Covid-19: Déjà vu, all over again
Main Article Content
Abstract
Since the first reports of a novel corona virus appearing in Wuhan, China, the expanding pandemic has been treated as an almost unique, unprecedented event. Both academic and popular reports have called it "unprecedented" and at best, "the worst in a century." A brief glance at history argues, however, that there is little unusual about COVID-19 except, perhaps, the rapidity of its global spread. Otherwise its clinical and social realities are familiar, similar to a host of epidemic and pandemic experiences throughout our history. What may be most notable is that our failure to recognize recurring patterns of infectious disease introduction and expansion has caused a general failure to recognize the root sources of microbial evolution and population invasion. And assuming its uniqueness today may prevent us from systemic changes to prepare for the next.

Introduction
We’ve been here before: Hospitals overfull, competing vaccines and multiple viral strains, public closures and public protests. The science has advanced but the realities of pandemic management have not. It’s just that … we forget. In the daily focus on tests, treatment and hopefully prevention we lose the lessons of the past, recreating as if new programs that were previously enacted and understood. Forgetting absolves us of blame for our current failures—“who would have thought?”—while history indicts our contemporary response to challenges.
As an aid to memory and an example of what we have forgotten, this commentary reviews some of the lessons learned in past pandemics and their relation to the current COVID-19 pandemic. The question becomes the reasons for our failure to learn from the past and to apply those lessons to the current pandemic.
The Virus
Clinically, we are shocked whenever an influenza-like retrovirus affects not simply the respiratory system but a patient’s neurology. It’s to be expected, however. Hippocrates described an outbreak in 430 B.C. with symptoms that included respiratory distress and a range of other symptoms. Historians long assumed he conflated the flu with other diseases1 but it is more likely those secondary symptoms where a result of complications from the retrovirus. This was certainly true in the 1918-1918 pandemic whose patients reported a complex of symptoms not unlike those Hippocrates described and patients are experiencing today. The encephalitis lethargica affecting Oliver Sacks’ patients in, Awakenings was only the most serious of complicating neurologies.2
Nor should we be surprised that COVID-19 has spawned new and competing strains of greater transmissibility. It is, after all, what this kind of virus always does: mutate in a manner that assures greater penetration in susceptible populations affected by a range of respiratory and non-respiratory symptoms. In this context it is useful to remember that in the 1940s variant strains of poliomyelitis challenged vaccine researchers just as, today, different strains of Covid-19 challenge public health officials and vaccine developers. Even today we struggle annually to create an influenza vaccine capable of addressing one or another of its three major strains … knowing mutations may bring us yet another we had not prepared for.
Vaccine distribution
There is a long, documented history of vaccine distributions programs whose protocols have been forgotten. In 1947 New York City’s public health officials vaccinated an estimated 6 million persons against smallpox vaccine in one month.3 While the numbers are difficult to verify today,4 what is clear is that it was an extraordinary effort based on protocols then widely known if not employed by every city. A decade earlier a less successful vaccination campaign in New York City was part of a national vaccination program for that disease.
In the 1950s two polio vaccines, an injected vaccine developed by Jonas Salk and later an oral vaccine by James Sabin, were rapidly distributed to school children nation-wide in many countries, including Canada and the United States.5 Together these were, in some cases, simultaneously treatment and elements in tests of vaccine efficacy. And the promise of immunity from these vaccines resulted in a global effort to immunize populations and thus control the virus everywhere.
Like today, issues of efficacy and safety of the competing vaccines were a matter of urgent concern. Hospitals overflowed with young patients whose symptoms included limb paralysis and respiratory distress.6 From Copenhagen to Hong Kong, gymnasiums were converted to makeshift wards in which dental, medical, and nursing students hand-ventilated patients until the crisis was over or cumbersome breathing machines, the so-called “iron lungs,” could be made manufactured and distributed.7 Their development was another example of an emerging urgently needed and rapidly produced on what was thought of as war-time urgency.
In the 1940s there were extraordinary public efforts to increase hospital capacities during that pandemic. Most famous in the US, perhaps, was the rapid, 1944 construction of a polio-dedicated hospital in Hickory, NC.8 It was built mostly by volunteers with publicly donated materials in the midst of a particularly virulent outbreak that existing local hospitals could not handle. Elsewhere as well, when hospital capacity was breached make-shift wards were created in school gymnasiums and elsewhere to assure space for needy patients.
