Intravenous vs. Oral Iron Therapy in CKD Anemia
Anemia of the Chronic Kidney Disease: A Comparision Between Oral and Intravenous Iron Therapy Combined with Erythropoietin
Sadat Memon1, Sumeira Naeem Khan2, Sophia Raza Laghari3, Sawaira Hussain4, Mashkoor Ahmed Ansari5, Ashique Ali Arain6
- Sadat Memon MBBS, M. Phil (Pharmacology), Assistant Professor, Department of Pharmacology, Liaquat University of Medical & Health Sciences, Jamshoro
- Sumeira Naeem Khan MBBS, M. Phil (Pharmacology) Lecturer, Department of Pharmacology, Liaquat Institute of Medical & Health Sciences LUMHS, Thatta
- Sophia Raza Laghari MBBS, Lecturer, Department of Pharmacology, Bilawal Medical College, Jamshoro
- Sawaira Hussain MBBS, Lecturer, Department of Pharmacology Liaquat Institute of Medical & Health Sciences LUMHS, Thatta,
- Mashkoor Ahmed Ansari MBBS, M. Phil (Pharmacology)Associate Professor, Department of Pharmacology, Liaquat University of Medical & Health Sciences, Jamshoro,
- Dr Ashique Ali ArainMBBS, MCPS (Family Medicine), M. Phil (Pharmacology), Consultant Family Physician, Assosiate Professor, Department of Pharmacology, Liaquat Institute of Medical & Health Sciences LUMHS, Thatta, Sindh, Pakistan
OPEN ACCESS
PUBLISHED: 30 June 2025
CITATION: Memon, S., Khan, SN., et al., 2025. Anemia of the chronic kidney disease: A Comparision Between Oral and Intravenous Iron Therapy Combined with Erythropoietin. Medical Research Archives, [online] 13(6). https://doi.org/10.18103/mra.v13i6.6722
COPYRIGHT: © 2025 European Society of Medicine. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
DOI: https://doi.org/10.18103/mra.v13i6.6722
ISSN 2375-1924
ABSTRACT
Background: Anemia is a common and significant complication in chronic kidney disease (CKD), largely due to iron deficiency and reduced erythropoietin production. This study aimed to compare the efficacy of oral versus intravenous iron supplementation, each combined with subcutaneous recombinant human erythropoietin (rHuEPO), in improving iron status and anemia in patients with chronic renal failure (CRF).
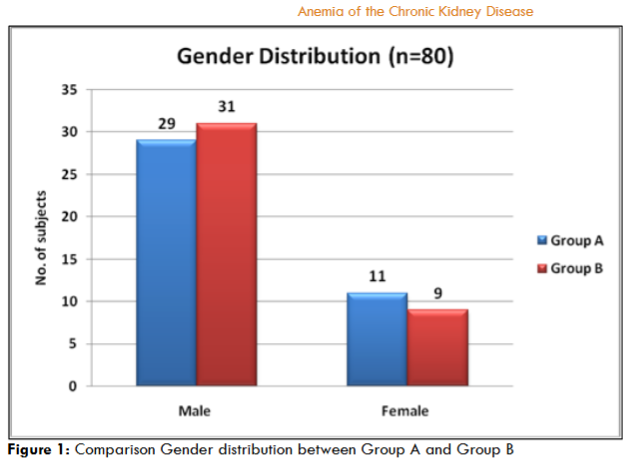
Methods: A total of 8 patients of CRF were included based on inclusion and exclusion criteria and divided into 2 groups. Group A received oral ferrous sulfate with subcutaneous (rHuEPO) and Group-B on intravenous Iran Dextran along with subcutaneous (rHuEPO). Hemoglobin and transferrin saturation (TSAT) were measured at baseline and after six months. Gender distribution was comparable in both groups.
Results: Both groups showed significant increase in hemoglobin and TSAT levels over six months (P=0.001), However, the increase was significantly higher in Group B. At six months, mean TSAT was 39.80±1.05% in Group B versus 26.96±0.95% in Group A (p=0.001), indicating superior efficacy of IV iron dextran in repleting iron stores.
Conclusion: IV Iron dextran, when combined with rHuEPO, is more effective than oral iron in improving anemia and iron status in CRF patients.
Keywords: Chronic Renal Failure, Iron, Erythropoietin, Anemia
Introduction:
Chronic kidney disease (CKD) is a growing global health concern, affecting approximately 13% of the U.S population. Its rising prevalence is closely linked to conditions such as diabetes mellitus and hypertension. Managing CKD presents a significant challenge for general practitioners, especially as symptoms often overlap with other medical conditions many patients are only referred to nephrologist at advanced stages, when options like kidney transplantation become necessary. CKD is marked by progressive renal structural damage and proteinuria, with disease severity often assessed through glomerular filtration rate (GFR) measurements.
