Myocardial Infarction in Young Patients: Case Report
Type 1 myocardial infarction in a 27-year-old patient with substance abuse, IGM antibodies against borrelia burgdorferi and hypercholesterolemia: Case report
Alexey Anokhin, MD1, Ksenija Stach MD2, Daniel Duerschmied, MD1,3,4, Reinhard Sauter1,5, Harald F. Langer, MD1,3,4,5
- Cardiology, Angiology, Haemostaseology, and Medical Intensive Care, Medical Centre Mannheim, Medical Faculty Mannheim, Heidelberg University, Germany
- 5th Medical Department, University Hospital Mannheim, Heidelberg University, Mannheim, Germany
- Cardiology, Angiology, Haemostaseology, and Medical Intensive Care, Medical Centre Mannheim, Medical Faculty Mannheim, Heidelberg University, Germany; European Center for AngioScience (ECAS), German Center for Cardiovascular Research (DZHK) partner site Heidelberg/ Mannheim, and Centre for Cardiovascular Acute Medicine Mannheim (ZKAM), Medical Centre Mannheim, Heidelberg University, Germany; Helmholtz Institute for Translational AngioCardioScience (HI-TAC), Medical Faculty Mannheim, Heidelberg University, Germany
- Cardiology, Angiology, Haemostaseology, and Medical Intensive Care, Medical Centre Mannheim, Medical Faculty Mannheim, Heidelberg University, Germany; Cardiovascular Systems Biology, Medical Faculty Mannheim, Heidelberg University, Germany
- Cardiology, Angiology, Haemostaseology, and Medical Intensive Care, Medical Centre Mannheim, Medical Faculty Mannheim, Heidelberg University, Germany; European Center for AngioScience (ECAS), German Center for Cardiovascular Research (DZHK) partner site Heidelberg/ Mannheim, and Centre for Cardiovascular Acute Medicine Mannheim (ZKAM), Medical Centre Mannheim, Heidelberg University, Germany; Helmholtz Institute for Translational AngioCardioScience (HI-TAC), Medical Faculty Mannheim, Heidelberg University, Germany; Cardiovascular Systems Biology, Medical Faculty Mannheim, Heidelberg University,
OPEN ACCESS
PUBLISHED: 31 December 2025
CITATION: ANOKHIN, Alexey et al. Type 1 myocardial infarction in a 27-year-old patient with substance abuse, IGM antibodies against borrelia burgdorferi and hypercholesterolemia: Case report. Medical Research Archives, [S.l.], v. 12, n. 12, dec. 2024. Available at: <https://esmed.org/MRA/mra/article/view/5350>. Date accessed: 27 oct. 2025. doi: https://doi.org/10.18103/mra.v12i12.5350.
COPYRIGHT: © 2025 European Society of Medicine. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
DOI: https://doi.org/10.18103/mra.v12i12.5350
ISSN 2375-1924
Abstract
Background: The overall incidence of hospital admissions because of myocardial infarction attributable to young patients seems to increase over the years. Myocardial infarction in young patients is a rare disease, it is necessary to identify young patients with a high risk profile to recognize and treat them in time.
Case Summary: We present a patient with an acute heart attack at a young age and several risk factors for a cardiovascular event, including multiple drug abuse and hypercholesterolemia. Additionally, the patient had a second-degree atrioventricular block and severely reduced pumping function in the echocardiography. Intriguing about this case is the exceptionally young age and the potential impact of the risk factors.
Discussion: This case illustrates that even young patients can experience an occlusive myocardial infarction and in the presence of cardiovascular risk factors, coronary heart disease should be considered even at a young age.
Keywords
case report, myocardial infarction, substance abuse, coronary artery disease
Learning Objectives:
- To be familiar with the standard operating procedure for myocardial infarction (MI) in young patients
- To understand the comorbidities and causing factors of MI in exceptionally young patients
Introduction
Cardiovascular diseases are among the most common diseases worldwide and are one of the leading causes of death. The primary cause of a heart attack is commonly acute exacerbation of a lesion originating from coronary artery disease (CAD), a chronic and complex condition of the coronary vessels, which can lead to progressive narrowing and ultimately complete occlusion. Known risk factors for CAD include dyslipidemia, smoking, obesity, hypertension, diabetes and physical inactivity. Standard therapy involves revascularization, antiplatelet therapy, optimization of lipid levels and blood pressure, as well as smoking cessation. Although myocardial infarction can also occur at a young age, albeit less frequently, data on this serious and often disturbing clinical setting is unfortunately very limited. Younger patients presenting with myocardial infarction can have different pathophysiologic processes and different risk factors, especially drug abuse is a frequently observed trigger. Importantly, increased attention for young patients with this severe disease can prevent delayed diagnosis and treatment.
