Fatigue, Susceptibility to the Common Cold and its Behavioural Effects
Main Article Content
Abstract
The aim of the present article is to describe bi-directional interactions between fatigue and infection with common cold producing viruses. Over one hundred years ago, researchers started to investigate the association between been fatigue and infection. Studies of psychological risk factors for upper respiratory tract illnesses (URTIs) have been carried out for over fifty years. Early research did not control for exposure and also often relied on self-report rather than clinical and virological assessment. Research on experimentally-induced URTIs has demonstrated that susceptibility to infection is increased by stress. Other research has shown that job insecurity, few social contacts, emotional disposition, early childhood experiences, sleep problems and self-rated health are key risk factors for infection. This article provides an interpretation of these results in terms of chronic fatigue increasing susceptibility to infection. Infection and illness also lead to changes in behaviour. These effects include greater fatigue, impaired attention and slower motor speed. Such effects occur not only when the person has symptoms but in the incubation period, with sub-clinical infections, and after the symptoms have gone. Those with URTIs are also more sensitive to other negative factors such as prolonged work, and this has implications for safety-critical jobs. Ingestion of caffeine, which is an established countermeasure for fatigue, can reduce the behavioural malaise induced by URTIs. Further support for the use of a fatigue framework comes from a secondary analysis of data on real-life colds. Previous research has demonstrated that chronic fatigue leads to greater effects of acute fatigue. The new analysis showed that those with high levels of fatigue prior to developing a cold had larger behavioural impairments when they became ill.

Introduction
This article aims to provide a common conceptual framework for psychological risk factors for susceptibility to the common cold and the behavioural malaise that accompanies the illness. The key concept is chronic fatigue, and the link between this and infection has a long history. Anecdotal reports of the link between fatigue and infection are described in an Editorial in JAMA in 1910 1. Observations during epidemics of plague and cholera suggested that physical or mental exhaustion made the person more susceptible to disease. Vets also observed that overexertion led to a greater risk of anthrax in horses and cattle. Clinical observations in the latter part of the nineteenth century linked fatigue with many diseases of microbic origin (e.g. typhus, tuberculosis and influenza). In 1890 Charrin & Roger 2 published their classic animal studies on anthrax infection and physical exhaustion, demonstrating that fatigued rats were more susceptible to infection and more severe illnesses. These results were confirmed by De Sandro 3 (1910) using other infecting agents and other species of animals. This research also identified some immunological mechanisms underlying the effects of fatigue. First, the leukopenia (decrease in the number of leukocytes) following virus challenge was greater in the fatigued animals. Second, the subsequent polynucleosis (e.g. increase in neutrophils) was less intense and persistent in the fatigued animals. The mononucleosis (increase in lymphocytes and monocytes) that followed was also less intense in the fatigued animals. Control animals also exceeded the fatigued animals in terms of the amount of agglutinin (antibodies that cause aggregation of antigens) produced.
Psychological risk factors for susceptibility to upper respiratory tract illnesses
Psychologists have carried out research on psychological risk factors for susceptibility to URTIs for over fifty years. Early research, reviewed by Cohen and Williamson (1991)4, was criticised for the use of retrospective or cross-sectional designs, lack of control of exposure to the virus, no clinical observations or virological assays, and poor conceptualisation of psychological constructs used. These issues have subsequently been addressed using experimentally induced URTIs, prospective longitudinal designs, control of a range of possible confounders, and more clearly defined psychological models.
Experimentally induced URTIs: The MRC Common Cold Unit, UK.
Research on experimentally induced URTIs was started at the MRC Common Cold Unit, UK.
Volunteers came to the MRC Common Cold Unit, Salisbury, from all parts of the UK and stayed for ten days. Initially, they were given a medical examination, and blood samples were taken to assess pre-existing antibody levels. They were then placed in quarantine for two days to ensure they had not brought an illness with them. They were then given either a virus or saline placebo in droplets up the nose. Each day they were assessed by the unit clinician, and nasal swabs were taken to allow identification of virus shedding.
About one-third of the volunteers developed clinical colds, another third had subclinical infections, and the rest were uninfected (their immune system had quickly dealt with the virus). Blood samples were taken three weeks later and returned to the unit to assess changes in antibodies. Baseline psychological measures were taken during the quarantine period and then again when some of the volunteers were symptomatic.
