Daily Hand-Off of Chronic Stroke Neurorehabilitation Patients to Expert Clinicians, With Resulting Significant Coordination Improvement: Care Model Development and Implementation
Main Article Content
Abstract
Background: New models of care delivery are necessary to meet workforce needs while delivering expert care in neurorehabilitation. Therefore, we sought to develop and assess the implementation of a new model of care for neurorehabilitation using a 5-member team of therapists (5-Team Model) for the treatment of individuals with chronic stroke, rather than a conventional single-therapist model.
Methods: A mixed methods approach was employed; continuous quality improvement methods and quasi-experimental pre-test/post-test methods were used to assess the effectiveness of the new model.
Six chronic stroke patients participated in an upper limb neurorehabilitation motor learning protocol 5 days/week, 5 hours/day (60 sessions; 300 hours); treatment was administered using the 5-Team Model approach to treatment.
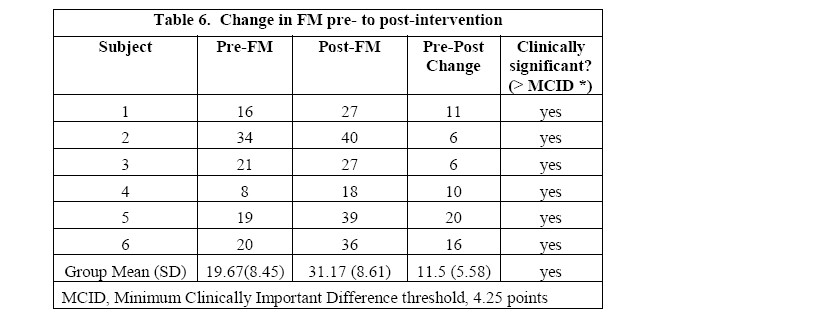
Results: Mean improvement on the Fugl Meyer (FM) was 11.5 points. All six participants demonstrated improvement on Fugl Meyer that was within or beyond the minimal clinically important difference (MCID) range of 4.25-7.25 points for chronic stroke. Results indicated that the 5-Team Model was effective in implementing care.
Conclusions: The 5-Team Model for neurorehabilitation was successfully implemented, with patient hand-off every day to a different therapist; it produced clinically significant improvement on a measure of coordination (FM) which is comparable to or better than prior reports from a standard care model. This new model of care met the needs of the research team workforce for flexibility, while maintaining the level of quality of care. Successful implementation required addressing a series of hindering factors in an iterative manner and enhancing promoting factors. These elements included the context within which the change was implemented, the methods used in implementing the change, the evidence that the change was successful, and communication that the change was successful. The context requirements included existing framework and participating model members who were willing to exert the required effort for success, model champions. This high level of enthusiastic participation along with strong leadership contributed to long-term success, sustainability.

BACKGROUND
Recovery from stroke presents major management challenges to both the stroke survivor and the healthcare system1–7. Some healthcare delivery challenges result from insufficient capacity to support stroke rehabilitation in terms of personnel, space, equipment, and delivery system design1–5. Effective models of stroke care exist and their associated improved outcomes depend upon continuity of care and communication5,6,8,9. However, continuity of care in rehabilitation (i.e. the same physical therapist providing all of the physical therapy care at a given stage of rehabilitation) is becoming increasingly difficult to ensure because of demands for seven day coverage10,11 and work life preferences11. Thsee factors make the traditional model of a “single therapist as provider” less feasible. Because of these difficulties, new models of care delivery are needed for stroke neurorehabilitation1. In fact, because of staffing issues within our own stroke rehabilitation research clinic, it became necessary to develop a new model of care in order to meet the needs of our clinical workforce. A team approach to providing physical therapy services was identified as one such model to meet these demands. One critical component of providing team based care is effective communication12, particularly at the transition point or ‘hand-off of patients’ from one therapist to another12. The main purpose of a good hand-off procedure is to ensure that accurate information concerning the patient’s care is effectively conveyed by one healthcare professional to the next13. The hand-off has been extensively studied in other healthcare settings12,14,15. However, the ‘hand-off’ of patients from one physical therapist to another has not been well-studied, especially with regard to the nature and quality of communication across physical therapists, and the effect on patient recovery of ‘handing off’ patients from day to day. The purpose of this study was to develop and implement a model of stroke neurorehabilitation using a team of five physical therapists (each working on separate days), and to report patient response to therapy in this 5-Team Member model.
METHODS
Study Design
We used a mixed methods approach and followed STROBE guidelines for reporting an observational study. A new care delivery method was developed through continuous quality improvement methods to meet the needs of our Research Program in terms of staffing, and patient response to this model was assessed.
Setting
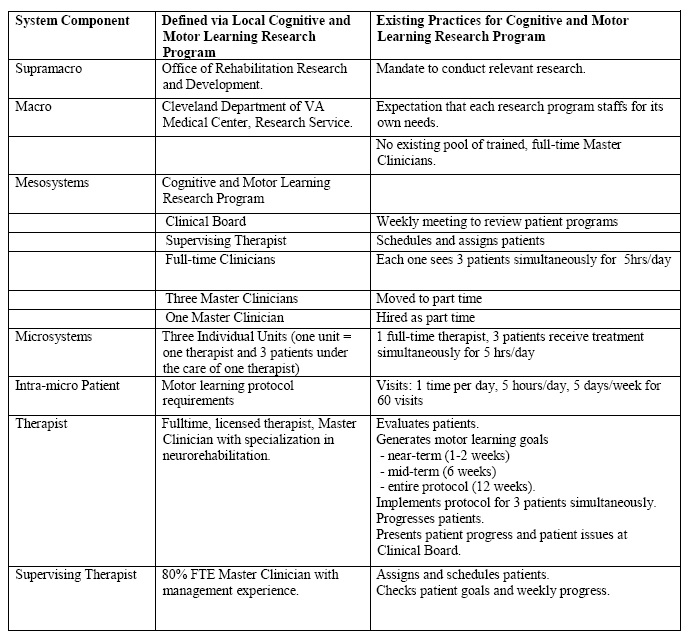
This project was conducted within an established Research Program that had an active clinic similar to an outpatient clinical facility in terms of use of resources and the type of clinical protocols that were administered for testing. The Institutional Review Board of the Cleveland VA of the medical facility oversaw the activities of the Research Program and study participants provided written informed consent to participate in the studies conducted within the Research Program. The initial existing clinical microsystem (individual units, each consisting of one therapist and three patients all treated for five hours per day) is the critical level at which the therapist and patient interact (Table 1, adapted from Batalden)16; this is the critical system level because the content of this interaction determines whether the patient will experience recovery of otherwise persistent motor deficits17–19.