Case Presentation
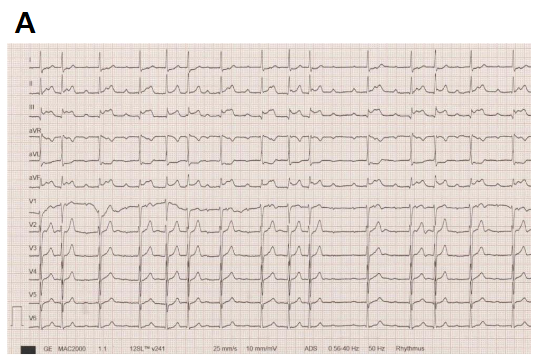
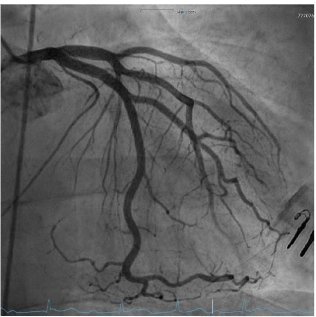
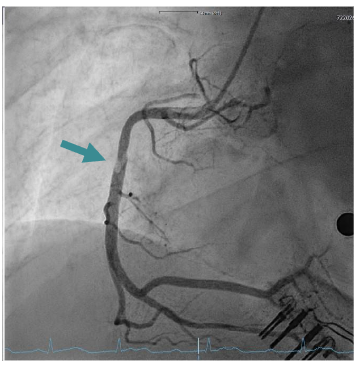
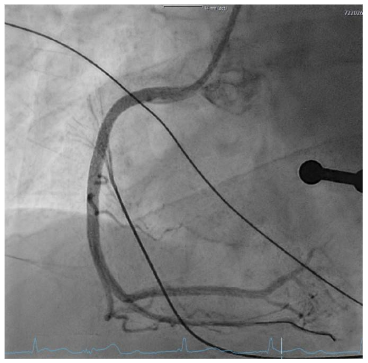
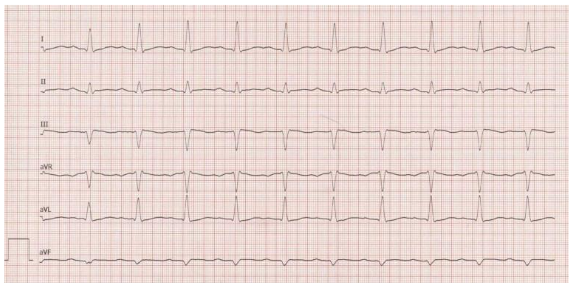
A 27-year-old patient presented with suspected ST-segment elevation myocardial infarction (STEMI). Approximately one hour prior to admission, the patient experienced onset of typical angina pectoris with accompanying vegetative symptoms (nausea and vomiting). Similar episodes had not occurred before. The patient’s medical history revealed regular or daily consumption of high-percentage alcohol, nicotine and cannabis. A few days before the event, the patient intended to consume nasal amphetamines, but due to a mix-up the substance consumed was heroin. No further substance use was reported. Furthermore, the patient had a tick bite approximately 10 years ago. The initial electrocardiogram (ECG) showed ST segment elevations in leads II, III, and avF, as well as a second-degree atrioventricular block (Mobitz type II) with a heart rate of approximately 70 beats/minute. Laboratory tests showed elevated cardiac biomarkers, with (troponin I 14.037 µg/l (cut-off value <0.045 µg/l) and CK-MB at 79 U/l (cut-off value <24U/l). Furthermore, the patient exhibited a flamboyant exanthema in large areas of the face with known atopic dermatitis. The patient reported of a pronounced stress response triggered by various problems in the work environment and social circle. After findings were reviewed in the Chest Pain Unit, based on the initial assessment, the patient was immediately transferred to the catheterization lab. The attending physician administered prehospital medication with aspirin and heparin. An emergency coronary angiography was performed, which revealed a single-vessel coronary disease with a subtotal occlusion of the right coronary artery (RCA) and high thrombus burden. During the procedure, the patient admitted that he had smoked marijuana the same morning. A primary stenting using a drug eluting stent (DES, Promus 4.0/32mm, Boston Scientific, Marlborough, Massachusetts) was performed, followed by stent optimization with balloon angioplasty. Complete reperfusion was documented immediately without evidence of remaining dissection or vascular injury. The placement of a temporary pacemaker was not necessary and the patient was transferred to our intensive care unit. Post-interventional follow-up showed no evidence of atrioventricular block and complete ST resolution on the following day. Dual antiplatelet therapy with acetylsalicylic acid and ticagrelor was initiated. On the following day, there was a slight increase in troponin I to a maximum of 18.469 µg/l, after which it then decreased, similarly CK values decreased. In addition, there was a slight increase in inflammatory markers, (CRP 41 mg/l, leukocytes 14.000/µl). LDL cholesterol was significantly elevated at 150 mg/dl (fasting, the following day), while HDL cholesterol was within the normal range at 40 mg/dl and triglycerides were at 145 mg/dl, Lipoprotein (a) 6.3 mg/dl. The urinary toxicology test showed a qualitative detection of benzodiazepines, cannabinoids, and opioids. Interestingly, serologically, IgM antibodies against Borrelia burgdorferi were detected without IgG antibodies. Further diagnostic workup included transthoracic and transesophageal echocardiography, which showed a severely reduced left ventricular ejection fraction (LVEF) of 29% by Simpson (biplane analysis), as well as an inferior inferolateral akinesia. Additionally, a floating structure measuring approximately 8x8mm was observed attached to the inferolateral wall, suggesting a ventricular thrombus. To further confirm the diagnosis and investigate the reduced LVEF, a cardiac magnetic resonance imaging (MRI) was scheduled. The possibility of providing a life vest was discussed until a decision regarding an implantable cardioverter-defibrillator (ICD) was made. Unfortunately, the patient declined further tests and treatments and left the hospital against our advice.
