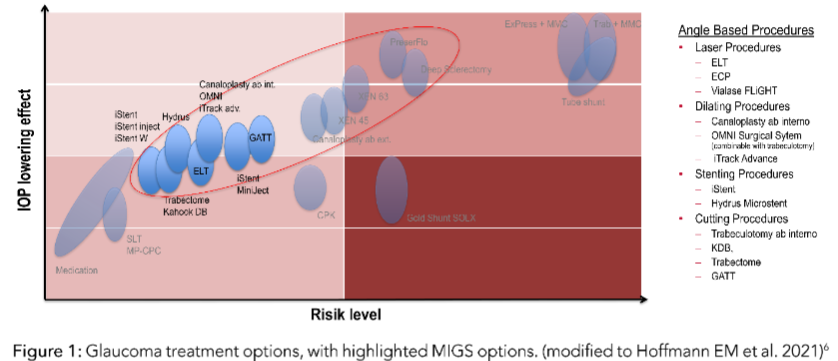
Surgical procedures for glaucoma are an increasingly important role in the treatment of glaucoma. The treatment is often necessitated due to structural alterations of the trabecular meshwork, in the chamber angle, Schlemm canal and the distal collector channels. The aim of the glaucoma treatment paradigm is evolving from a reactive approach to a more proactive procedural approach. Approximately 50-70% of the total burden of glaucoma treatment is related to lowering intraocular pressure (IOP). The first-line therapy for lowering intraocular pressure is usually the administration of medication in the form of eyedrops. Poor compliance and tolerability can sometimes lead to treatment failure. The glaucoma treatment paradigm is evolving from a reactive approach to a more proactive procedural approach, a shift that has been termed “minimally invasive glaucoma surgery” (MIGS). The selection of the MIGS procedure should be based on the severity of the glaucoma, the surgical skills of the surgeon, the desired target pressure and the patient’s needs.
Keywords:
- Glaucoma
- Minimally Invasive Surgery
- Intraocular Pressure
- Trabecular Meshwork
- MIGS
Introduction
Glaucoma is still the second leading cause of blindness. The risk factors for glaucoma-related blindness are the severity of the disease at diagnosis, bilateral disease, and age. Currently, the only effective approach to preserving visual function in glaucoma is the reduction of the intraocular pressure (IOP). The first-line therapy for lowering intraocular pressure is usually the administration of medication in the form of eyedrops. Poor compliance and tolerability can sometimes lead to treatment failure. The glaucoma treatment paradigm is evolving from a reactive approach to a more proactive procedural approach, a shift that has been termed “minimally invasive glaucoma surgery” (MIGS).
The selection of the MIGS procedure should be based on the severity of the glaucoma, the surgical skills of the surgeon, the desired target pressure and the patient’s needs.
Angle-based Minimally Invasive Glaucoma Surgery-procedures
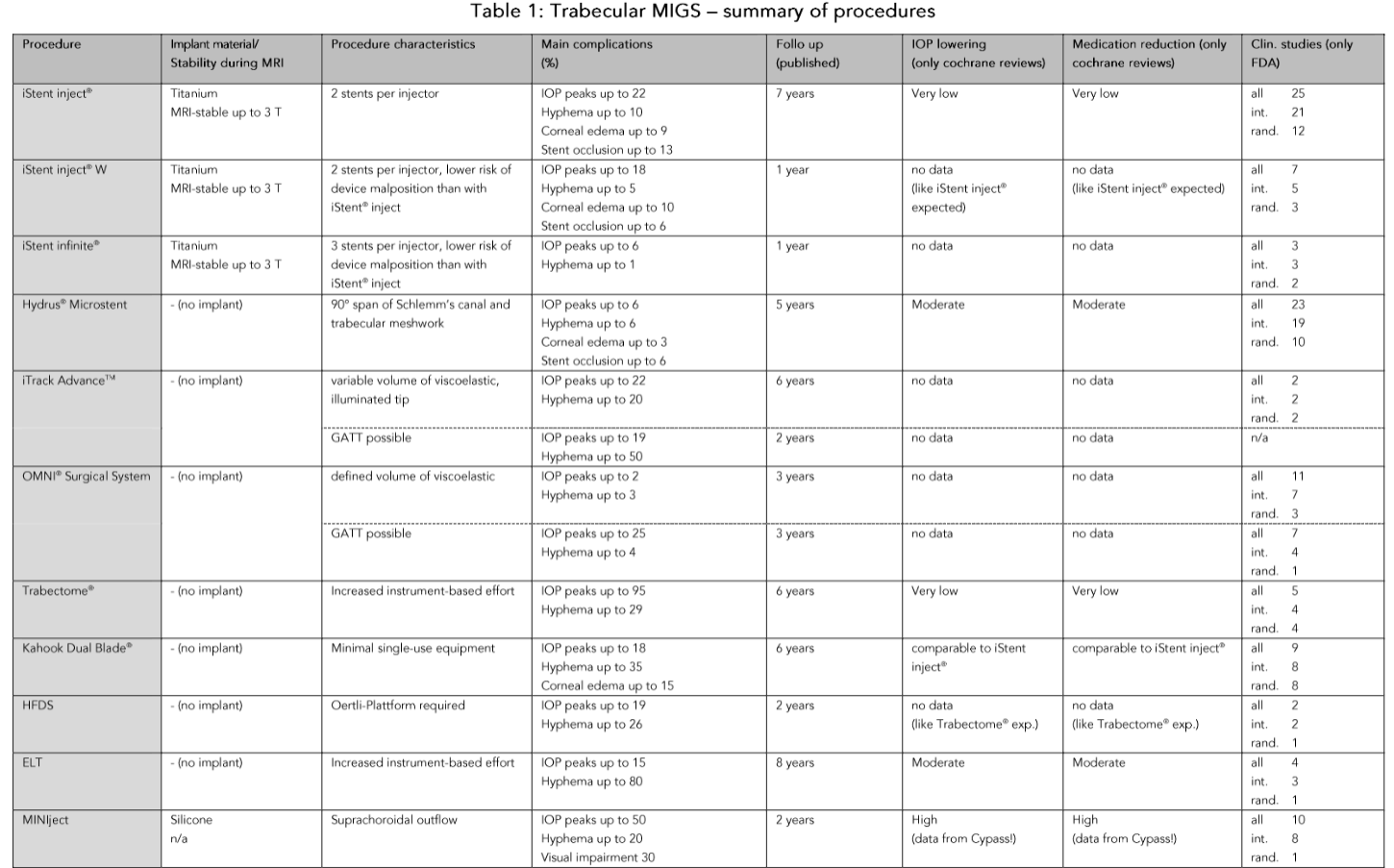
iStent
The first generation of iStent® (Glaukos Corp., Aliso Viejo, CA, USA; 2004) consisted of an angled, half-open titanium stent that was implanted into Schlemm’s canal after perforation of the trabecular meshwork. The part recorded in Schlemm’s canal had collectible-like divisions that prevented obstruction. Zade et al. found a reduction in IOP from a preoperative mean of 21.3 to 16.4 mmHg 7 years after combined cataract surgery with implantation of a first-generation stent. Preoperatively, a mean of 21.7 anti-glaucoma medications was required. After 7 years, an average of 1.5 medications. Even without combined cataract surgery, the IOP reduction was significant, with a reduction in IOP and the number of medications required.