Table 1. System components for implementation of 5-Team Model delivering upper limb motor recovery protocol.
Problem definition and preparation for model development
The staffing problems of the research program clinic reflected problems of clinical staffing at large. Specifically, a full-time scope of work from an expert clinician was needed, but it was not possible to locate a full-time therapist; rather, five part-time expert therapists were available to fulfill the scope of work. In the new model, the single therapist-patient relationship was replaced by a daily, rotating therapist-patient relationship which was nested within the mesosystem (neurorehabilitation research clinic setting; Figure 1)16.
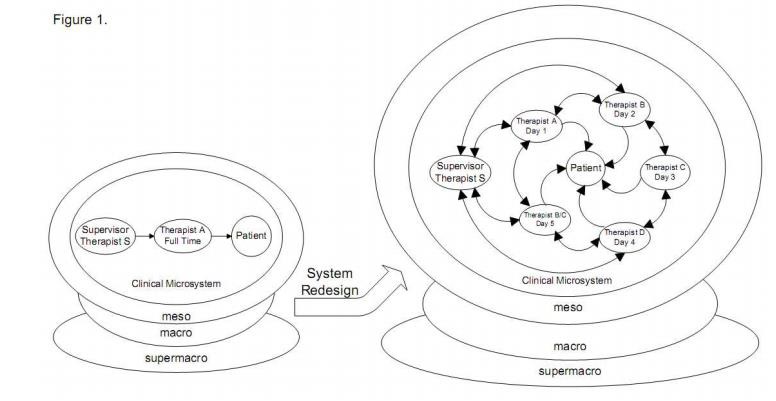
Figure 1. Illustration of the transformation (system redesign) for successful implementation of the 5-Member Team model as an intra-meso component. The figure on the left side is the initial model and the right side illustrates the system redesign.
Development of the Intervention: 5-Team Model
Through continuous quality improvement methods, team members examined the problem, generated the model, implemented the model, and examined the success of the model during implementation. Model development was conducted using an iterative (participatory action research20) approach. Full team meetings were held and individual team members identified any issues they observed in the developing model. A focus group was then used to determine the best way to solve an identified issue, and consensus from the group as a whole was sought. During in-person meetings, all members were given the opportunity to discuss any issues they deemed necessary and notes were recorded and maintained by the program director. Additional methods of communication included group e-mails and small in-person group meetings in dyads and triads.
Preparation for model development
The problem was presented to the team, as follows: “Three patients require receipt of a motor learning protocol, 5 hours/day, 5 days/week for 60 visits. Staffing constraints require that these three patients be seen simultaneously by one clinician on any given day. With potential resources of 4 part-time, treating therapists and one supervisor, what is the best model for delivering care?”
At the initial meeting, participating group members were requested to analyze their own professional resources and their existing individual necessary needs in order to participate in any solution to the problem. Needs included childcare, learning of the protocol, and coverage of the treatment schedule. In a series of dyad and triad meetings, a potential solution was generated for each of these needs.
Model development
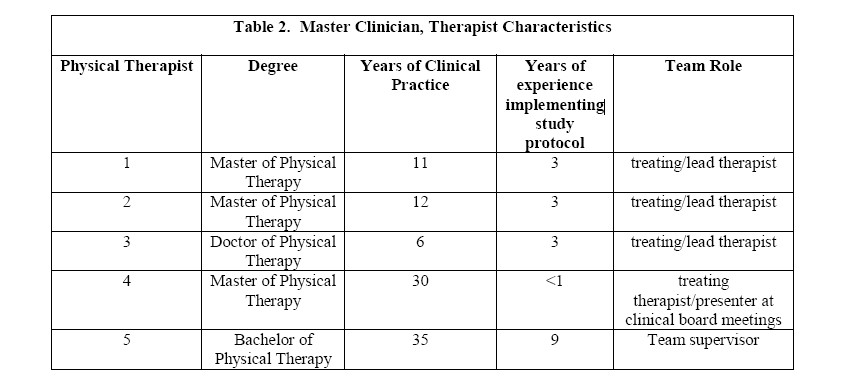
A second meeting was held to arrive at a consensus for the best new model. Having organized themselves to share resources and meet critical needs, they constructed a 5-Team Model: one member would serve as team supervisor, and the remaining four would provide patient care one day per week (two members alternated for the fifth day/week) throughout the duration of a study subject’s participation. Characteristics of the members of the 5-Team Model are provided in Table 2.
Three patients were treated simultaneously in a group. Three different treating therapists each served as the lead therapist for one of the three patients, all of whom were treated simultaneously. Duties of the lead therapist for a given patient included: 1) development of patient goals and a treatment plan; 2) monitoring of that patient’s progress across the week (even though the given patient’s lead therapist was present only one day per week); 3) generating a Clinical Board Meeting report describing progress and goals at pre-/mid-/-post-treatment so that it could be presented to the research program members. The fourth treating therapist agreed to present reports for all three patients at the Clinical Board Meeting (because the others were not present for that meeting).