While we treat the emerging alternate strains of COVID-19 as if they are an unexpected challenge any virologist, or medical historian, would say they should have been expected. Bacteria and viruses evolve over time, changing as medicine attempts to limit their effect. This is especially true of retroviruses like influenza and Covid-19. These have long been a problem in vaccine development—think influenza or polio—and remains so today. Perhaps the problem is we’re trained to think of each new microbe as a solitary enemy, a “thing” to be beaten down. Better to think of each as a bacterial or viral cadre whose members share similarities while differing in their parts.
Mortuaries
Since the Black Death and the centuries of plague every pandemic has been accompanied by images of bodies piling up in hospital morgues and mortuary homes. Cities filled with trade and commerce became near mortuaries in which the dead, not the living, were the focus. In the plague centuries from 1300 to 1700 there were no refrigerated trucks to warehouse the fallen. Cremation was not in vogue and grave diggers could not work fast enough to bury the dead. Special burial grounds were created in London and elsewhere when local cemeteries could not handle the volume of newly deceased. Today the same reality is encapsulated in images of refrigerated trucks parked outside hospitals and funeral homes where demand again far outpaces supply. Mortuaries are backlogged and in some countries mass graves have been needed.
Isolation, Quarantine
The silence of city streets once filled with peoples visiting shops now shuttered is a common theme of Covid-19 journalists. But the eyrie absence of urban activity is a recurring theme of pandemic literatures
A hollowing of the urban core during one or another pandemic is as constant an element of pandemic life as the fever and congestion that attend a respiratory virus. In Daniel Defoe’s A Journal of the Plague Year of 1665 he described a silent London near destitute of people.9
Quarantine restrictions were everywhere and those not sick and dying—isolated in dwellings marked with a cross—were cloistered in their homes.10 The rich who could fled the city, of course, carrying the plague with them to country sites. Today the question is not squires retiring to country homes but international travelers. “Snowbirds” from Canada seek to the warmth of Florida; international students seek easy travel to their homes; business folk seek to attend distant meetings. All promote the potential for viral spread.
In the poliomyelitis years of my early youth in the 1950s I remember when we as children were not permitted to leave our homes to shop or visit local swimming pools. People were afraid, some into the late 1950s, to attend weddings and other public gatherings. Like the aftershocks of an earthquake, the cautions begun during a pandemic can reverberate long after the major incidence is over.
Economics vs. public health
There is nothing new in the cavils of those sceptical of lockdowns, quarantines and the interruption of commerce that results. In the past many argued, as have some today that in a pandemic the most important thing is the economy, not the people themselves. In 1831, for example, Lancet authors attacked the idea of a British quarantine to stop the importation of cholera from continental countries.11 Better a bit of cholera, they concluded, than an expensive reduction in national manufacturing and trade. The quarantine orders were withdrawn and in the pandemic that followed—the first of seven major cholera epidemics—more than 50,000 Britons died.
U.S. President Donald Trump followed this rather inglorious tradition, insisting for months that “the cure can’t be worse than the disease” and that COVID-19 was an inconvenience while aggressive measures to contain the virus would be a financial disaster. Shop owners in cities argue against restrictions, seeking exemptions for everything from hair salons to supermarkets. In some regions, officials insist that while the pandemic is real that measures to contain it must not forget the primary needs of the businesses that provide jobs and promote the economy at large.
The question, shorn of ambiguities—then and now—is whether the responsibilities of government are first and foremost the protection of the economy and its revenues or the health and welfare of the people. There is a history to this recurring debate. If it was the latter then attention had to be paid to the living conditions of the poor. As Christopher Hamlin tells it in his Public Health and Social Justice in the Age of Chadwick, reformers realized that the abysmal living conditions of the poor made them more vulnerable to a range of infectious and endemic infectious diseases.12 Radical physicians and social reformers insisted that if infectious diseases were to be tamed for the benefit of all then better living conditions for the most vulnerable must be a priority.
