Risk Factors for Dural Tears in Spinal Surgery
Risk Factors for Dural Tears in Spinal Surgery: A Prospective Multicenter Registry Study of 1,853 Cases
Masahiro Hirahata ¹, Muneyoshi Fujita ¹, Takahiro Inui ², Keisuke Ishii ², Tatsuhisa Takekawa ², Hirotaka Kawano ¹, Tomoaki Kitagawa ¹
¹ Department of Orthopaedic Surgery, Teikyo University School of Medicine, Tokyo, Japan
² Trauma and Reconstruction Center, Teikyo University Hospital, Tokyo, Japan
OPEN ACCESS
PUBLISHED: 31 July 2025
CITATION Hirahata, M., Fujita, M., et al., 2025. Risk Factors for Dural Tears in Spinal Surgery: A Prospective Multicenter Registry Study of 1,853 Cases. Medical Research Archives, [online] 13(7). https://doi.org/10.18103/mra.v13i7.6754
COPYRIGHT © 2025 European Society of Medicine. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
DOI: https://doi.org/10.18103/mra.v13i7.6754
ISSN 2375-1924
Abstract
Introduction: Dural tear (DT) is one of the most common complications in spinal surgery. High-quality cohort studies were needed to identify risk factors for DT, but accurate data are currently lacking. The purpose of this study was to clarify the predictors of DT through a prospective cohort study with a low dropout rate.
Methods: In this prospective multicenter cohort study in Japan, a registry was established to collect information about patients undergoing spinal surgery between July 1, 2020 and June 30, 2021 at 10 hospitals. Clinical features, laboratory data, and operative factors were collected from the database. Risk factors were analyzed by comparing DT and non-DT groups.
Results: A total of 1,853 patients were enrolled. There were 81 cases with unintended DTs (4.4%; DT group) and 1,772 cases without DTs (non-DT group). Multivariate analysis revealed that old age, rheumatoid arthritis, and non-attending surgeon as the operator were significant risk factors for DTs.
Conclusions: The incidence of DTs in spinal surgery was 4.4%, and identified risk factors were old age, rheumatoid arthritis, and non-attending surgeon as the operator.
Keywords
dural tear, spinal surgery, risk factors, prospective study, cohort study
Introduction
Dural tear (DT) is one of the most common complications in spinal surgery. It can lead to cerebrospinal fluid pressure syndrome, cerebral spinal fluid leakage, and epidural hematoma after surgery. In rare cases, serious complications such as cerebral hemorrhage and meningitis can occur due to DT.
The reported incidence of DTs ranges from 2% to 20%. Yoshihara and Yoneoka reported the risk factors for DT in the United States based on clinical data obtained from the Nationwide Inpatient Sample for 2009. Imajo et al. found that DT was the most frequently occurring complication of spinal surgery in a nationwide survey by the Japanese Society for Spine Surgery and Related Research in 2015, occurring in 661 of 31,380 patients (2.1%). However, the return rate of the questionnaires in that study was low at 28.0%. High-quality cohort studies were needed to identify risk factors for DT, but accurate data are currently lacking. The purpose of this study was to clarify the predictors of DT through a prospective cohort study with a low dropout rate.
Methods
PATIENTS
This prospective multicenter cohort study used a registry that we established to collect information about spine surgeries between July 1, 2020, and June 30, 2021. Ten hospitals in Japan participated. All patients who underwent spinal surgery at these hospitals between July 2020 and June 2021 were enrolled. The inclusion criteria were spinal surgery under general anesthesia and ability to provide informed consent. The exclusion criteria were implant removal, reoperation for complications of initial surgery (e.g., debridement), and intentional or traumatic DTs. The protocol for this registry study was reviewed and approved by the institutional review board of each participating hospital. All patients enrolled in this study provided written informed consent.
Clinical features, such as age, sex, body mass index, hypertension, diabetes mellitus, chronic kidney failure requiring dialysis, Parkinson’s disease, rheumatoid arthritis, regular use of oral steroids, regular use of oral anticoagulant or antiplatelet drugs, and smoking habit were collected from our database. Operative factors were also recorded in the registry, including the type of disease, anatomical location of the disease, surgical procedure, operative time, estimated blood loss, and length of hospital stay.