The first large scale study5 found that those with high-stress scores were at greater risk of developing colds than those with lower levels of stress. These results were due to increased susceptibility to infection rather than a greater risk of becoming symptomatic. The effects of stress did not reflect health-related behaviours, although subsequent analyses6 found that smoking increased both infection and illness, and consumption of a small amount of alcohol on a regular basis reduced the symptom severity, possibly due to the anti-inflammatory action reducing nasal symptoms. Different types of stress influenced either infection or illness. Negative affect and perceived stress increased the likelihood of infection, whereas negative life events led to greater symptom severity7.
Closure of the MRC Common Cold Unit
Results from studies of psychosocial factors and experimentally induced URTI have been replicated in research on naturally occurring illnesses8 and confirmed with other infectious agents9. However, the unit closed in 1990, and the experimental induction of colds was then largely carried out in the USA. A series of trials, the Pittsburgh studies (see Cohen, 2005, for a review10), continued to examine psychosocial factors and susceptibility to URTIs.
Experimentally induced URTIs: The Pittsburgh Studies
Initial research11 showed that chronic stress was the key risk factor for susceptibility to URTIs. Major risk factors were lack of social support and job insecurity. These effects did not reflect personality or health-related behaviours, although these latter factors had independent effects on the disease outcomes. Other research12 demonstrated that having fewer social ties was also a risk factor for susceptibility to infection, and more diverse social networks were associated with greater resistance to upper respiratory illness. A positive emotional style also predicted resistance to URTIs13, and dispositional affect moderated the buffering effect of social support on the risk of developing a cold14. Other research investigated the importance of socioeconomic status15 and parental separation during childhood16. As in other areas of public health, low income and parental separation were risk factors for URTIs. Other research focused on sleep17 and showed that shorter sleep duration led to greater susceptibility to the common cold. Later research suggested that this effect of sleep duration was only observed in those with low socioeconomic status18. Poor self-rated health (SRH) status was also a risk factor for susceptibility to URTIs19, which probably reflects the association between SRH and premorbid immune dysfunction.
The Pittsburgh studies also aimed to identify the immunological mechanisms linking psychosocial factors to infection. One line of research showed that shorter CD8CD28- T-cell telomere length was a risk factor for experimentally induced acute upper respiratory infection and illness20. Other research21,22 supported the view that interleukin-6 (IL-6) might be the link between psychological factors and the risk of infection. Another study examined the role of neuroendocrine factors and demonstrated an association between basal cortisol production and the risk of URTI infection23. This provided support for the chronic stress, glucocorticoid receptor resistance, inflammation, and disease risk model24. This view argues that chronic stress interferes with responding to hormones that turn off the pro-inflammatory cytokines. This increases the response of the immune system, which then over-responds and amplifies the symptoms of the URTI. Chronic stressors increase the glucocorticoid response (GCR), which reduces the sensitivity of the immune system to glucocorticoid hormones that normally suppress the inflammatory response. It has been shown that stress increases GCR, which is a risk factor for getting a cold and leads to the production of more pro-inflammatory cytokines (TNF-alpha, IL-beta and IL-6).
A re-interpretation of psychological factors and the common cold: The role of fatigue
This next section examines whether some of the diverse results linking psychosocial factors to susceptibility to experimentally induced URTIs can be put in a fatigue framework. It is not intended to dispute early findings but rather to re-interpret in a parsimonious way. Most psychosocial concepts have many correlated attributes, and the next section examines whether chronic fatigue scores are correlated with some of the risk factors for URTIs.
Smith25 conducted a large scale prospective study of naturally-occurring URTIs. At baseline, participants (N=457) completed a battery of psychosocial questionnaire, one being the Profile of Fatigue Related Symptoms26, and others which had been shown to be predictors of susceptibility to experimentally-induced URTIS. Fatigue showed the following correlations, all of which were significant:
- Negative Life Events: r = 0.21
- Perceived Stress Scale: r = 0.46
- Social Support (ISEL total score): r = -0.21
- UCLA Loneliness score: r = 0.29
- Alert mood: r = -0.26
- Hedonic Tone: r = -0.19
- Anxiety: r = -0.13
Not too surprisingly, a literature search also confirms that short sleep time and poor self-rated health are also positively associated with fatigue. Interestingly, fatigue is also correlated with childhood stress27. Mechanisms linking psychosocial factors and susceptibility to URTIs are also related to fatigue (e.g. high cortisol and fatigue28; Il-6 and fatigue29; and telomere length and fatigue30). The next question is whether chronic fatigue is associated with increased susceptibility to URTIs.