Discussion
Remarkable about this case is not only the very young age of the patient with 27 years. The overall incidence of hospital admissions because of myocardial infarction attributable to young patients seems to increase over the years, however the data for very young patients are limited. The Framingham study shows a decreasing incidence with younger age, in the group of 30 to 34 years old (male) the incidence was 1.29%, a group younger than 30 was not even defined. Myocardial infarction in young patients is a rare disease and comes with a similar risk profile compared to older, but is more often associated with male gender, hypercholesterolemia, smoking status, obesity, substance abuse and less with hypertension. Further data is required to identify young patients with a high risk profile to recognize and treat them in time.
The obvious risk factor of this patient was the massive use of substances, alcohol and nicotine. Especially the daily use of nicotine and cannabis may have contributed to the acute myocardial infarction. The risk of cannabis for cardiovascular diseases is still a matter of research. A systematic review of 85 publications with 541.518 patients in total shows at least an association between frequent cannabis use and an increased risk for acute coronary syndrome and chronic cardiovascular diseases. To further address this scientific issue is of particular interest in light of the ongoing discussion to legalize cannabis, e.g. in Germany.
Furthermore, the patient´s lipid profile was of relevance. The LDL cholesterol was significantly elevated at 150 mg/dl, while the other fat compartments were within normal range. The role of elevated LDL cholesterol at a young age is still a subject of research. A retrospective study of young STEMI patients in China showed a significantly higher LDL cholesterol in the group of 18-35 years-old compared to 36-44 years-old STEMI patients and dyslipidemia was an independent risk factor for the recurrence of cardiovascular events. Lipid lowering therapy was started with Rosuvastatin 20 mg and Ezetimibe 10 mg to reach the goal of 55 mg/dl. We suggest screening for dyslipidemia in young patients with further risk factors for cardiovascular diseases, as they may benefit from therapy for LDL reduction. Association of elevated LDL cholesterol probably stay in context of smoking/cannabis consumption and lead because of cholesterol years to atherosclerosis.
Another interesting aspect of this case is the second-degree atrioventricular block (Mobitz Type II) and the positive history of a tick bite. However, the significantly prolonged latency of 10 years and the serological evidence of IgM antibodies against Borrelia burgdorferi without detection of IgG are suggesting against a causality. Possible explanations could be another tick bite, a false positive serology or a persistent positive serostatus after a past infection. To further investigate a potential Lyme myocarditis, a cardiac MRI examination and possibly a myocardial biopsy would have been helpful. However, unfortunately the patient refused further investigations and therapies. In countries with endemic areas for borreliosis, we suggest patients with new atrioventricular blocks should be screened for potential lyme-myocarditis. Most likely, however, the cause of this block was the ruptured RCA plaque, which is supported by its reversibility after coronary angiography and intervention.
Conclusion
In conclusion, this case shows that very young patients can also experience acute myocardial infarction and the importance of screen those for cardiovascular risk factors and treat them. Especially in cases of young patients with substance abuse and inflammatory states further risk factors should be investigated.
Disclosures:
None
Author Contributions:
AA collected the important information and images for the case, created the initial draft and revised the report based on the feedback. HL was the attending physician, conceptualized and wrote the report. DD, RS and KS contributed essential sources and feedback to the report.
Conflict of interest:
The authors declare that no conflict of interest exists.
Funding:
This work was supported by the DZHK (German Research Centre for Cardiovascular Research), partner site Hamburg/Lübeck/Kiel. H.F.L. is supported by an ERA PerMed 2020 JTC grant “PROGRESS.” H.F.L. and D.D. were furthermore supported by the SFB1366/2 (project B08) of the DFG and the DZHK partner site Mannheim/Heidelberg.