STATISTICAL ANALYSIS
Risk factor analysis was performed by comparing the DT and non-DT groups. Continuous variables were analyzed using the unpaired two-tailed t-test for normally distributed data and the Mann–Whitney U test for data with a skewed distribution according to the Shapiro–Wilk test. Fisher’s exact test was used for categorical variables. Multivariate logistic regression analysis was performed to identify the significant risk factors for DT by using a forward-backward stepwise procedure (P < 0.1 for entry) with adjustment for old age, sex, overweight, hypertension, diabetes mellitus, hemodialysis, Parkinson’s disease, rheumatoid arthritis, regular use of oral steroids, regular use of anticoagulant or antiplatelet drugs, smoking, ossification of the posterior longitudinal or yellow ligament (OPLL/OYL), metastatic bone tumor, trauma, kyphosis/lordosis, emergency surgery, revision surgery (i.e., a second or third surgery performed at the same spinal levels as the previous surgery), attending surgeon (i.e., surgeons certified by the Japanese Society for Spine Surgery and Related Research) as the operator or assistant, instrumentation surgery, minimally invasive surgery, and use of a navigation system. Operative time and blood loss were omitted because we could not determine whether they were the cause or result of DTs. Then, odds ratios (OR) and 95% confidence intervals (CIs) of the risk factors for DT were calculated. Statistical analyses were performed using SAS 9.4 for Windows (SAS Institute Inc., Cary, NC). A P-value less than 0.05 was considered statistically significant.
Results
At the participating hospitals, 1,951 consecutive patients underwent spinal surgery, of whom 90 were excluded because they did not provide written informed consent or there was no discharge date. Of the remaining 1,861 patients, 8 with intended DTs were excluded. There were no patients with traumatic DTs. Finally, 1,853 patients were included in the analysis, of whom 617 (33.3%) were female. Mean age at surgery was 62.8 (14-98) years. Spinal stenosis was the most frequent type of disease, occurring in 975 cases (52.6%), followed by disk herniation (668, 36.0%) and traumatic spinal fracture (49, 2.6%). The most common procedure was laminectomy (788, 42.5%), followed by herniotomy (632, 34.1%) and posterior decompression and fixation (196, 10.6%). There were 201 patients (10.8%) who received revision surgeries.
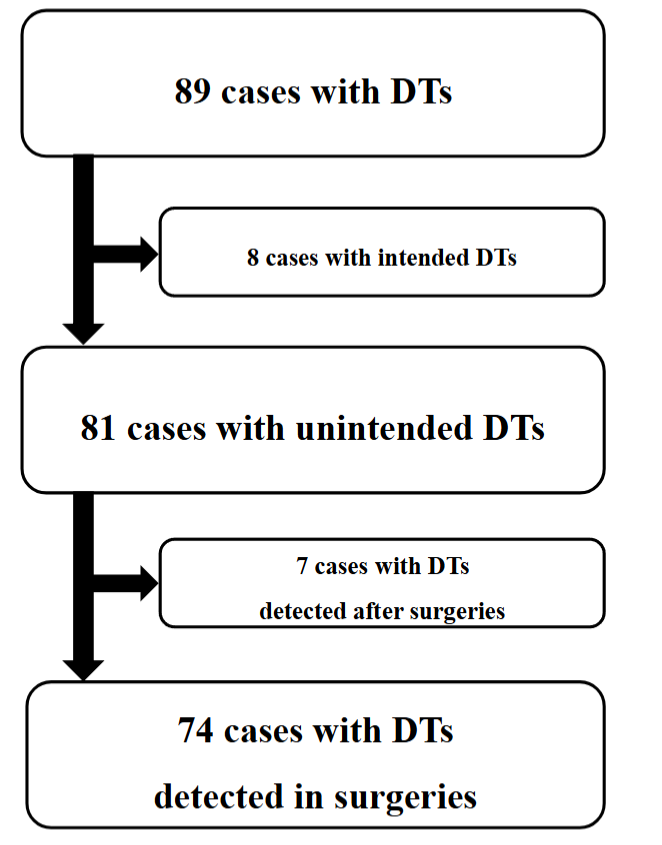
Table 1: Analyzed Variables with Percentages
| All (n = 1853) | Percentage | ||
|---|---|---|---|
| Age, y (min – max) | 63 (14 – 98) | ||
| Old age | 858 | 46.3 | |
| Sex | Female | 617 | 33.3 |
| Male | 1235 | 66.7 | |
| BMI, kg/m2 (min – max) | 23.8 (16.1 – 39.0) | ||
| Overweight | 668 | 36.1 | |
| Diagnosis | Spinal stenosis | 975 | 52.6 |
| Disk hernia | 668 | 36.0 | |
| Traumatic spinal fracture | 49 | 2.6 | |
| Level | Cervical | 301 | 16.2 |
| Thoracic | 53 | 2.9 | |
| Lumbosacral | 1509 | 81.4 | |
| Procedure | Laminectomy | 788 | 36.0 |
| Herniotomy | 632 | 34.1 | |
| Posterior decompression and fixation | 196 | 10.6 | |
| Operative time, minute (min – max) | 80 (15 – 3467) | ||
| Blood loss, mL (min – max) | 10 (10 – 2009) | ||
| Revision surgery | 201 | 10.8 | |
| Inhospitable stay, day (min – max) | 4 (2 – 255) | ||
| FIM, point (min – max) | 125 (18 – 126) | ||
| Death | 4 | 0.2 |
BMI: body mass index; FIM: functional independence measure
The number of patients who had DTs was 89. Of these 89 cases, there were 8 with intended DTs. Thus, there were 81 cases (4.4%) in the DT group and 1,772 cases (95.6%) in the non-DT group. In 7 of the 81 cases, DT was detected after surgery by spinal fluid leakage into the suction drain.