Chronic fatigue and susceptibility to URTIs
Two studies of susceptibility to naturally occurring illnesses support the view that chronic fatigue is associated with increased susceptibility to URTIs. Smith et al.31 conducted a prospective diary study of susceptibility to colds and influenza. The participants were patients who had been diagnosed with Chronic Fatigue Syndrome (CFS) and healthy controls. The CFS group reported more illnesses and greater severity of symptoms. Smith and Thomas32 repeated the study and included virological assays to identify the infecting agents. The results confirmed that CFS patients reported more URTIs, and the increased infection rates showed that this was not due to a bias in symptom reporting but reflected greater susceptibility to infection.
The above sections suggest that it is reasonable to interpret previous results linking psychosocial factors to susceptibility to URTIs in terms of chronic fatigue. Another area of research, this time studying the effects of URTIs on the brain and behaviour, also supports this approach and is briefly reviewed in the next section.
Effects of URTIs on Behaviour
Research on stress, fatigue and infection is an area of research on how the brain and behaviour influence the immune system. The relationship between the brain and the immune system is bi-directional, and the next section is concerned with the effect of URTIs on cognition and mood. Again, much of this has involved initial studies of experimentally induced colds and influenza, with the results being confirmed in later research with naturally occurring URTIs. A detailed review of the results from both types of study is given in Smith33.
Experimentally-induced URTIs
The early studies demonstrated that URTIs were associated with performance impairments and an increase in negative mood34-40 (reviewed by Smith41-45). Colds and influenza were associated with different profiles of impairment, with colds leading to psychomotor slowing and influenza impairing the performance of attention tasks (where the person did not know where the stimulus would be presented or when to respond). The differences between colds and influenza may also reflect the severity of the illnesses and/or the sample sizes in the different studies. Impairments were observed when the person was symptomatic in the incubation period of the illness, with sub-clinical infections, and after the symptoms were no longer present.
Naturally-occurring URTIs:
The initial aim of studies of naturally occurring URTIs was to replicate effects observed with experimentally induced URTIs. This was achieved46,47, and some of the studies even used virological techniques to identify the infecting agent48.49. Other studies examined possible cognitive mechanisms for the impairments50-58. The early studies used computer-based cognitive tasks but later research used simulations of real-life activities, such as driving59-60, and the results suggested that driving performance may be impaired when the person has a cold.
The combined effects of having a cold and performing in noise61, after alcohol62, and after a day of work63-64 showed that having a cold led to a greater impact of risk factors for fatigue. Caffeine is a known countermeasure for fatigue, and the impairments seen when the person has a cold could be reduced by ingestion of caffeine65-66. This led to research investigating the neurotransmitter basis of the cold-induced impairments. Research with naturally occurring colds found that the impairments were reduced by a drug which increased the uptake of central noradrenaline67. Other researchers68 suggested that the impairments related to having a cold were due to sleep disturbance, but there has been little evidence supporting this view69-70.
Research has also examined the immunological basis for the behavioural effects of URTIs. Research at the MRC Common Cold Unit showed that behavioural effects similar to those when a person has influenza were observed when volunteers were given an injection of alpha interferon71-72. Other research suggests that Il-6 may be associated with the mood changes associated with URTIs73 and possibly the psychomotor slowing74.
The above section suggests that the effects of URTIs on performance and mood should be examined in a fatigue framework. One more piece of evidence would strengthen this view, and this requires data on the effects of URTIs in those with high and low chronic fatigue.
Acute fatigue in those with chronic fatigue
Research demonstrates that those with chronic fatigue are more sensitive to acute fatigue75. In that study, chronic fatigue was defined by the person having been diagnosed with chronic fatigue syndrome. Acute fatigue was assessed by examining changes with time on task. The new analyses presented in the next section used a sample of university students and sub-divided them into high and low fatigue groups based on PFRS fatigue scores collected at baseline and reflecting the month before that time point. High acute fatigue was defined by having a cold (low acute fatigue was being healthy). The outcome measures were subjective alertness and simple reaction time. Details of the methodology are given in Smith57 and can be summarised as follows.