Anemia in chronic kidney disease (CKD) is typically normocytic and normochromic, resulting from reduced red cell parameters such as hemoglobin or hematocrit. According to WHO, anemia is defined as hemoglobin <13g/dl in men and postmenopausal women, and <12g/dl in menopausal women. It affects nearly 50% of CKD patients and becomes more prevalent as kidney function declines, with up to 75% of dialysis patients experiencing anemia.
Chronic kidney disease (CKD) is strongly linked with transferrin saturation (TSAT), serum creatinine and blood urea nitrogen (BUN) levels. TSAT is a key marker of iron status and reduced levels are associated with higher mortality in CKD patients. Therefore, regular assessment of TSAT, along with serum creatinine and BUN, is essential for effective disease management. Transferrin, is a liver-derived glycoprotein, transport iron in the plasma and helps prevents iron-induced oxidative damage. TSAT reflects iron availability, normally around 33%. In CKD, TSAT <20% with low ferritin levels indicates absolute deficiency. Optimal erythropoiesis occurs at TSAT >30% with dialysis guidelines recommending a 30-50% TSAT target.
Serum creatinine and Blood Urea Nitrogen (BUN) are key indicators of kidney function. Creatinine is a byproduct of muscle metabolism, is commonly used to assess the severity and stage of chronic kidney disease (CKD). BUN, derived from protein catabolism in the liver offers a rough estimate of renal function but may also be influenced by non-renal factors such as diet, hydration and catabolic states. Both tests are essential for early detection, staging and monitoring of CKD progression, enabling timely intervention to prevent complications and delay end stage renal disease. This study aims to evaluate and compare the effects of Oral and Intravenous Iron therapy on TSAT, Scr and BUN in CKD patients receiving rHuEPO, thereby contributing to more informed clinical decisions regarding anemia management in renal failure.
Methodology:
This prospective, comparative interventional study was conducted in the department of pharmacology and therapeutic, LUMHS Jamshoro, in collaboration with the Department of Urology Liaquat University Hospital Hyderabad and Jamshoro. A total of 80 Patients with chronic renal failure (CRF) and anemia on conservative treatment were selected from the urology units of LUH Hyderabad and Jamshoro from April 2016 to September 2017. The sample size was calculated using Rao soft calculator with 5% margin of error and 95% confidence level. All patients were divided into two equal groups of 40 patients each, using a simple random sampling technique. Group A patients received Oral Ferrous Sulfate 200mg thrice a day, while Group B patients were administered intravenous Iron dextran (100mg elemental Iron) twice a month, diluted in 200ml normal saline and infused over one hour after sensitivity testing. All patients in both groups received Recombinant Human Erythropoietin (200 IU) subcutaneously twice weekly for three months. The study duration was six months after approval from the research ethics committee. Inclusion criteria comprised patients aged 25 years or older, known cases of CRF with microcytic hypochromic anemia (Hb 5-8g/dl) on conservative treatment. Patients with other causes of anemia, recent androgen therapy, coronary artery disease or uncontrolled hypertension were excluded. Blood samples were collected and analyzed for transferrin saturation (TSAT), blood urea nitrogen (BUN), and serum creatinine (Scr) at baseline and monthly intervals. Data were analyzed using SPSS version 16 (IBM, USA). Continuous variables were expressed as Mean ± Standard Error of Mean and compared using Student’s t-test, while categorical variables were analyzed as frequency and percentages. A p-value ≤ 0.05 was considered statistically significant.
Results:
Out of 80 CRF patients, Group A had 29 males (72.5%) and 21 Females (27.5%) while the Group B had 31 males (77.5%) and 9 females (22.5%)
.
At baseline, Transferrin saturation (TSAT) was comparable between Group A (13.91±0.52%) and Group B (13.54±0.50%; P=0.60). after 6 months, TSAT significantly increased in both groups (P=0.001), with a greater rise observed in Group B (39.80±1.05%) compared to Group A (26.96±0.95%; P=0.001)
| Parameters | Day 0 | After 3 months | After 6 months | P-Value |
|---|---|---|---|---|
| Hb.%-Group-A | 6.73±0.20 | 8.93±0.14 | 11.24±0.11 | 0.0001 |
| Hb.%-Group-B | 6.63±0.19 | 8.92±0.19 | 11.98±0.84 | 0.0001 |
| Iron-Group-A | 76.38±1.68 | 91.52+1.83 | 105.43±3.26 | 0.0001 |
| Iron-Group-B | 73.28±1.72 | 102+2.03 | 138.63±0.91 | 0.0001 |
| TIBC-Group-A | 450.20± 0.49 | 401.31+ 6.14 | 309.23+ 9.32 | 0.0001 |
| TIBC-Group-B | 449.62± 0.87 | 321.27 +3.23 | 245.05 +4.19 | 0.0001 |
| TSAT-Group-A | 13.91± 0.52 | 19.25+0.46 | 26.96 ± 0.95 | 0.0001 |
| TSAT-Group-B | 13.54 ± 0.5 | 19.41+0.31 | 39.8± 1.05 | 0.0001 |
.