| DT group (n = 81) | Non-DT group (n = 1,772) | P | |
|---|---|---|---|
| Operative time | 164.7 | 99.2 | 0.000 |
| Blood loss | 170.2 | 65.5 | 0.000 |
| Inhospitable stay | 13.2 | 10.0 | 0.165 |
| FIM | 113.3 | 114.7 | 0.773 |
| Death | 1 | 3 | 0.164 |
DT: dural tear; FIM: functional independence measure
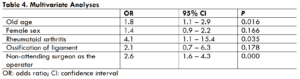
Univariate analyses revealed that old age (P=0.003), female sex (P=0.093), hypertension (P=0.077), rheumatoid arthritis (P=0.025), ossification of ligament (P=0.081), and non-attending surgeon as the operator (P=0.000), as potential risk factors for DTs.
Multivariate analyses revealed that old age (OR=1.8 95% CI: 1.1-2.9, P=0.016), rheumatoid arthritis (OR=4.1, 95% CI: 1.1-15.4, P=0.035), and non-attending surgeon as the operator (OR=2.6, 95% CI: 1.6-4.3, P=0.000) were significant risk factors for DTs.
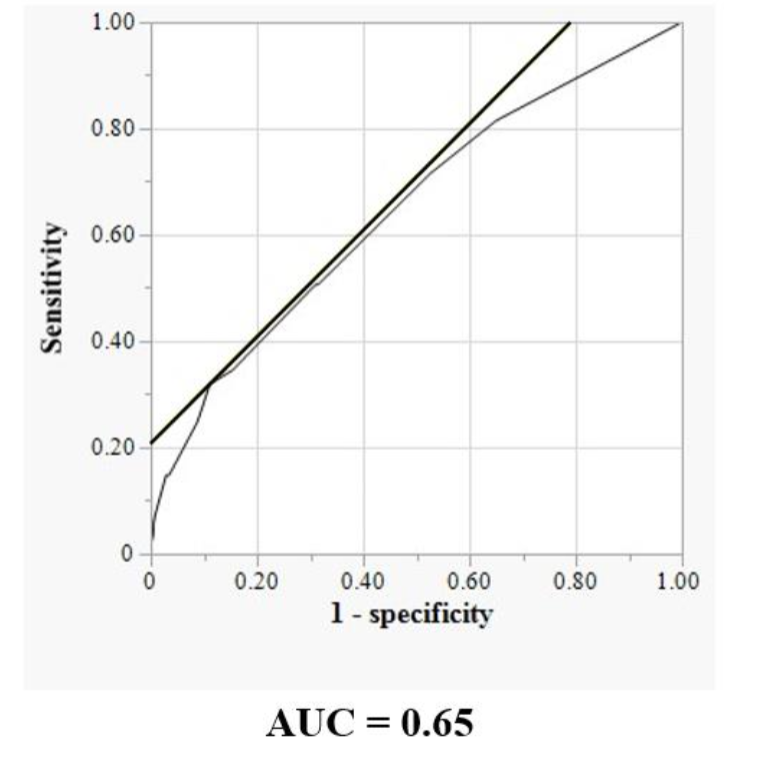
Table 3. Univariate Analyses
| DT group | Non-DT group | P | |||
|---|---|---|---|---|---|
| Old age | 51 | 2.8 | 807 | 43.6 | 0.003 |
| Female sex | 34 | 1.84 | 583 | 31.5 | 0.093 |
| Overweight | 25 | 1.4 | 643 | 34.7 | 0.406 |
| Hypertension | 38 | 2.1 | 651 | 35.1 | 0.077 |
| Diabetes mellitus | 14 | 0.8 | 266 | 14.4 | 0.529 |
| Hemodialysis | 1 | 0.1 | 13 | 0.7 | 0.466 |
| Parkinson disease | 0 | 0.0 | 6 | 0.3 | 1.000 |
| Rheumatoid arthritis | 3 | 0.2 | 12 | 0.7 | 0.025 |
| Steroid | 1 | 0.1 | 22 | 1.2 | 1.000 |
| Anticoagulant or antiplatelet drug | 5 | 0.3 | 105 | 5.7 | 0.812 |
| Smoking | 17 | 0.9 | 352 | 19.0 | 0.777 |
| Ossification of ligament | 4 | 0.2 | 34 | 1.8 | 0.081 |
| Metastatic bone tumor | 1 | 0.1 | 10 | 0.5 | 0.389 |
| Trauma | 2 | 0.1 | 47 | 2.5 | 1.000 |
| Kyphosis or lordosis | 0 | 0.0 | 17 | 0.9 | 1.000 |
| Emergency surgery | 4 | 0.2 | 69 | 3.7 | 0.557 |
| Revision surgery | 9 | 0.5 | 192 | 10.4 | 0.856 |
| Non-attending surgeon as the operator | 25 | 1.4 | 247 | 13.3 | 0.000 |
| Non-attending surgeon as the assistant | 69 | 3.7 | 1591 | 85.9 | 0.191 |
| Instrumentation | 13 | 0.7 | 319 | 17.2 | 0.767 |
| Minimally invasive surgery | 19 | 1.0 | 310 | 16.7 | 0.180 |
| Navigation | 0 | 0.0 | 19 | 1.03 | 1.000 |
DT: dural tear; SD: Standard deviation
Discussion
This study found that the incidence of DTs in spinal surgery was 4.4%, and the identified risk factors were old age, rheumatoid arthritis, and non-attending surgeon as the operator.