The argued, often anecdotally, income inequality and its attendant causes resulted in the increased incidence of infection among the marginal, poor, and racialized communities. The difference between then and now is that digital data and mapping have allowed us to precisely picture the relationship between higher disease rates in poorer, often ethnic communities whose members typically work in poorly paid but critical service areas. What had been the anecdotal assertion of physicians in the 19th century has become a part of the dashboard maps of Covid-19 activity in many towns and cities.13
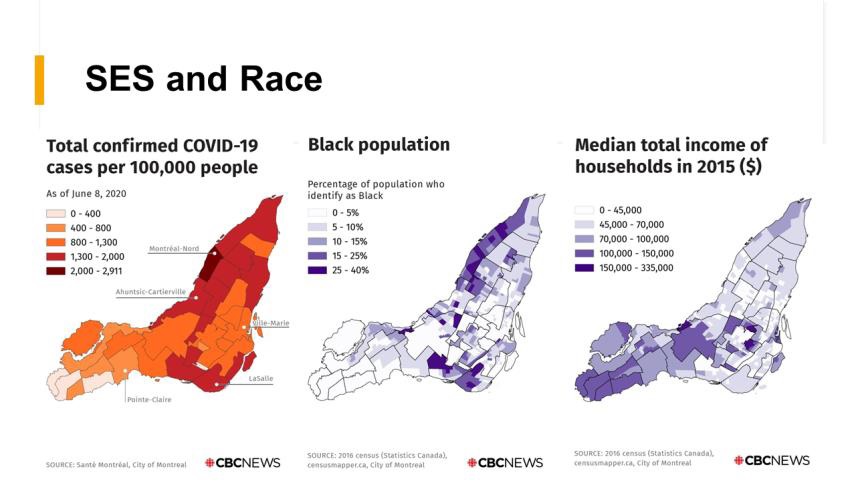
Figure 1. This map produced by CBC News in 2020 used official sources to describe the degree to which COVID-19 infections were highest in poorer and racialized communities in Montreal, Canada (Map courtesy Leah Rosencrantz).14 Similar studies, with attendant graphics, have been produced in many other cities.15
Preparation
Pandemics always catch us unaware and unprepared. This is true historically and it is true today. It is not as if we were not warned. After the 2002-2004 SARS (Severe Acute Respiratory Syndrome) epidemic local and national governments, as well as the World Health Organization developed plans to prepare for future pandemics. When it did not appear, those plans were shelved and the resources allocated to pandemic preparedness dispersed. Canada’s widely respected Global Public Health Intelligence Network (GPHN), created in the 1990s, was critical in warning national and international health agencies about SARS, H1N1 Influenza and Ebola. In 2018 Public Health Agency officials, assuming the potential of future pandemics was minimal, relocated its resources to other areas.16
At another scale, After SARS California Governor Arnold Schwarzenegger funded a supply depot storing materials to be used in the event of another pandemic. His successor, Governor Brown, decided it was an unnecessary expense and closed the facility.17 When Covid-19 began one of the first problems was the lack of precisely those materials that had been stockpiled by the former governor.
We knew there would be future pandemics. We know it today. COVID-19 will not be a one-off, unique experience. The World Health Organization speaks today of “Disease-X,”18 a microbe that will cause a future global pandemic with greater transmissibility and a higher mortality than today’s virus which is, really, only the latest in a long line of microbial attacks.
Discussion
It is worth speculating on the reasons we refuse to learn from the past. First, we like to think of history as a story ended, ideally with a victory achieved. To see each incidence as one in a continuing chain of continuing events argues for programs of preparation and social change that will be long-term and, in the short run, expensive. Nineteenth century physicians argued that infectious and endemic diseases were a threat both to democracy and the economics of industrializing nations. It was clear to them that disadvantaged citizens created population pools where diseases might become entrenched in a manner that would endanger other, wealthier peoples. Manchester physician John Ferriari, for example, warned that “the dwellings and persons [of the poor] continually breathe contagion. Attention to their care and needs thus served everyone, rich and poor alike. … The safety of the rich is intimately connected with the welfare of the poor … minute and constant attention to their wants is not less an act of self-preservation than of virtue.” 19
A wealth of data exists today similarly arguing the need for increased social support for marginalized citizens. Sir Douglas Black’s famous 1980 report on Inequalities in Health described a broad, inverse relationship between socioeconomic status, on the one hand, and increased disease incidence on the other.20 It was immediately rejected as too costly by neoliberal officials focused primarily on the needs of entrepreneurs and industry.21 The Black Report’s conclusions and recommendations came "disconcertingly close to a recapitulation of the recommendations [Rudolph] Virchow made 130 years ago."22 Infectious or non-infectious, the issues are the same.
From Chadwick and Virchow to Donald Trump the question has not changed. Is “a little bit of cholera” better than the dislocation of commercial advance? Is the responsibility of government first and foremost the health and welfare of populations or measures of economic growth and corporate income? The difference today is a new focus on “global health” and the recognition that issues of disease propagation and growth occur within a context of international as well as national and regional disparities.