A prospective study was carried out, and 200 university students recruited in early autumn and carried out ratings of alertness, a measure of psychomotor speed and completed the profile of fatigue-related states questionnaire. Participants returned to the laboratory when they developed a cold and repeated the procedure. Those who did not catch a cold in 10 weeks were re-test as healthy controls. One hundred and eighty-seven completed the study (91 male, 96 female; mean age 20.9 years, range 18-30 years). Forty-eight developed colds, and the rest were healthy controls. The sample was subdivided into those with high/low fatigue scores (based on a median split) at baseline. A MANOVA was carried out using percentage change from baseline as the dependent variable and cold and fatigue groups as the independent variable. The results are shown in Table 1. There was a highly significant effect of cold status (Wilks’ Lambda = 0.586 p < 0.001 partial eta =0.414) and a significant interaction between cold status and baseline fatigue (Wilks Lambda = 0.927 p < 0.005 partial eta squared = 0.073). Those with colds reported lower alertness and had a slower psychomotor response. Those with a cold and high baseline fatigue showed the greatest impairments.
Table 1: The effects of having a cold and fatigue status on the percentage change from baseline for the reaction times and alertness ratings.
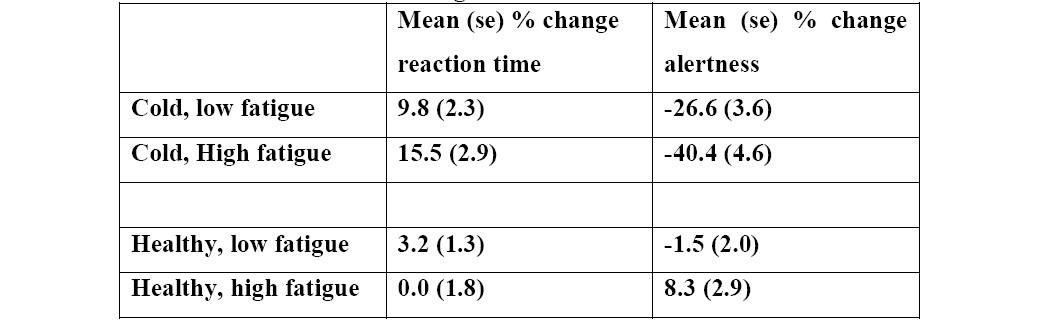
Higher RT scores = greater slowing
Lower alertness = greater drop in alertness
Conclusion
Fatigue provides a good conceptual framework for research on susceptibility to URTIs and their effects on behaviour. This does not imply that research using other approaches is wrong, but rather the current view presents the “big picture”, which may make the area more understandable by non-experts, whereas the more focused approaches, which consider specific psychosocial concepts, provide information on the microstructure of associations. Further research, either with experimentally induced URTIs or large scale epidemiological methods, is now required to test the view presented here. In addition, there should be more attention to the health implications of chronic fatigue.
It should also be pointed out that these illnesses have a major impact on healthcare costs and cause frequent absenteeism from education and work. It has been shown 76 that in the USA the annual cost of lost productivity because of the common cold is over $25 billion, of which $16.6 billion is due to productivity loss, $8 billion to absenteeism, and $230 million to caregiver absenteeism. Other research77-79 has shown that URTIs lead to presenteeism, with academic and work performance being less efficient than normal.
Article Details
The Medical Research Archives grants authors the right to publish and reproduce the unrevised contribution in whole or in part at any time and in any form for any scholarly non-commercial purpose with the condition that all publications of the contribution include a full citation to the journal as published by the Medical Research Archives.
References
2. Charrin Le G, Roger, CW (1890) Contribution à l'étude expérimentale du surmenage. Son influence, surl'infection. Arch. de Physol. 1890. (cited in Editorial JAMA. Fatigue and susceptibility to infection, 1911).