Communication methods during protocol implementation
At the initial implementation of the new model, an in-person meeting established the responsibilities of each team member. Subsequently, communication was conducted across team members using written patient records, emails, and almost daily discussion with the supervisor, regarding patient progression.
Patient protocol implementation
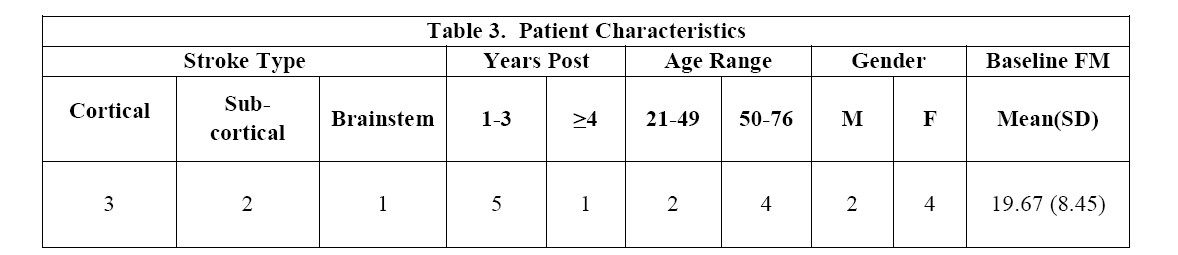
Patient characteristics are provided in Table 3. Financial and resource constraints limited the study sample size to 6 patients, which would allow us to run the 5-Team care model twice. Data from this pilot study could be potentially useful in the design of a future larger study. During the first run, the model could accommodate up to three patients, each of whom received treatment five hours/day, five days/week for 60 visits (3 months duration), using a therapist to patient ratio of 1:3. We repeated this for the second run of the 5-Team care model. With one treating therapist on any given day, the maximum number of patients that could be treated simultaneously by one therapist for five hours on that given day, was three patients, which was tested in prior work18,19. The patients in the treatment group were provided upper limb motor learning and functional training, including practice of coordination, task components and whole functional tasks, both with and without practice-assist technologies (shoulder/elbow robot and surface functional electrical stimulation). The patient treatment protocol is described elsewhere18,19.
Patient performance on a measurement of coordination in response to protocol implementation
The Fugl-Meyer Coordination Scale (FM; a measure of coordination of isolated joint movement)21 was chosen to assess patient response to the intervention. It has been extensively reported in the literature and is recommended for use in experimental studies22. An established MCID range of 4.25-7.25 points has been published for chronic stroke23. Descriptive statistics were generated to determine patient response on FM from pre- to post-intervention.
RESULTS
Accommodating the Innovation into the Local Context: Initial Decisions
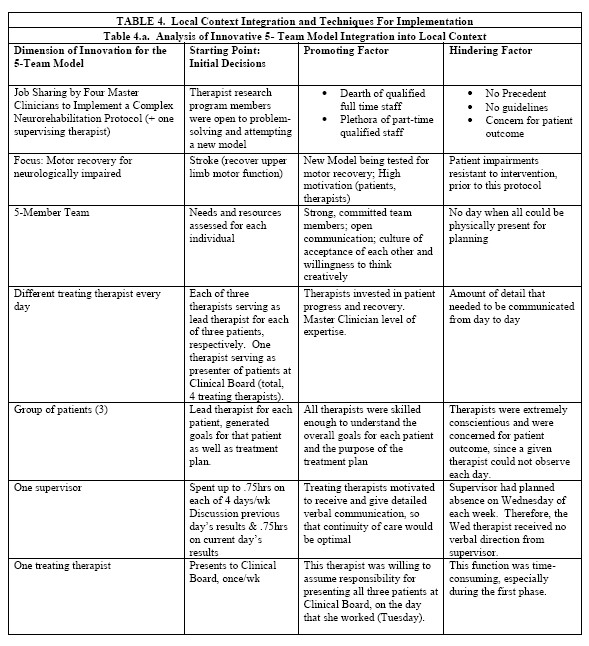
Table 4 provides an analysis of the 5-Team Model including dimensions of innovation, starting points, promoting factors and hindering factors (4.a.), as well as techniques used (4.b). In our analysis, we found that the most important promoting factor was the strong focus by the 5 team members on producing fidelity of the patient protocol in comparison to the one full-time therapist standard model. Other important promoting factors included particular characteristics of all the team members including: high skill level of each Master Clinician, conscientiousness in expending the intellectual effort to do the best job possible, maturity in accepting imperfect communication methods, creativity in generating improved communications across therapists, acceptance of each other’s differences in communication and thinking styles, confidence that speaking up about problems would result in solutions, and flexibility and capability to work in dyads and triads to solve problems as they arose. Finally, the leadership of the Research Program (Mesosystem level16) empowered the team members in that problem identification, problem-solving and implementation of the intervention was entrusted to them.