Hydrus® Microstent
The Hydrus® Microstent (Alcon, Fort Worth, TX, USA) was also developed for trabecular implantation. At 8 mm in length, it is significantly larger than the iStents. Like the first generation iStent, the Hydrus is implanted laterally into Schlemm’s canal using the applicator after incision of the trabecular meshwork. Compared to the iStent, only the ostium, which is located at the transition from the anterior chamber to Schlemm’s canal, is exposed to the aqueous humor. The pressure-lowering effect was 38% at 12 months.

iTrack System and OMNI System
Up-to-date publications show a significant and sustained reduction in pressure and medication use with the iTrack system and the OMNI system. In a first retrospective study, Gallardo et al. compared canaloplasty as an adjunct to stand-alone procedure (n = 41) with the combination with cataract surgery (n = 34). The pressure-lowering effect at 8 years was slightly higher with the stand-alone procedure, compared to the combined procedure (31.7%). In the reduction of pressure-lowering medications, the combination was reported by other authors.
Trabeculectomy Ab Interno
Compared to classic goniotomy, the Trabectome® (Neomedix, Tustin, USA) not only incises the trabecular meshwork, but were removed over the inner wall of the SC a 90°-120° range. At the same time as the electroblation of the tissue, irrigation is carried out via an infusion to cool and suction off the ablated tissue. In addition to anti-inflammatory substances, pilocarpine should be administered for several days after the trabectome application to prevent the aqueous humor from sticking to the trabecular meshwork.

| Procedure | Implant material | Stability | Main complications | Follow-up (months) | Medication reduction (in %) | Clinical studies (n) | FDA studies (n) |
|---|---|---|---|---|---|---|---|
| iStent® | Titanium | 1 year | Very low | 12 | 50-60% | 2 | 1 |
| Hydrus® Microstent | Silicone | 2 years | Low | 24 | 30-40% | 1 | 1 |
| OMNI® Surgical System | Non-implant | 3 years | Moderate | 12 | 50-60% | 2 | 1 |
References
- Funke CM, Ristow D, Yadgarov A, Micheletti JM. Interventional glaucoma consensus treatment protocol. Expert Review of Ophthalmology. 2025; 202(2):79-87.
- Lavia C, Dallorto L, Maulé M, Ceccarelli M, Fea AM. Minimally-invasive glaucoma surgeries (MIGS) for open angle glaucoma: A systematic review and meta-analysis. PLoS One. 2017;12(8):e0183142.
- Weich C, Zimmermann JA, Storp JU, et al. Comparison of the Intraocular Pressure Lowering Effect of Minimally Invasive Glaucoma Surgery (MIGS) iStent Inject W and Hydrus-The 12-Month Real-Life Data. Diagnostics (Basel). 2025;15(4):493.