3. De Sandro D Riforma Med. 1910. 841-871. (cited in Editorial JAMA. Fatigue and susceptibility to infection, 1911).
4. Cohen S, Williamson, GM. Stress and infectious disease in humans. Psychological Bulletin.1991; 109(1): 5–24.
5. https://doi.org/10.1037/0033-2909.109.1.5
6. Cohen S, Tyrrell DA.J, Smith AP. Psychological stress in humans and susceptibility to the common cold. New England Journal of Medicine. 1991; 325: 606 - 612. www.nejm.org/doi/full/10.1056/NEJM199108293250903
7. Cohen S,Tyrrell DAJ, Russell M, Jarvis MJ, Smith AP. Smoking, alcohol consumption and susceptibility to the common cold. American Journal of Public Health, 1993; 83: 1277-1283. https://dx.doi.org/10.2105%2Fajph.83.9.1277
8. Cohen S. Tyrrell DAJ, Smith AP. Negative Life Events, Perceived Stress, Negative Affect and Susceptibility to the Common Cold. Journal of Personality and Social Psychology. 1993; 64: 131 -140. doi: 10.1037//0022-3514.64.1.131
9. Smith AP, Nicholson KG. Psychosocial factors, respiratory viruses and exacerbation of 2020, asthma. Psychoneuroendocrinology. 2001; 26: 411-420. https://doi.org/10.1016/S0306-4530(00)00063-9
10. Song H, Fall K, Fang F, et al. Stress related disorders and subsequent risk of life threatening infections: population based sibling controlled cohort study. British Medical Journal. 2019; 367: 15784. doi:10.1136/bmj.l5784
11. Cohen S. The Pittsburgh Common Cold Studies: Psychosocial predictors of susceptibility to respiratory infectious illness. International Journal of Behavioral Medicine. 2005; 12: 123-154. doi: 10.1207/s15327558ijbm1203_1
12. Cohen S, Frank E, Doyle WJ, Skoner DP, Rabin BS, Gwaltney JM, Jr. Types of stressors that increase susceptibility to the common cold in healthy adults. Health Psychology. 1998; 17: 214-223.
13. Cohen S, Doyle WJ, Skoner DP, Rabin BS, Gwaltney J.M,Jr. Social ties and susceptibility to the common cold. Journal of the American Medical Association. 1997; 277: 1940-1944.
14. Cohen S, Alper CM, Doyle WJ, Treanor JJ, Turner RB. Positive emotional style predicts resistance to illness after experimental exposure to rhinovirus or influenza A virus. Psychosomatic Medicine. 2006; 68: 809-815.
15. Janicki-Deverts D, Cohen S, Doyle WJ. Dispositional affect moderates the stress-buffering effect of social support on risk for developing the common cold. Journal of Personality. 2017; 85: 675-686.
16. Cohen S, Doyle WJ, Turner RB, Alper CM, Skoner DP. Childhood socioeconomic status and host resistance to infectious illness in adulthood. Psychosomatic Medicine. 2004; 66: 553-558.
17. Murphy MLM, Cohen S, Janicki-Deverts D, Doyle WJ. Offspring of parents who were separated and not speaking to one another have reduced resistance to the common cold as adults. Proceedings of the National Academy of Sciences. 2017; 114: 6515-6520.
18. Prather AA, Janicki-Deverts D, Adler NE, Hall M, Cohen S. Sleep habits and susceptibility to upper respiratory illness: the moderating role of subjective socioeconomic status. Annals of Behavioral Medicine. 2017; 51: 137-146.
19. Prather AA, Janicki-Deverts D, Hall MH, Cohen S. Behaviorally assessed sleep and susceptibility to the common cold. Sleep. 2015; 38(9):1353-1359. PMCID: PMC4531403
20. Cohen S, Janicki-Deverts D, Doyle WJ. Self-rated health in healthy adults and susceptibility to the common cold. Psychosomatic Medicine. 2015; 77 (9): 959-968.
21. Cohen S, Janicki-Deverts D, Turner RB, Casselbrant ML, Li-Korotky H, Epel E S, Doyle W J. Association between telomere length and experimentally induced upper respiratory viral infection in healthy adults. Journal of the American Medical Association. 2013; 309: 699-705. doi: 10.1001/jama.2013.613
22. Doyle WJ, Gentile DA, Cohen S. Emotional style, nasal cytokines, and illness expression after experimental rhinovirus exposure. Brain, Behavior, and Immunity. 2007; 20:175-181.
23. Doyle WJ, Casselbrant ML, Li-Korotky H, Cullen Doyle AP, Lo C, Turner R, Cohen S. The interleukin 6 -174 C/C genotype predicts greater rhinovirus illness. The Journal of Infectious Diseases. 2010; 201: 199-206.
24. Janicki-Deverts D, Cohen S, Turner RB, Doyle WJ. Basal salivary cortisol secretion and susceptibility to upper respiratory infection. Brain, Behavior, & Immunity. 2016; 53: 255-261.
25. Cohen S, Janicki-Deverts D, Doyle WJ, Miller GE, Frank E, Rabin BS, Turner RB. Chronic stress, glucocorticoid receptor resistance, inflammation, and disease risk. Proceedings of the National Academy of Sciences. 2012; 109: 5995-5999.