Serum creatinine was 3.98±0.15 mg/dL in Group A and 3.95±0.16 mg/dL in Group B at baseline (P=0.88), and 3.60±0.16 vs. 3.71±0.17 mg/dL at six months (P=0.67). The difference between different parameters at day-0, after 3 months and after 6 months was statistically significant represented by table-1 in details.
Discussion:
This study evaluated the comparative efficacy of intravenous iron dextran versus oral ferrous sulfate in improving anemia among CKD patients receiving (rHuEPO). The findings demonstrate a significantly greater rise in hemoglobin levels in the intravenous iron group over six months, suggesting superior iron availability and erythropoietic response. These results are consistent with previous studies indicating that intravenous iron is more effective than oral supplementation in overcoming functional and absolute iron deficiencies common in CKD, particularly in patients undergoing erythropoietin therapy. TSAT levels significantly improved in both groups by the sixth month; however, the increase was markedly greater in patients receiving intravenous iron dextran compared to oral iron therapy. This indicates enhanced iron saturation with intravenous administration in CKD patients. Our findings align with previous studies, such as those by Tobli et al. and Ponikowski et al. which highlight the superior efficacy of intravenous iron in restoring iron stores. The combination of IV iron and (rHuEPO) may therefore be a more effective approach for managing anemia in CKD, potentially reducing associated morbidity and mortality.
Ratna et al. stated that in the FIND-CKD trial, intravenous ferric carboxymaltose led to a significant increase in TSAT, with values rising from a mean of 10.71% to 24.11% after treatment. A previous study by Jenq et al demonstrated that there was no significant effect of long-term oral versus intravenous therapy on parameters like serum creatinine and blood urea nitrogen. These finding were consistent with our study’s findings. The research by Pisani et al does not report any change in serum creatinine and BUN during the study period. This is similar to our finding.
Conclusion:
The intravenous iron therapy combined with erythropoietin is more effective as compared to oral Iron therapy combined with erythropoietin in the treatment of the anemia of the chronic renal failure.
References:
- Coresh J, Selvin E, Stevens LA, Manzi J, Kusek JW, Eggers P, et al. Prevalence of chronic kidney disease in the United States. J Am Med Assoc. 2007;298(17):2038–47.
- Executive Summary. American Journal of Kidney Diseases. 2006;47(3). https://pubmed.ncbi.nlm.nih.gov/16678659/
- Levey AS, Eckardt KU, Tsukamoto Y, Levin A, Coresh J, Rossert J, et al. Definition and classification of chronic kidney disease: A position statement from Kidney Disease: Improving Global Outcomes (KDIGO). Kidney Int 2006;67(6):2089–100.
- Besarab A, Levin A. Defining a renal anemia management period. American Journal of Kidney Diseases. 2000;36(6). https://pubmed.ncbi.nlm.nih.gov/11118154/
- McClellan W, Aronoff SL, Bolton WK, Hood S, Lorber DL, Tang KL, et al. The prevalence of anemia in patients with chronic kidney disease. Curr Med Res Opin. 2004;20(9):1501–10.
- Gaweda AE. Markers of Iron Status in Chronic Kidney Disease Diagnosing Iron Deficiency. Hemodial Int. 2017;21(1):S21. https://pmc.ncbi.nlm.nih.gov/articles/PMC6247786/
- Huebers HA, Finch CA. The physiology of transferrin and transferrin receptors. 1987;67(2):520–82.
- Kamal A. estimation of blood urea (bun) and serum creatinine level in patients of renal disorder. 2014;4. http://www.cibtech.org/jls.htm
- Gaitonde DY, Cook DL, Rivera IM, Eisenhower DD. Chronic Kidney Disease: Detection and Evaluation. Am Fam Physician. 2017;96(12):776–83.
- Toblli JE, Di Gennaro F. Switching patients with non-dialysis chronic kidney disease from oral iron to intravenous ferric carboxymaltose: Effects on erythropoiesis-stimulating agent requirements, costs, hemoglobin and iron status. PLoS One. 2015;10(4). https://pubmed.ncbi.nlm.nih.gov/25928811/
- Ponikowski P, Filippatos G, Colet JC, Willenheimer R, Dickstein K, Lüscher T, et al. The impact of intravenous ferric carboxymaltose on renal function: An analysis of the FAIR-HF study. Eur J Heart Fail. 2015;17(3):329–39.
- Ratna palit dakrskrsjp. iron status in anemia of chronic kidney disease (ckd) stage-v and its improvement with intravenous iron supplementation. international journal of pharma and bioscience. 2014 Jul;5(3):91–7.
- Jenq CC, Tian YC, Wu HH, Hsu PY, Huang JY, Chen YC, et al. Effectiveness of oral and intravenous iron therapy in haemodialysis patients. Int J Clin Pract. 2007;62(3):416–22.
- Pisani A, Riccio E, Sabbatini M, Andreucci M, Del Rio A, Visciano B. Effect of oral liposomal iron versus intravenous iron for treatment of iron deficiency anaemia in CKD patients: a randomized trial. Nephrology Dialysis Transplantation. 2015;30(4):645–52.

