Catecholamine Concentrations during and after Retroperitoneoscopic Adrenalectomies in Surgeon, Anaesthetist and Patients – how is physiological stress different from pathophysiological stress? Catecholamine Concentrations during Retroperitoneoscopic Adrenalectomies
Main Article Content
Abstract
Background: During resections of phaeochromocytoma release of catecholamines can lead to excessive hypertension and arrhythmia. Therefore, these procedures can be stressful to surgeons and anaesthetists. It is completely unknown, how the excessive catecholamine concentrations in phaeochromocytoma patients relate to catecholamine concentrations of physiological stress of physicians and control patients undergoing adrenalectomy because of hormone inactive tumours. We measured catecholamine concentrations, heart rate and blood pressure in patients with phaeochromocytoma, incidentaloma, a surgeon and an anaesthetist.
Methods: After approval of the local ethics committee, we measured metanephrine and normetanephrine plasma concentrations in 8 patients with phaeochromocytoma, 6 control patients with incidentaloma, one surgeon and one anaesthetist at rest, after incision, after 20 and 40 minutes of surgery, and in recovery. Moreover, blood pressure and heart rate were obtained.
Results: Intraoperatively significant increases of blood pressure, metanephrine and normetanephrine were found in patients and surgeon. Significant increase of normetanephrine was also found in control patients. But catecholamine concentrations in patients with phaeochromocytoma were 18 to 42 times higher than in control patients and physicians. Heart rate analysis showed no significant results.
Conclusion: During phaeochromocytoma resections significant increases in catecholamine concentration and blood pressure can be found in patients and physicians. The excessive increase of catecholamine concentrations in phaeochromocytoma patients, was not always reflected by a corresponding blood pressure increase. Interestingly, although catecholamine concentrations in phaeochromocytoma patients almost normalize directly after surgery, their blood pressure remains stable without the need for pharmacological support.

Background
Physiological stress is a collective term for reactions of the organism to psychological and/or physical stress, which are controlled by the central nervous system. In general, two main stress axes are distinguished: a fast sympatico-adreno-medullary (SAM) axis and a slow hypothalamic-pituitary-adrenal (HHN) axis. 1 Stress responses via the SAM axis include all responses that result in immediate central nervous activation of the sympathetic nervous system and adrenal medulla and are accompanied by a release of catecholamines.
However, catecholamines can also be released uncontrolled, pathologically due to a phaeochromocytoma. Phaeochromocytoma and paraganglioma are rare neuroendocrine tumours originating in the chromaffin cells of the sympathetic nervous system. Due to their neuroendocrine origin, these tumors are capable of producing catecholamines (epinephrine, norepinephrine, dopamine) which largely determines their clinical but equally variable appearance.2 However, cardiovascular side effects and associated diseases are the main cause of life-threatening complications. Epinephrine, with its preferential stimulation of ß1- and ß2- adrenoceptors, causes tachycardia and arrhythmias, whereas the effects on blood pressure can be small. Norepinephrine, with its -adrenergic action, causes particularly excessive increases in blood pressure, and due to the baroreceptor reflex rather a decrease in heart rate than tachycardia. Dopamine-producing tumors are associated with normotensive as well as hypotensive blood pressure. 2,3
During resections of phaeochromocytoma, surgical manipulation can lead to bolus-like release of catecholamines with excessive hypertension, tachycardia and arrhythmia within seconds. Therefore, these surgeries were considered high-risk operations with high mortality rates (20-45%) until the second half of the 20th century. 4-5 Although mortality has been significantly reduced in the meantime from 1-3% in the last decades6-9 to 0.3 – 0.5% most recently, 10 these operations still represent a major challenge for the attending physicians, which requires a very high concentration and readiness to react, especially intraoperatively, to counteract an uncontrolled catecholamine release. Therefore, these procedures can be very stressful to surgeons and anesthetists.
Until now it is completely unclear how pathophysiological stress (in phaeochromocytoma patients) compares to a physiological stress response (in control patients, surgeon and anesthetist). Moreover, how does intraoperative stress differ between patients with catecholamine-producing tumour compared to a noncatecholamine-producing tumour of the adrenal gland (incidentaloma).
To investigate this question, we determined haemodynamic parameters (heart rate and blood pressure) and the plasma catecholamine metabolites metanephrine and normethanephrine in 8 phaeochromocytoma patients, 6 patients with an adrenal tumor without catecholamine production (incidentaloma patients), one surgeon and one anesthetist.