Implementation of the Innovation and Further Refinement of Processes
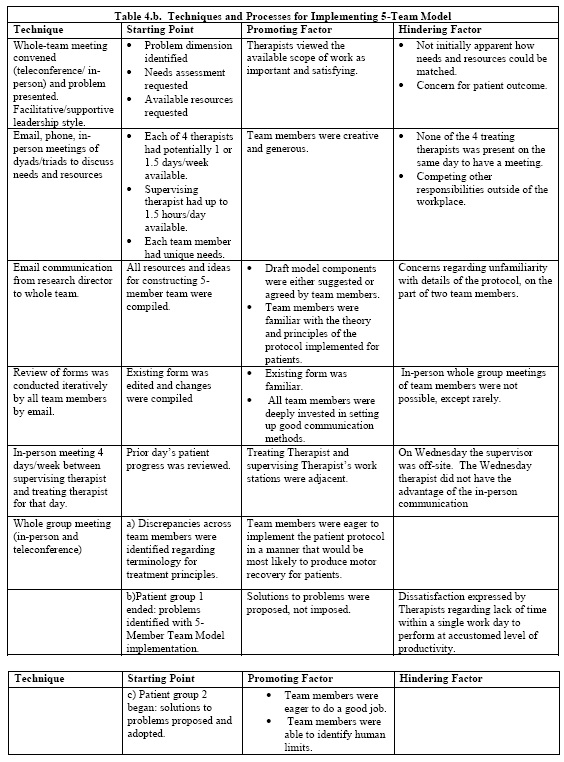
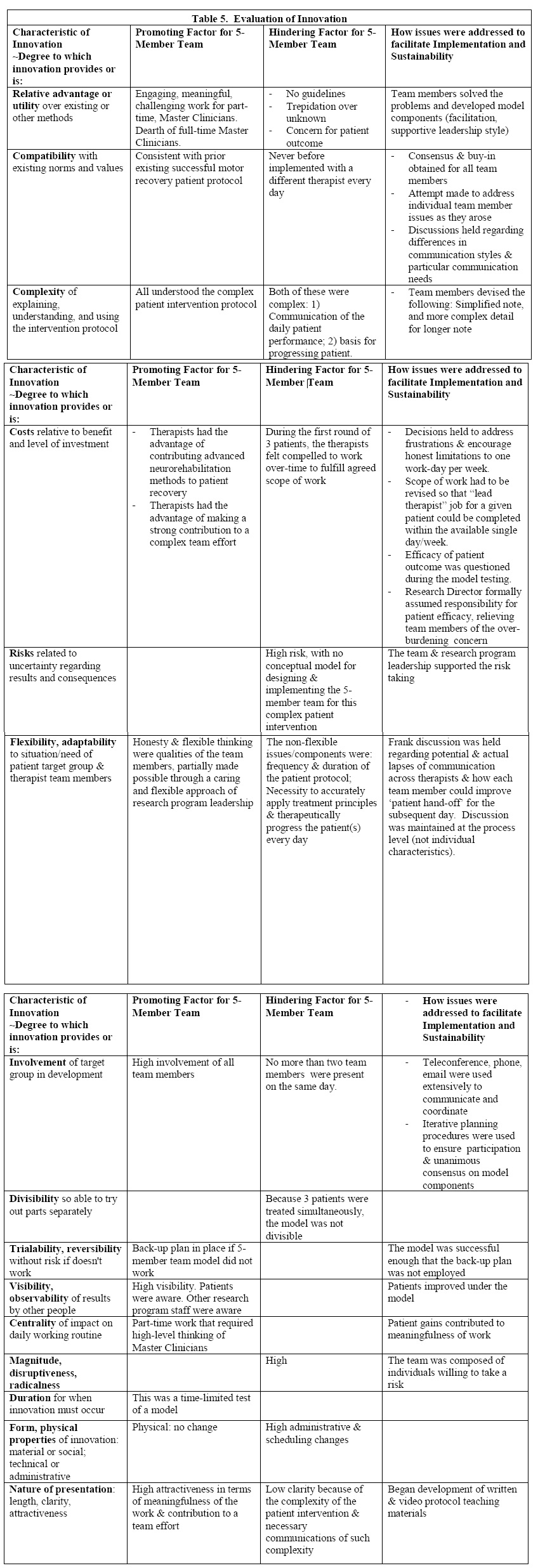
Because the team composition, communication system, and patient treatment were complex, it was important to facilitate an environment in which adjustments and refinements could be made during the implementation process. In order to monitor the implementation process and identify needed adjustments, we utilized the schema by Grol et al.24, which suggests the importance of identifying promoting and hindering processes during the implementation process (Table 5). A variety of communication processes were used during implementation including whole-group and small-group meetings, email communication, and phone meetings.
One of the main hindering factors was that after treatment began, there was no day when the 5 team members were assembled together. A second hindering factor was the complexity of the patient treatment intervention and the need to precisely progress patients each day. The upper limb motor learning protocol is a complex endeavor, which requires considerable expertise from the Master Clinician regarding the conduct of motor learning for those with neurological deficits following stroke. The nature of the patient intervention each day (60-day protocol) is critical; if too little or too much challenge is demanded of the patient, no progress is made. For a 5- Team Model to produce patient recovery, each team member must understand exactly what should be implemented that day, based on the previous day’s achievement by the patient.
Mid-Project Focus Group
After one group of three patients had been treated for 60 visits, a mid-project focus group was held. Team members identified the issues listed below and action steps to address the issues. After the following issues were addressed, a second group of three patients was treated for 60 visits.
A. Issues Identified and action steps generated.
1. Sense of not doing a good job during use of the 5-Team Model; whereas, each therapist had experienced the sure knowledge that she had always previously done a good job using the full-time single therapist standard practice model, and every day patient treatment: This issue stemmed from not seeing the patient every day; not knowing from direct observation whether the treatment provided on a given day was fitting properly into what came before or what came after; and less experience with the specific protocol (2 team members). Assurance was provided by research program leadership that patients had improved as expected and protocol implementation was correct.