26. Smith AP. Effects of upper respiratory tract illness and stress on alertness and reaction time. Psychoneuroendocrinology. 2013; 38: 2003-2009. http://dx.doi.org/10.1016/j.psyneuen.2013.03.012
27. Ray C, Weir WRC, Phillips S, Cullen S. Development of a measure of symptoms in Chronic Fatigue Syndrome: The Profile of Fatigue-Related Symptoms (PFRS). Psychology and Health. 1992; 7(1): 27-43. doi: 10.1080/08870449208404293
28. Borsini A, Hepgul N, Mondelli V, Chalder T, Pariante C. Childhood stressors in the development of fatigue syndromes: a review of the past 20 years of research. Psychological Medicine. 2014; 44 (9): 1809-1823.
29. Fujimaru C, Okamura H, Kawasaki M, Tatsuyuki Y, Matsuishi T. Self-perceived work-related stress and its relation to salivary IgA, cortisol and 3-methoxy-5-hydroxyphenyl glycol levels among neonatal care nurses. Stress and Health. 2012; 28: 171-174.
30. Rohleder N, Aringer M, Boentert M. Role of interleukin-6 in stress, sleep and fatigue. Annals of the New York Academy of Sciences. 2012; 1261: 88-96.
31. Bendix L, Thingaard M, Kimura M, Aviv A, Christensen K, Osler M, Avlund K. Association of leukocyte telomere length with fatigue in nondisabled older adults. Journal of Aging Research. 2014; Article ID: 403253, 8 pages.
32. Smith AP, Thomas M, Borysiewicz L, Llewelyn,M. Chronic fatigue syndrome and susceptibility to upper respiratory tract illnesses. British Journal of Health Psychology. 1999; 4: 327-335.
33. Smith AP, Thomas MA. Chronic fatigue syndrome and increased susceptibility to upper respiratory tract infections and illnesses. Fatigue: Biomedicine, Health & Behavior. 2015; 3(3): 156-163. http://dx.doi.org/10.1080/21641846.2015.1033271
34. Smith AP. Twenty-five years of research on the behavioural malaise associated with influenza and the common cold. Psychoneuroendocrinology. 2013; 38: 744-751. https://doi.org/10.1016/j.psyneuen.2012.09.002
35. Smith AP, Tyrrell DAJ, Coyle K, Willman JS. Selective effects of minor illnesses on human performance. Brit J Psychol. 1987; 78: 183 - 188. doi:10.1111/j.2044-8295.1987.tb02238.x
36. Smith AP, Tyrrell DAJ, Al-Nakib W, Coyle KB, Donovan CB, Higgins PG, Willman JS. Effects of experimentally-induced virus infections and illnesses on psychomotor performance. Neuropsychobiology. 1987; 18: 144 - 148. doi: 10.1159/000118408
37. Smith AP, Tyrrell DAJ, Al-Nakib W, Coyle KB, Donovan CB, Higgins PG, Willman J S. The effects of experimentally-induced respiratory virus infections on performance. Psychol Med. 1988; 18: 65 - 71. doi: 10.1017/s0033291700001896
38. Smith AP, Tyrrell DAJ, Al-Nakib W, Barrow GI, Higgins PG, Leekam S, Trickett S. Effects and after-effects of the common cold and influenza on human performance. Neuropsychobiology. 1989; 21: 90 - 93. doi: 10.1159/000118558
39. Smith AP, Tyrrell DAJ, Barrow GI, Coyle KB, Higgins PG, Trickett S, Willman JS. The effects of experimentally induced colds on aspects of memory. Percept Mot Skills. 1990; 71: 1207 - 1215. doi: 10.2466/pms.1990.71.3f.1207
40. Smith AP, Tyrrell DAJ, Barrow GI, Higgins PG, Willman JS, Bull S, Coyle KB, Trickett S. Mood and experimentally-induced respiratory virus infections and illnesses. Psychol Health. 1992; 6: 205-212. doi: 10.1080/08870449208403184
41. Smith AP, Tyrrell DAJ, Barrow GI, Higgins PG, Bull S, Trickett S, Wilkins AJ. The Common Cold, pattern sensitivity and contrast sensitivity. Psychol Med. 1992; 22: 487-494 doi: 10.1017/S0033291700030427
42. Smith AP. Minor illnesses and performance. In: Different Aspects of Performance. (eds) W Rohmert & H G Wenzel Frankfurt: Peter Lang. 2009; 300 – 306.