The incidence of DTs in this study was generally consistent with previous reports. In a systematic review, Alshameeri and Jasani reported that the incidence of DTs was 5.8% (range, 0.4-15.8%) in 23 clinical studies. According to a nationwide survey conducted by the Japanese Society for Spine Surgery and Related Research in 2015, the incidence of DTs during spinal surgery in Japan was 2.1% (661 of 31,380 patients). We found a higher incidence than in that study. This difference was likely due to the low return rate of the questionnaires in the survey compared with the high rate of coverage in our registry (28.0% vs 99.0%). Thus, our incidence data could be close to actual incidence in Japan.
Old age was identified as an independent risk factor in both univariate and multivariate analyses. Alshameeri and Jasani reported that advanced age was significantly associated with increased risk of DTs in their systematic review. Typical signs of aging, such as narrowing the spinal canal, thickening of the yellow ligament, and osteophyte formation, can lead to incidental durotomy. Furthermore, degenerative shortening of the spine may cause redundant dura, which is more easily caught between the jaws of a Kerrison rongeur. Great care should be taken when manipulating around the fragile dura mater in elderly patients.
In our study, rheumatoid arthritis was identified as a risk factor, consistent with previous reports. In a retrospective review of a prospective database, O’Neill et al. reported that rheumatoid arthritis was a risk factor of DTs in cervical spinal surgery because this inflammatory condition caused more significant adhesions or made the dura more fragile. There was no mention of rheumatoid arthritis in the systematic review on DTs, and many previous studies may not have considered rheumatoid arthritis as a factor. Future studies that include rheumatoid arthritis as a potential risk factor for DTs are desirable.
The surgeon’s training and experience are considered a factor associated DTs in spinal surgery. In the present study, the incidence of DTs was significantly higher in surgeries performed by non-attending surgeons than by attending surgeons. The attending surgeons certified by the Japanese Society for Spine Surgery and Related Research had at least 10 years of experience as physicians. Sin et al. reported that residents caused significantly more DTs during training. McMahon et al. found that the incidence of DTs stabilized at the level of attending physicians. They also reported that the failure of assistants to provide adequate visualization because of insufficient suctioning, retraction, or dural dissection was a factor in DTs. However, our study did not find non-attending surgeons as assistants to be a factor in DTs.