2. Poor communication regarding what each patient should be receiving for the day. Even though notes were written by each treating therapist, as planned, this was considered not sufficient by some. For example, because the supervisory therapist was not available on Wednesday, the Wednesday therapist was receiving only written notes; we determined that the verbal communication was critical for particular content, such as the exact set-up for a given exercise, and exact, fine-grained detail of patient response and treatment progression. To address this concern, direct communication was instituted between the Tuesday and Wednesday therapists (no supervisor). In this manner, each therapist’s concerns were identified and resolved. Each dyad from day-to-day refined the manner and detail to be communicated.
3. Different cognitive styles and communication styles were used by each therapist. The cognitive process styles of each therapist became more apparent during discussions of preferred received communications. Across the team members, there was a continuum of successful cognitive processing styles, from highly objective to highly intuitive. Some therapists were entirely comfortable with the communication that they were receiving, and others identified a need for better and more detailed communication. The validity of each style was affirmed. During the discussion, each team member expressed an awareness of additional ways in which she herself could enhance her communication content in order to mesh better with the preferred cognitive process style of the receiver.
4. For each patient in the group, one of the therapists was assigned ‘lead therapist’, with responsibility to generate the treatment plan and a mid- and post-treatment report. This responsibility proved unreasonable since each worked only one day per week. Therefore, for the second round of model implementation, this duty was assumed by the supervising therapist. Team members provided input and assistance to the supervising therapist, in that regard. Adjustment was made also at the Mesosystem level, in that additional time was allocated to the supervising therapist for this duty.
5. Because all team members had to communicate and understand each other’s patient treatment in great detail, it became clear that a common lexicon was not as securely in place as was desired. A meeting was held to better clarify terminology for patient evaluation methods, goal statements, and treatment progression terminology.
Table 5 provides an accounting of the key changes over time and the strategies employed; for this we have used the framework provided by Grol and Wensing’s characteristics of innovations framework24. We found that a critical aspect of innovating a new treatment delivery model was the response of everyone to problems. Flexibility proved a key factor in utilizing continuous quality improvement throughout the process. The changes in process and responsibility described above are examples of the flexibility and support of Mesosystem level leadership. The willingness of team members to provide an honest assessment of problems is evidence of the functional level of the group process employed during the focus group meeting, and the atmosphere of the program itself.
Quantitative Patient Data: Stroke Survivor Response to Treatment
All patients demonstrated a clinically significant gain in FM (Table 6; range of change from pre-treatment to post-treatment: 6-20 points; mean, 11.5 points).
DISCUSSION
Overall, the study contributes in a number ways to the literature. Through mitigation of hindering factors and enhancing promoting factors, we developed and implemented a model that proved sustainable through meeting the work/life balance of part-time highly skilled professionals and delivery of an efficacious motor learning protocol for stroke survivors,
Mitigation of hindering factors
In developing the current treatment model, we initially faced a number of hindering factors, including no precedent and no guidelines for handing off patients, who were in a complex motor learning protocol, to a different therapist each day. The participatory action20 approach was instrumental in the successful mitigation of hindering factors. Basic to this approach is its iterative, continued improvement process, which embodied the therapists’ participatory creative problem-solving and discussions focused to obtain consensus. The success of this approach was borne out in successful mitigation of a number of hindering factors.
One hindering factor was initial concern for patient welfare, fueled by the knowledge that we would be dealing with a known treatment-resistant motor dyscoordination problem in this patient population and that past success had been based on a consistent therapist across 60 treatment sessions19. Additionally, the treatment protocol, by necessity, is a complex series of exercises progressed according to multiple principles of motor learning and based on accurate daily observation and assessment of the individual patient; it requires expert judgement in constructing the custom-designed motor learning exercises for any given day, if the patient is to improve18,19,25. Thus, there was legitimate concern that a different therapist every day would prevent the usual ability of therapists to effectively progress the patients. Indeed, there was no initial basis upon which to trust that the 5-Team Model would improve treatment-resistant upper limb dyscoordination, given that the treating therapists had no experience handing-off patients every day of the week. We mitigated this hindering factor and other hindering factors, through participatory group process, by listening to each clinician’s concern, and by working to address the concern or problem until there was a consensus and level of comfort with moving forward. Notably, this process was iterative, continually applied to assessing the smoothness of operation, patient progress, and effectiveness of solutions to problems.
A second major hindering factor was communication. For example, during the mid-point focus group, we addressed the situation that the treating clinician on Wednesday did not have the advantage of in-person interaction with the supervising therapist and relied only on the written notes from the day prior. In this instance, it was clear that additional communication would strengthen the care delivery provided by this therapist; thus, oral communication was instituted to improve the hand-off by having the clinician from the prior day speak by phone with the Wednesday therapist. Also, to preserve fidelity of the treatment protocol, we instituted more detailed written description of motor task set-up, as well as more detailed notes on achievement of motor coordination milestones on any given day. These two aspects of continuous improvement examples ensured that motor coordination practice was optimally progressed from day to day.
A third example of mitigating the hindering factor of communication entailed a major revision of delegation of responsibilities within the 5-Team Model. By re-allocating report generation, we reduced responsibilities for treating therapists so that each could focus more completely on delivering the intervention and capturing greater detail in written notes and other communications. We increased responsibilities for the therapy supervisor to include generation of reports, both written and oral for presentation to the team (initial care plan, as well as reports at mid- and post-treatment). This change in responsibility was sensible, given the specific knowledge of each patient that the supervisor possessed, and the greater time needed for the treating Master Clinicians to devote to the intervention and communication among themselves during patient hand-offs.