43. Smith AP. A review of the effects of colds and influenza on human performance. Journal of the Society of Occupational Medicine. 1989; 39: 65-68. https://doi-org.abc.cardiff.ac.uk/10.1093/occmed/39.2.65
44. Smith AP. Respiratory virus infections and performance. In: Human Factors in Hazardous Situations, (eds) D Broadbent, A D Baddeley and J Reason. Oxford Science Publications. 1990.
45. Smith AP. Respiratory illnesses and performance. In: Contemporary Ergonomics. 1991; (ed) E J Lovesey. London: Taylor & Francis, 203 – 207.
46. Smith AP. Colds, influenza and performance. In: Handbook of Human Performance, Vol2: Health and Performance. (eds) A P Smith & D M Jones London: Academic Press. 1992; pp 197-218.
47. Hall SR, Smith AP. An investigation of the effects and after-effects of naturally occurring upper respiratory tract illnesses on mood and performance. Physiology and Behavior. 1996; 59: 569-577. https://doi.org/10.1016/0031-9384(95)02112-4
48. Smith AP. Psychological studies of the common cold. In: The Common Cold - The condition and its treatment. 1996; pp 89-111. Ed DAJ Tyrrell. Stuttgart: Gustav Fischer (In German).
49. Smith AP, Thomas M, Brockman P, Kent J, Nicholson KG. Effect of influenza B virus infection on human performance. British Medical Journal. 1993; 306: 760 – 761. doi: 10.1136/bmj.306.6880.760
50. Smith A, Thomas M, Kent J, Nicholson K. Effects of the common cold on mood and performance. Psychoneuroendocrinology. 1998; 23: 733-739. http://dx.doi.org/10.1016/S0306-4530(98)00042-0
51. Smith A, Rich N, Sturgess W, Brice C, Collison C, Bailey J, Wilson S, Nutt D. Effects of the common cold on subjective alertness, simple and choice reaction time and eye movements. Journal of Psychophysiology. 1999; 13: 145-151. doi: 10.1027//0269-8803.13.3.145
52. Smith AP, Thomas M, Whitney H. After-effects of the common cold on mood and performance. Ergonomics. 2000; 43: 1342-1349. http://dx.doi.org/10.1080/001401300421789
53. Matthews G, Warm JS, Dember WN, Mizoguchi H, Smith AP. The common cold impairs visual attention, psychomotor performance and task engagement. Proceedings of the Human Factors and Ergonomics Society 45th Annual Meeting. Santa Monica, CA : Human Factors and Ergonomics Society. 2001; pp 1377-1381.
54. Smith AP. From the brain to the workplace: research on cognitive fatigue in the laboratory and on board ship In: Cognitive Fatigue: Multidisciplinary perspectives on current research and future applications. Ed P Ackerman. American Psychological Association. 2011; Chapter 14: pp 291-305. ISBN: 978-1-4338-0839-5
55. Smith AP. Behavioral effects of upper respiratory illnesses: A consideration of possible underlying cognitive mechanisms. Behavioral Sciences. 2012; 2: 38-49. doi:103390/b2010038
56. Smith AP. Effects of the common cold on mood, psychomotor performance, the encoding of new information, speed of working memory and semantic processing. Brain, Behavior & Immunity. 2012; 26:1072-1076. http://dxdoiorg/101016/jbbi201206012
57. Smith AP. Upper respiratory tract illnesses and fatigue. In: Matthews, G, Desmond, PA, Neubauer, C, & Hancock, PA (Eds), The Handbook of Operator Fatigue. Farnham, Surrey, UK: Ashgate Publishing. ISBN: 978-0-7546-7537-2. 2012; Chapter 20: Pg 321-332.
58. Smith AP. Effects of upper respiratory tract illness and stress on alertness and reaction time. Psychoneuroendocrinology.2013;38:2003-2009. http://dxdoiorg/101016/jpsyneuen201303012
59. Matthews G, Warm JS, Smith AP. Task engagement and attentional resources: Multivariate models for individual differences and stress factors in vigilance. Human Factors. 2017; 59: (1), 44-61. doi: 101177/0018720816673782
60. Smith AP. Effects of the Common Cold on simulated driving. In Contemporary Ergonomics 2006. Editor: PD Bust. pp621-624. ISBN10 0415398185
61. Smith AP, Jamson SL. An investigation of the effects of the common cold on simulated driving performance and detection of collisions: a laboratory study. BMJ Open. 2012; 2:e001047. doi:101136/bmjopen-2012-001047
62. Smith AP, Thomas M, Brockman P. Noise, respiratory virus infections and performance. Proceedings of 6th International Congress on Noise as a Public Health Problem. Actes Inrets. 1993; 34: Vol 2, 311-31
63. Smith AP, Whitney H, Thomas M, Brockman P, Perry K. A comparison of the acute effects of a low dose of alcohol on mood and performance of healthy volunteers and subjects with upper respiratory tract illnesses. Journal of Psychopharmacology. 1995; 9: 225-230. https://doi.org/10.1177/026988119500900310
64. Smith AP, Thomas M, Whitney H. Effects of upper respiratory tract illnesses on mood and performance over the working day. Ergonomics. 2000; 43: 752-763. http://dx.doi.org/10.1080/001401300404724
65. Smith AP, Brice C, Leach A, Tiley M, Williamson S. Effects of upper respiratory tract illnesses in a working population. Ergonomics. 2004; 47: 363-369.