Ossification of ligament has also been reported as risk factors for DTs because it could be accompanied by dural ossification or dural defects, which would then contribute to the occurrence of DTs. In the present study, ossification of ligament was not detected as a risk factor for DTs. A possible reason is that there were fewer cases of OPLL and OYL in the present study than in previous studies. Also, the high rate of posterior decompression for OPLL might explain why no association was observed.
Revision surgery was not a factor in DTs in the present study. According to the systematic review by Alshameeri and Jasani, revision surgery is significantly associated with increased risk of DTs. Revision surgery could result in scar tissue formation at the surgical site, which might obscure the normal anatomy and form adhesions to the dura mater. However, our analysis did not support the argument that scar tissue formation resulted in DTs being likely to occur in reoperations. A possible reason for this is that the surgeon would be more aware of the possibility of incidental durotomy during reoperation and may tend to be more cautious in areas covered with dense scar tissue.
Minimally invasive surgery was not a risk factor for DTs in the present study. In a systematic review of DTs in lumbar degenerative spinal surgery, Ghobrial et al. described durotomy rates in patients who underwent either open or minimally invasive surgical procedures. The durotomy rates did not significantly differ between the two cohorts. Several studies included in Ghobrial’s systematic review had higher durotomy rates in open surgery. These reported results may be attributable to the retrospective design of the studies and a major confounder was that a significantly higher percentage of revision surgery patients underwent open surgery.
The present study has several limitations. First, the data were obtained cross-sectionally in the prospective study. Second, patients with a high risk of DTs might be excluded from the indication for surgery. Third, there might be other risk factors assumed in this study. Despite these limitations, this study contributes to our understanding of risk factors for DTs in spinal surgery and thus to efforts to prevent them.
Conclusions
The incidence of DTs in spinal surgery was 4.4%, and identified risk factors were old age, rheumatoid arthritis, and non-attending surgeon as the operator.
Conflicts of Interest Statement
The authors declare that there are no relevant conflicts of interest.
Funding Statement
None
Acknowledgments
None
References
- Fang Z, Tian R, Jia YT, et al. Treatment of cerebrospinal fluid leak after spine surgery. Chin J Traumatol. 2017;20:81-83.
- Takenaka S, Makino T, Sakai Y, et al. Dural tear is associated with an increased rate of other perioperative complications in primary lumbar spine surgery for degenerative diseases. Medicine (Baltimore). 2019;98:e13970.
- Honegger J, Zentner J, Spreer J, et al. Cerebellar hemorrhage arising postoperatively as a complication of supratentorial surgery: a retrospective study. J Neurosurg. 2002;96:248-254.
- Alluri R, Kang HP, Bouz G, et al. The True Effect of a Lumbar Dural Tear on Complications and Cost. Spine (Phila Pa 1976). 2020;45:E155-e62.
- Alshameeri ZAF, El-Mubarak A, Kim E, et al. A systematic review and meta-analysis on the management of accidental dural tears in spinal surgery: drowning in information but thirsty for a clear message. Eur Spine J. 2020;29:1671-1685.
- Yoshihara H, Yoneoka D. Incidental dural tear in cervical spine surgery: analysis of a nationwide database. J Spinal Disord Tech. 2015;28:19-24.
- Imajo Y, Taguchi T, Yone K, et al. Japanese 2011 nationwide survey on complications from spine surgery. J Orthop Sci. 2015;20:38-54.
- Alshameeri ZAF, Jasani V. Risk Factors for Accidental Dural Tears in Spinal Surgery. Int J Spine Surg. 2021;15:536-548.
- Espiritu MT, Rhyne A, Darden BV 2nd. Dural tears in spine surgery. J Am Acad Orthop Surg. 2010;18:537-545.
- OʼNeill KR, Neuman BJ, Peters C, et al. Risk factors for dural tears in the cervical spine. Spine (Phila Pa 1976). 2014;39:E1015-1020.
- Ghobrial GM, Theofanis T, Darden BV, et al. Unintended durotomy in lumbar degenerative spinal surgery: a 10-year systematic review of the literature. Neurosurg Focus. 2015;39:E8.
- Sin AH, Caldito G, Smith D. Predictive factors for dural tear and cerebrospinal fluid leakage in patients undergoing lumbar surgery. J Neurosurg Spine. 2006;5:224-227.
- McMahon P, Dididze M, Levi AD. Incidental durotomy after spinal surgery: a prospective study in an academic institution. J Neurosurg Spine. 2012;17:30-36.
- Head J, Rymarczuk G, Stricsek G, et al. Ossification of the Posterior Longitudinal Ligament: Surgical Approaches and Associated Complications. Neurospine. 2019;16:517-529.