Enhancement of Promoting Factors
Efficacious treatment protocol, demonstrated in prior work with a consistent therapist across multiple treatment sessions. A major promoting factor in the current work was that we sought to administer a treatment protocol with known efficacious results, when a consistent therapist treated the patients across sessions. Therefore, we were attempting to test only a new delivery model of an otherwise efficacious treatment. Our enhancement of this promoting factor was key to the current results which provide evidence that even with daily hand-off to a different therapist, there was faithful implementation of the 5-Team Model for neurorehabilitation. One important measure of success was the equal or better patient response to treatment for the new 5-Team model versus the standard consistent therapist model17–19,26,27. Based on prior basic and clinical science work, we can note specific principles required for successful motor learning, as follows: coordination practice as close to normal as possible28,29; high repetition of productive motor practice30–33; focused attention to the motor practice34; and specificity of training35. Though some of these principles were identified many years ago, they were not tested in the human chronic stroke population in a comprehensive, coherent manner until more recently18,19. More detail of protocol components has been published elsewhere19.
Necessary expertise of neurorehabilitation physical therapists. A second promoting factor in the study was that the therapy team was composed of Master Clinicians. In order for the known successful treatment protocol to produce recovery of coordination, it is necessary for the protocol to be administered by experts in motor learning. The treatment protocol required that the Master Clinician possess the following skills and abilities: accurate assessment of motor performance initially, and on each day of treatment; awareness training for the patient regarding impaired movement and normal coordination; progression of the treatment program each day according to customized motor capability and impairments of the given patient; customized daily progression that is constructed so as to avoid occurrence of too great or too small a challenge that could interfere with motor learning; high repetition of productively practiced motor tasks; single joint movement practice alone and also embedded within practice of complex limb movement and functional tasks19. A Master Clinician applies these treatment components, avoiding any possibility of simply ‘counting repetitions’ and avoiding the use of a general, preconceived exercise prescription. Rather, the Master Clinician is expert in basing upper limb motor learning on daily assessment and custom-designed finely-incrementalized daily progression19.
A critical feature in the Master Clinician skill-set is the employment of a patient centered approach. Others have noted that the Master Clinicians who employ a patient-centered approach, produce greater recovery of function versus therapists with the same number of years of experience, but who do not use a patient-centered paradigm of care36. A patient-centered approach, in this case, entails empowering the patient by teaching the difference between dyscoordination and the normal coordinated movement desired. The importance of this concept in stroke rehabilitation was identified many years ago37, but perhaps not universally applied due to time constraints in the current rehabilitation milieu. In the current treatment protocol, this patient empowerment or ‘awareness training’ is required every day, as the patient progresses through a sequence of coordination practice exercises. In this way, after patient instruction and full understanding, the patient is independent in the practice of that particular exercise, with the sure knowledge of the difference of the desired coordinated movement versus the undesired dyscoordinated movement. In a comparison of Master Clinicians versus others with the same years of experience, others have identified the following additional differences in Master Clinicians: a richer knowledge base; greater use of movement observation; and self-reflection to continually improve their own professional performance36. Even very early papers supported expert decision-making versus prescription-based treatment for stroke survivors, which called out advantages such as more accurate assessment of motor control deficits; ability to synthesize the multiple relevant factors in motor control and motor dysfunction; ability to generate a custom or novel approach and treatment progression for a given patient based on past experience and which is necessary for stroke survivors who each show a unique composite of impairments38,39. Thus, we enhanced the ability of the Master Clinicians to administer the treatment protocol according to their best work; we accomplished this by carefully and effectively addressing their identified obstacles both initially and as obstacles emerged.
Work/life balance and capitalizing on professional experience and Master Clinician qualifications. The initial motivating factor for the study was achieving a satisfying work/life balance for Master Clinicians who needed a reduced work schedule. This was a promoting factor in terms of motivation of the team to work toward achieving the goal. Still, in the current professional field, work/life balance can be a challenge. It is suggested that balance is met when employees experience fulfillment in both work and non-work aspects of their lives40. Work-life balance requires the development and nurturing of a healthy work environment which allows individuals to maintain balance between their personal needs and demands of work40. Healthcare organizations that engage those principles create a happier and more productive work force40. The entire team was motivated to enhance the initial promoting factor of desired work/life balance in order to prevent loss of needed Master Clinicians, to maintain fidelity of the treatment protocol, and to produce recovery of upper limb motor coordination.
Sustainability ingredients which contributed to the success of the 5-Team model. A number of sustainability ingredients were noted during model implementation. First, the Master Clinicians, the therapy supervisor, and the director expressed great satisfaction in contributing to the patient recovery of upper limb function; this level of work satisfaction ensures continued commitment and sustained employment. Second, the team members felt empowered because they developed the overarching model, and in the process, each of their concerns were heard and addressed by the entire team. Consequently, they were motivated to work iteratively through issues that arose as they witnessed amelioration of concerns and problem-solving. Third, in support of good communication, the multi-modal communication processes became a sustainability ingredient. Fourth, the role of the supervising therapist was a critical sustainability ingredient. The supervising therapist was responsible to verbally communicate with the treating therapist for the given day, which served to supplement the written communications between treating therapists. This finding is understandable given the five-hour duration of daily treatment for each patient, along with the complexity of the treatment protocol and criteria for patient progression; these factors made it difficult to capture only in writing, the totality of the needed daily information. Fourth, the 5-Team care delivery model ensured an acceptable work/life balance for all concerned, ensuring sustainability of employment for the Master Clinicians. Fifth, and notably, the patients exhibited excellent recovery of motor coordination equal to or greater than that reported for patients seen by a consistent therapist every day in standard care. With recovery of patient coordination at this level, the protocol and a five-team model is clinically deployable.
CONCLUSIONS
Through continuous quality improvement methods, a new model of care was designed to meet the needs of a highly skilled current workforce for flexibility, while maintaining the level of quality of care. Successful implementation included addressing a series of hindering factors in an iterative manner, as well as enhancing promoting factors. These elements included the context within which the change was implemented, the methods used in implementing the change, the evidence that the change was successful, and communication that the change was successful. The context requirements included existing framework and participating model members who were willing to exert the required effort for success, model champions. This high level of enthusiastic participation along with strong leadership contributed to long-term success, sustainability.