What we know to a certainty is that this pandemic will not be our last. A new strain of influenza, or Tuberculosis, or another microbe will challenge us again in the future. We may ignore past lessons bitterly learned or build upon them to assure greater preparedness. Even better would be the broad embrace of programs to address the environmental and socioeconomic context in which infectious diseases evolve. That would be grand but is unlikely, I suspect. For most today, history is a set of lessons to be remembered only when it is too late.
Article Details
The Medical Research Archives grants authors the right to publish and reproduce the unrevised contribution in whole or in part at any time and in any form for any scholarly non-commercial purpose with the condition that all publications of the contribution include a full citation to the journal as published by the Medical Research Archives.
References
. Sacks O. Awakenings. London, Gerald Duckworth & Co.1973; revised version, NY: Picador, 1982.
. Florio J.L., Shapiro O. https:// www.nytimes.com/2020.12.20/worldNew-York-City-vaccinated-six-million-people –in-less-than-a-month-in-1947.html.
Sepkowitz K.A. The 1947 Smallpox Vaccination Campaign in New York City, Revisited. Emerging Infectious Diseases. 2004;10(5):960-961. doi:10.3201/eid1005.030973.
. Oshinsky D. M. Polio: Am American Story. NY: Oxford University Press, 2005.
. Trevelyan B. Smallman-Raynor S., Cliff, A.D. The spatial dynamics of Poliomyelitis in the United States: From Epidemic Emergency to Vaccine-Induced Retreat, 1010-1971. Annals of the Association of American Geographers 2005; 95 (2): 269-293.
. Wackers G. L. Constructivist Medicine. Maastricht, NL. Univeritare Pers Maastricht, 1994: 137-138.
. Oshinsky D. M. Op. Cit. Note 3: 69-72.
. Defoe, D. A Journal of the Plague Year & c. 1665. Norwalk, CT. The Heritage Press, 1968.
. Lepore J. Don’t come any closer. The New Yorker 2020 (March 30), 22-25.
. Lancet. History of the rise, progress, ravages, etc. of the blue cholera of India. Lancet 1831; 17 (429): 241-284.
. Hamlin C. Pubic Health and Social Justice in the Age of Chadwick. Britain, 1800-1854. NY: Cambridge University Press, 1998.
. Rosenkrantz L. Mapping Covid-19: Panel on Geography in the Time of Covid. University of British Columbia, Dept. of Geography, Vancouver, BC, Canada. Oct. 27.
. Rosenkrantz L. Mapping Covid-19: What GIS Brings to the Table. Panel on Geography in the Time of COVID. University of British Columbia, Dept. of Geography, Vancouver, BC. 2020 (Oct. 27).
. Oppel R.A., Gebeloff, R. Lai, K.K; Wright W., Smith M. The Fullest Look Yet at the
Racial Inequity of Coronavirus. New York Times 2020 (July 20). The Fullest Look Yet at the Racial Inequity of Coronavirus - The New York Times (nytimes.com). https??www.nytimes.com/interactive/2020/07/05/us/coronavirus-latinos-african-americans-cdc-data.html?
. Robertson G. Ottawa must address mistakes regarding COVID-19 pandemic preparedness, experts say. The Globe and Mail 2021 (Feb. 23).
https://www.theglobeandmail.com/canada/article-ottawa-must-address-mistakes-regarding-pandemic-preparedness-experts/.
. William L., Evans W., Carless, W. California once had mobile hospitals and a ventilator stockpile. But it dismantled them. Los Angeles Times 2020 (March 27). https://www.latimes.com/california/story/2020-03-27/coronavirus-california-mobile-hospitals-ventilators.
. Kessler R. Disease X: The Next Pandemic. EcoHealth Alliance 2018 (March). https://www.ecohealthalliance.org/2018/03/disease-x
. Hamlin, Op cit. Note 12.
. Black D, Chair. Report of the Working Group on Inequalities in Health. London: Stationary Office, 1980. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/265503/ih.pdf .
. Jenkin, C.P. Forward. Report of the Working Group on Inequalities in Health. London: Stationary office, 1980. https://www.sochealth.co.uk/national-health-service/public-health-and-wellbeing/poverty-and-inequality/the-black-report-1980/black-report-foreword/.
. Taylor R., Rieger A. Rudolf Virchow on the typhus epidemic in Upper Silesia: an introduction and translation. Sociology of Health and Illness 1984; 6 (2): 202-217.