References:
- Thygesen K, Alpert JS, White HD, et al. Universal definition of myocardial infarction. Circulation. Nov 27 2007;116(22):2634-53. doi:10.1161/circulationaha.107.187397
- Nording HM, Seizer P, Langer HF. Platelets in inflammation and atherogenesis. Front Immunol. 2015;6:98. doi:10.3389/fimmu.2015.00098
- Lawton JS, Tamis-Holland JE, Bangalore S, et al. 2021 ACC/AHA/SCAI Guideline for Coronary Artery Revascularization: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. Jan 18 2022;79(2):e21-e129. doi:10.1016/j.jacc.2021.09.006
- Gawaz M, Geisler T, Borst O. Current concepts and novel targets for antiplatelet therapy. Nat Rev Cardiol. Sep 2023;20(9):583-599. doi:10.1038/s41569-023-00854-6
- Johansson S, Rosengren A, Young K, Jennings E. Mortality and morbidity trends after the first year in survivors of acute myocardial infarction: a systematic review. BMC Cardiovasc Disord. Feb 7 2017;17(1):53. doi:10.1186/s12872-017-0482-9
- Shah N, Kelly AM, Cox N, Wong C, Soon K. Myocardial Infarction in the “Young”: Risk Factors, Presentation, Management and Prognosis. Heart Lung Circ. Oct 2016;25(10):955-60. doi:10.1016/j.hlc.2016.04.015
- Sagris M, Antonopoulos AS, Theofilis P, et al. Risk factors profile of young and older patients with myocardial infarction. Cardiovasc Res. Jul 27 2022;118(10):2281-2292. doi:10.1093/cvr/cvab264
- Krittanawong C, Khawaja M, Tamis-Holland JE, Girotra S, Rao SV. Acute Myocardial Infarction: Etiologies and Mimickers in Young Patients. J Am Heart Assoc. Sep 19 2023;12(18):e029971. doi:10.1161/jaha.123.029971
- Arora S, Stouffer GA, Kucharska-Newton AM, et al. Twenty Year Trends and Sex Differences in Young Adults Hospitalized With Acute Myocardial Infarction. Circulation. Feb 19 2019;139(8):1047-1056. doi:10.1161/circulationaha.118.037137
- Gulati R, Behfar A, Narula J, et al. Acute Myocardial Infarction in Young Individuals. Mayo Clin Proc. Jan 2020;95(1):136-156. doi:10.1016/j.mayocp.2019.05.001
- Jortveit J, Pripp AH, Langørgen J, Halvorsen S. Incidence, risk factors and outcome of young patients with myocardial infarction. Heart. Sep 2020;106(18):1420-1426. doi:10.1136/heartjnl-2019-316067
- Zasada W, Bobrowska B, Plens K, et al. Acute myocardial infarction in young patients. Kardiol Pol. 2021;79(10):1093-1098. doi:10.33963/KP.a2021.0099
- Yang J, Biery DW, Singh A, et al. Risk Factors and Outcomes of Very Young Adults Who Experience Myocardial Infarction: The Partners YOUNG-MI Registry. Am J Med. May 2020;133(5):605-612.e1. doi:10.1016/j.amjmed.2019.10.020
- Richards JR, Bing ML, Moulin AK, et al. Cannabis use and acute coronary syndrome. Clin Toxicol (Phila). Oct 2019;57(10):831-841. doi:10.1080/15563650.2019.1601735
- Li XR, Zuo HJ, Yang HX, et al. [Clinical characteristics and prognosis of young (<35 years) patients with acute ST-segment elevation myocardial infarction]. Zhonghua Xin Xue Guan Bing Za Zhi. Nov 24 2021;49(11):1124-1129. doi:10.3760/cma.j.cn112148-20210805-00672
- Ray KK, Ference BA, Séverin T, et al. World Heart Federation Cholesterol Roadmap 2022. Glob Heart. 2022;17(1):75. doi:10.5334/gh.1154
- Delgado GE, Krämer BK, Siekmeier R, et al. Influence of smoking and smoking cessation on biomarkers of endothelial function and their association with mortality. Atherosclerosis. Jan 2020;292:52-59. doi:10.1016/j.atherosclerosis.2019.11.017
- Robert-Koch-Institut. Lyme-Borreliose. RKI-Ratgeber. Accessed 03.04.2023, https://www.rki.de/DE/Content/Infekt/EpidBull/Merkblaetter/Ratgeber_LymeBorreliose.html#doc2398672bodyText6
- Institut RK. Lyme-Borreliose. Accessed 03.04.2023, https://www.rki.de/DE/Content/Infekt/EpidBull/Merkblaetter/Ratgeber_LymeBorreliose.html#doc2398672bodyText6