DECLARATIONS
Ethics Approval and consent to participate
The Institutional Review Board of the Cleveland VA oversaw the activities of the Research Program, approved the study, and study participants provided written informed consent to participate in the study.
ACKNOWLEDGEMENTS
This study was supported by the Department of Veterans Affairs, Office of Rehabilitation Research, grants # B3709 and B5080S (JJ Daly, PI). Dr. Susan R Kirsh, M.D. provided valuable consultation.
AUTHORS’ CONTRIBUTIONS
JPM participated in the design and implementation of the study, collection of data and assisted in manuscript drafting. JJD conceived of the study, participated in its design, acquired funding, participated in model development and implementation, data collection and analysis, generated the first draft the manuscript, and edited manuscript iterations and the last draft. MM, KB, JR and MM participated in the design and implementation of the study as well as collection of data. DA participated in the study design, data analysis and assisted in drafting the manuscript.
Article Details
The Medical Research Archives grants authors the right to publish and reproduce the unrevised contribution in whole or in part at any time and in any form for any scholarly non-commercial purpose with the condition that all publications of the contribution include a full citation to the journal as published by the Medical Research Archives.
References
2. Teasell R, Meyer MJ, Foley N, Salter K, Willems D. Stroke Rehabilitation in Canada: A Work in Progress. Top Stroke Rehabil. 2009;16(1):11-19. doi:10.1310/tsr1601-11
3. Gropen T, Magdon-Ismail Z, Day D, Melluzzo S, Schwamm LH. Regional Implementation of the Stroke Systems of Care Model: Recommendations of the Northeast Cerebrovascular Consortium. Stroke. 2009;40(5):1793-1802. doi:10.1161/STROKEAHA.108.531053
4. Abilleira S, Gallofré M, Ribera A, Sánchez E, Tresserras R. Quality of in-hospital stroke care according to evidence-based performance measures: results from the first audit of stroke, Catalonia, Spain. Stroke. 2009;40(4):1433-1438. doi:10.1161/STROKEAHA.108.530014
5. Robinson J. Facilitating earlier transfer of care from acute stroke services into the community. Nurs Times. 2009;105(12):12-13.
6. Gregory PC, Han E. Disparities in Postacute Stroke Rehabilitation Disposition to Acute Inpatient Rehabilitation vs. Home: Findings from the North Carolina Hospital Discharge Database. Am J Phys Med Rehabil. 2009;88(2):100-107. doi:10.1097/PHM.0b013e3181951762
7. Reding MJ, McDowell FH. Focused Stroke Rehabilitation Programs Improve Outcome. Arch Neurol. 1989;46(6):700-701. doi:10.1001/archneur.1989.00520420122034
8. Alonso de Leciñana-Cases M, Gil-Núñez A, Díez-Tejedor E. Relevance of Stroke Code, Stroke Unit and Stroke Networks in Organization of Acute Stroke Care – The Madrid Acute Stroke Care Program. Cerebrovasc Dis. 2009;27(1):140-147. doi:10.1159/000200452
9. Clarke DJ. Achieving teamwork in stroke units: The contribution of opportunistic dialogue. J Interprof Care. 2010;24(3):285-297. doi:10.3109/13561820903163645
10. Rapoport J, Judd-Van Eerd M. Impact of Physical Therapy Weekend Coverage on Length of Stay in an Acute Care Community Hospital. Phys Ther. 1989;69(1):32-37. doi:10.1093/ptj/69.1.32
11. Duncan C, Hudson M, Heck C. The impact of increased weekend physiotherapy service provision in critical care: a mixed methods study. Physiother Theory Pract. 2015;31(8):547-555. doi:10.3109/09593985.2015.1060657
12. Scotten M, Manos EL, Malicoat A, Paolo AM. Minding the gap: Interprofessional communication during inpatient and post discharge chasm care. Patient Educ Couns. 2015;98(7):895-900. doi:10.1016/j.pec.2015.03.009
13. Arora V, Johnson J. A Model for Building a Standardized Hand-off Protocol. Jt Comm J Qual Patient Saf. 2006;32(11):646-655. doi:10.1016/S1553-7250(06)32084-3
14. O’Brien CM, Flanagan ME, Bergman AA, Ebright PR, Frankel RM. “Anybody on this list that you’re more worried about?” Qualitative analysis exploring the functions of questions during end of shift handoffs. BMJ Qual Saf. 2016;25(2):76-83. doi:10.1136/bmjqs-2014-003853
15. Zakrison TL, Rosenbloom B, McFarlan A, et al. Lost information during the handover of critically injured trauma patients: a mixed-methods study. BMJ Qual Saf. 2016;25(12):929-936. doi:10.1136/bmjqs-2014-003903
16. Batalden PB, Nelson EC, Edwards WH, Godfrey MM, Mohr JJ. Microsystems in Health Care: Part 9. Developing Small Clinical Units to Attain Peak Performance. Jt Comm J Qual Saf. 2003;29(11):575-585. doi:10.1016/S1549-3741(03)29068-7
17. Daly JJ, Hogan N, Perepezko EM, et al. Response to upper-limb robotics and functional neuromuscular stimulation following stroke. JRehabilResDev. 2005;42(1938-1352 (Electronic)):723-736.
