Amosy M’Koma
Abstract:
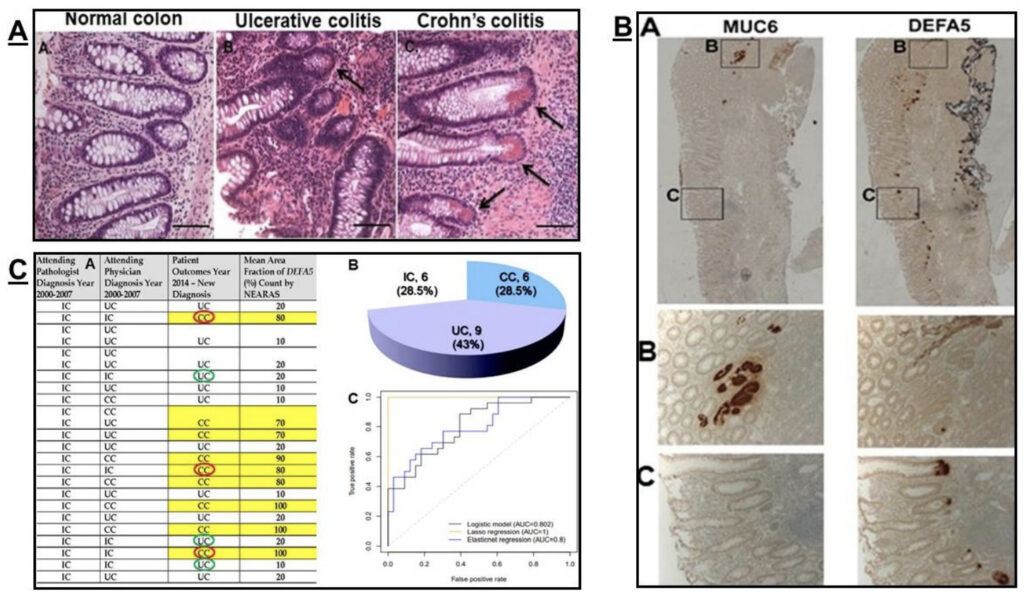
Background: The central medical challenge is the discrimination of predominantly colonic inflammatory bowel disease (IBD), The colitides, into the specific subtypes with high accuracy because it greatly effects surgical care of patients. Innovative, robust evidence links Paneth cell-like cells, apparent crypt-cell like cells (CCLCs), Fig. 1C and Alpha Defensin 5 (DEFA5 also abbreviated as HD5) expansion in the colonic mucosa crypt of Crohn’s colitis (CC) patients. These colonic areas of ectopic ileal metaplasia, positive for Paneth cell markers are consistent and facilitate diagnosis of CC and provide new insight into the etiopathogenesis and differentiation triggers driving colonic IBD. Colon do not have Paneth cells. We sought to find out the source of DEFA5 and whether is co-expressed in ulcer-associated cell lineages (UACL) and/or CCLCs, stained for Mucin 6 (MUC6) and DEFA5; and identified indeterminate colitis (IC) patients their initial biopsies were analyzed by DEFA5 bioassay to either CC or ulcerative colitis (UC) and if in agreement with the outcome ≥14 years later.
Methods: 1) To examine the association between injury to the mucosae of the colonic IBD and emergence of UACL and CCLCs as an active reparative defensive response to ulceration, differentiated lineage analysis by immunohistochemistry (IHC) of on paraffin wax embedded (FFPE) tissue sections from CC stained for MUC6 and DEFA5. 2) Retrospectively, identified 21 patients with indeterminate colitis 2000-2007 and were reevaluated their final diagnosis 2014 after follow-up of mean 8.7±3.7 (range 4-14) years. Their initial biopsies were analyzed by DEFA5 bioassay. Three statistical methods were used: (i) Univariate analysis; (ii) LASSO; and (iii) Elastic net.
Results: CCLCs depicted in mucosal crypt in CC, Fig. 1C complemented with co-localized DEFA5, Fig. 1B. IHC staining of CC for MUC6 and DEFA5 stained in different locations, out from the bases of adjacent crypts and in the crypts, indicating that CCLCs staining DEFA5 is not co-expressed in UCAL, Fig. 1C. DEFA5 is therefore not the genesis of CC, rather a secretagogue of DEFA5-indused specific biomarker(s) that underlie the distinct crypt pathobiology of CC. DEFA5 bioassay authenticated CC/UC among IC cohort with the initial endoscopy biopsy with a positive predictive value of 96 percent. A fit logistic model with group CC vs. UC as the outcome and DEFA5 as independent variable discriminator (not shown here).
Conclusions: Double staining of CCLCs and DEFA5 of IBD patients accurately facilitate CC diagnosis. CCLCs staining DEFA5 is not co-expressed in UACL therefore is not the genesis of CC, rather a secretagogue for specific signature(s) that underlie the distinct crypt pathobiology of CC. CCLCs and DEFA5 in crypt areas with ectopic ileal metaplasia in IC cohort was authenticated into CC with first endoscopy biopsy.