66. Smith AP, Thomas M, Perry K, Whitney H. Caffeine and the common cold. Journal of Psychopharmacology. 1997; 11 (4): 319-324. https://doi.org/10.1177/026988119701100406
67. Smith AP, Nutt DJ. Effects of upper respiratory tract illnesses, ibuprofen and caffeine on reaction time and alertness Psychopharmacology. 2014; 231: 1963-1974. doi: 101007/s00213-013-3339-7
68. Smith AP, Sturgess W, Rich N, Brice C, Collison C, Bailey J, Wilson S, Nutt DJ. Effects of idazoxan on reaction times, eye movements and mood of healthy volunteers and subjects with upper respiratory tract illnesses. Journal of Psychopharmacology. 1999; 13: 148-151. doi: 10.1007/s00213-013-3339-7
69. Drake CL, Roehrs TA, Royer H, Koshorek G, Turner RB, Roth T. 2000. Effects of an experimentally induced rhinovirus cold on sleep, performance and daytime alertness. Physiol Behav. 2000; 71: 75-81. doi: 101016/S0031-9384(00)0322-x
70. Smith AP. Sleep, colds and performance. In: Sleep, Arousal and Performance: A tribute to Bob Wilkinson. Eds: R Broughton & R Ogilvie. Boston: Birkhauser. 1991; 233-242.
71. Smith AP. Sleep and the common cold. Journal of Behavioral Health. 2012; 1: 114-117. ISSN 2146-8346. doi:105455/jbh20120322073850
72. Smith AP, Tyrrell DAJ, Coyle KB, Higgins PG. Effects of interferon alpha on performance in man: A preliminary report. Psychopharmacology. 1988; 96: 414 – 416. https://doi.org/10.1007/BF00216072
73. Smith AP, Tyrrell DAJ, Coyle KB, Higgins PG. Effects and after-effects of interferon alpha on human performance, mood and physiological function. Journal of Psychopharmacology. 1991; 5: 243 - 250.
74. Janicki-Deverts D, Cohen S, Doyle WJ, Turner RB, Treanor JJ. Infection-induced pro-inflammatory cytokines are associated with decreases in positive affect, but not increases in negative affect. Brain, Behavior, and Immunity. 2007; 21: 301-307.
75. Balter L, Higgs S, Aldred S, Bosch J, Raymond J. Inflammation Mediates Body Weight and Ageing Effects on Psychomotor Slowing. Scientific Reports. 2019; 9(1): 15727, pp. 1-13. https://doi.org/10.1038/s41598-019-52062-3
76. Smith AP, Borysiewicz L, Pollock J, Thomas M, Perry K, Llewelyn M. Acute fatigue in chronic fatigue syndrome. Psychological Medicine. 1999; 29: 283-290.
77. Bramley TJ, Lerner D, Sarnes M. Productivity losses related to the common cold. J. Occup. Environ. Med. 2002; 44: 822-829.
78. Nichol KL, D’Heilly S, Ehlinger E. Colds and influenza-like illnesses in university students: impact on health, academic and work performance, and health care use. Clin. Infect. Dis. 2005; 40:1263-1270.
79. Nichol KL, D’Heilly S, Ehlinger E. Burden of upper respiratory illnesses among college and university students: 2002-2003 and 2003-2004 cohorts. Vaccine. 2006; 24, 6724-6725.
80. Palmer LA, Rousculp MD, Johnston SS, Mahadevia PJ, Nichol KL. Effect of influenza-like illness and other wintertime respiratory illnesses on worker productivity: the child and house- hold influenza-illness and employee function (CHIEF) study. Vaccine. 2010; 28: 5049-5056.