18. McCabe J, Monkiewicz M, Holcomb J, Pundik S, Daly JJ. Comparison of Robotics, Functional Electrical Stimulation, and Motor Learning Methods for Treatment of Persistent Upper Extremity Dysfunction After Stroke: A Randomized Controlled Trial. Arch Phys Med Rehabil. 2015;96(6):981-990. doi:10.1016/j.apmr.2014.10.022
19. Daly JJ, McCabe JP, Holcomb J, Monkiewicz M, Gansen J, Pundik S. Long-Dose Intensive Therapy Is Necessary for Strong, Clinically Significant, Upper Limb Functional Gains and Retained Gains in Severe/Moderate Chronic Stroke. Neurorehabil Neural Repair. 2019;33(7):523-537. doi:10.1177/1545968319846120
20. Chevalier JM, Buckles DJ. Participatory Action Research: Theory and Methods for Engaged Inquiry. 2nd ed. Routledge; 2019. doi:10.4324/9781351033268
21. Fugl-Meyer AR, Jääskö L, Leyman I, Olsson S, Steglind S. The post-stroke hemiplegic patient. 1. a method for evaluation of physical performance. Scand J Rehabil Med. 1975;7(1):13-31.
22. Santisteban L, Térémetz M, Bleton J-P, Baron J-C, Maier MA, Lindberg PG. Upper Limb Outcome Measures Used in Stroke Rehabilitation Studies: A Systematic Literature Review. Tremblay F, ed. PLOS ONE. 2016;11(5):e0154792. doi:10.1371/journal.pone.0154792
23. Page SJ, Fulk GD, Boyne P. Clinically importance differences for the upper-extremity Fugl-Meyer Scale in people with minimal to moderate impairment due to chronic stroke. Phys Ther. 2012;92:791-798 doi:10.1177/0269215512464795
24. Grol RPTM, Bosch MC, Hulscher MEJL, Eccles MP, Wensing M. Planning and Studying Improvement in Patient Care: The Use of Theoretical Perspectives: Planning and Studying Improvement in Patient Care. Milbank Q. 2007;85(1):93-138. doi:10.1111/j.1468-0009.2007.00478.x
25. Ward NS, Brander F, Kelly K. Intensive upper limb neurorehabilitation in chronic stroke: outcomes from the Queen Square programme. J Neurol Neurosurg Psychiatry. 2019;90(5):498-506. doi:10.1136/jnnp-2018-319954
26. Page SJ, Levine PG, Basobas BA. “Reps” Aren’t Enough: Augmenting Functional Electrical Stimulation With Behavioral Supports Significantly Reduces Impairment in Moderately Impaired Stroke. Arch Phys Med Rehabil. 2016;97(5):747-752. doi:10.1016/j.apmr.2016.01.004
27. Lum PS, Burgar CG, Shor PC, Majmundar M, Van der Loos M. Robot-assisted movement training compared with conventional therapy techniques for the rehabilitation of upper-limb motor function after stroke. Arch Phys Med Rehabil. 2002;83(7):952-959. doi:10.1053/apmr.2001.33101
28. Nudo RJ, Wise BM, SiFuentes F, Milliken GW. Neural Substrates for the Effects of Rehabilitative Training on Motor Recovery After Ischemic Infarct. Science. 1996;272(5269):1791-1794. doi:10.1126/science.272.5269.1791
29. Nudo R, Milliken G, Jenkins W, Merzenich M. Use-dependent alterations of movement representations in primary motor cortex of adult squirrel monkeys. J Neurosci. 1996;16(2):785-807. doi:10.1523/JNEUROSCI.16-02-00785.1996
30. Pascual-Leone A, Torres F. Plasticity of the sensorimotor cortex representation of the reading finger in Braille readers. Brain. 1993;116(1):39-52. doi:10.1093/brain/116.1.39
31. Bütefisch C, Hummelsheim H, Denzler P, Mauritz K-H. Repetitive training of isolated movements improves the outcome of motor rehabilitation of the centrally paretic hand. J Neurol Sci. 1995;130(1):59-68. doi:10.1016/0022-510X(95)00003-K
32. Elbert T, Pantev C, Wienbruch C, Rockstroh B, Taub E. Increased Cortical Representation of the Fingers of the Left Hand in String Players. Science. 1995;270(5234):305-307. doi:10.1126/science.270.5234.305
33. Dean CM, Shepherd RB. Task-Related Training Improves Performance of Seated Reaching Tasks After Stroke: A Randomized Controlled Trial. Stroke. 1997;28(4):722-728. doi:10.1161/01.STR.28.4.722
34. Singer RN, Lidor R, Cauraugh JH. To Be Aware or Not Aware? What to Think about while Learning and Performing a Motor Skill. Sport Psychol. 1993;7(1):19-30. doi:10.1123/tsp.7.1.19
35. Plautz EJ, Milliken GW, Nudo RJ. Effects of repetitive motor training on movement representations in adult squirrel monkeys: role of use versus learning. Neurobiol Learn Mem. 2000;74(1):27-55. doi:10.1006/nlme.1999.3934
36. Resnik L, Jensen GM. Using clinical outcomes to explore the theory of expert practice in physical therapy. Phys Ther. 2003;83(12):1090-1106.
37. Winstein CJ. Knowledge of Results and Motor Learning—Implications for Physical Therapy. Phys Ther. 1991;71(2):140-149. doi:10.1093/ptj/71.2.140
38. Riolo L. Skill Differences in Novice and Expert Clinicians in Neurologic Physical Therapy: Neurol Rep. 1996;20(1):60-63. doi:10.1097/01253086-199620010-00021
39. Bloom BS, Englehart MB, Furst EJ, Hill WH, Krathwohl DR. Taxonomy of Educational Objectives: The Classification of Educational Goals. Handbook 1: Cognitive Domain. Longman; 1956.
40. Shivakumar K, Pujar V. Work Life Balance in the Health Care Sector. Published online 2018. doi:10.13140/RG.2.2.19413.73440