Patients and Methods
After approval by the local ethics committee (Board of Physicians “Ärztekammer Nordrhein” reg.no.: 2009061) 8 phaeochromocytoma and 6 incidentaloma patients scheduled for surgery between May 2009 and October 2017 gave their informed written consent to have their data analysed in this observational study. 7 patients suffered from sporadic phaeochromocytoma, one patient suffered from Hippel-Lindau disease. All tumours were histologically verified as phaeochromocytoma.
Half of all examined phaeochromocytoma patients showed a mixed secretion pattern of catecholamine (norepinephrine and epinephrine), the others showed a pure norepinephrine production. 7 phaeochromocytoma patients received preoperative antihypertensive treatment, including only two patients with preoperative -receptor blockade. The majority of incidentaloma patients (5 of 6) received antihypertensive medication. The attending anaesthesitist and surgeon for all operations were the head of the Department of Anaesthesia, Critical Care Medicine and Pain Therapy (Prof. Dr. med. H. Groeben) and the head of the Department of Surgery and Center of Minimal Invasive Surgery, Kliniken Essen-Mitte (Prof. Dr. med. Dr. h.c. M. K. Walz).
Preoperative management
Preoperative preparations were in accordance with the hospital's standard procedure. -receptor blockade was not initiated. Only in previously treated patients was -receptor blockade continued until the day of surgery.
Anaesthesia and Surgery
On the day of surgery, blood sample was taken to determine the baseline catecholamine concentration of patients’ and physicians’ via an indwelling venous cannula after 20 minutes of rest. Blood sampling of the patients was performed in the anaesthesia induction room. Blood sampling of the physicians was performed in the respective office.
For all patients invasive monitoring was applied and an arterial line was placed under local anaesthesia in the right or left radial arteria. Subsequently, general anaesthesia was induced with propofol, remifentanil, and mivacurium and endotracheal intubation was performed. In the phaeochromocytoma patients, intraoperative monitoring was extended by placing a central venous catheter into the jugular vein to apply vasoactive agents. All patients were placed in prone position. Anaesthesia was maintained with isoflurane in an oxygen/air mixture and continuous intravenous administration of remifentanil. Further blood samples were taken intraoperatively at the time of incision, after 20 and 40 minutes after incision, and postoperatively in the recovery room. In addition, heart rate and blood pressure were measured at each of these times.
Postoperative management
After the operation, the patients were transferred to the recovery room. Postoperative treatment with vasoactive substances was not necessary in any patient.
The blood samples were stored on ice immediately and separated in the in-house laboratory and frozen. Further analysis was performed using high-performance liquid chromatography.
Data Analysis
A total of 14 patients (8 phaeochromocytoma and 6 incidentaloma patients), one anaesthetist, and one surgeon were included in the study with respect to a calculation based on a power analysis. Power analysis was based on a test power of 0.8, an -error of 0.05, and a β-error of 0.1. Patient and subject characteristics (age, height, weight, blood pressure, heart rate), intraoperative infusion volume, operative time, and metanephrine and normetanephrine plasma concentrations were calculated as mean ± standard deviation. To compare the different perioperative serial measurements (metanephrine, normethanephrine, blood pressure, heart rate), a two-factorial analysis of variance with a repeated measure ANOVA (Analysis of Variance for repeated Measurements) was performed. A post-hoc test (Bonferroni) for multiple testing was performed. Significant differences were assumed with p values < 0.05
Results
Blood pressure
There was a significant increase in maximum systolic blood pressure in the phaeochromocytoma patients and the surgeon, but with a significantly greater increase in the phaeochromocytoma group (p = 0.0001). Systolic blood pressure at baseline in the phaeochromocytoma patients was 153 ± 27 mmHg. At the 20-minute time point, maximal systolic blood pressure was 176 ± 46 mmHg. No significant differences in maximum systolic blood pressure were found for the incidentaloma patients or the anaesthetist. The highest measured systolic blood pressure in the incidentaloma patients was seen preoperatively (baseline: 135 ± 6 mmHg). No significant changes in blood pressure were seen in the anaesthetist. In contrast to the physicians, patients’ systolic blood pressure decreased significantly after induction of anaesthesia. Intraoperatively, the patients' blood pressures increased in phaeochromocytoma patients and deceased in patients with an incidentaloma. Despite the different blood pressure dynamics of the study groups, all patients and physicians showed normotensive blood values in the recovery room. In particular, phaeochromocytoma patients did not experience a dramatic drop in blood pressure after resection of the catecholamine-producing tumor (figure1).
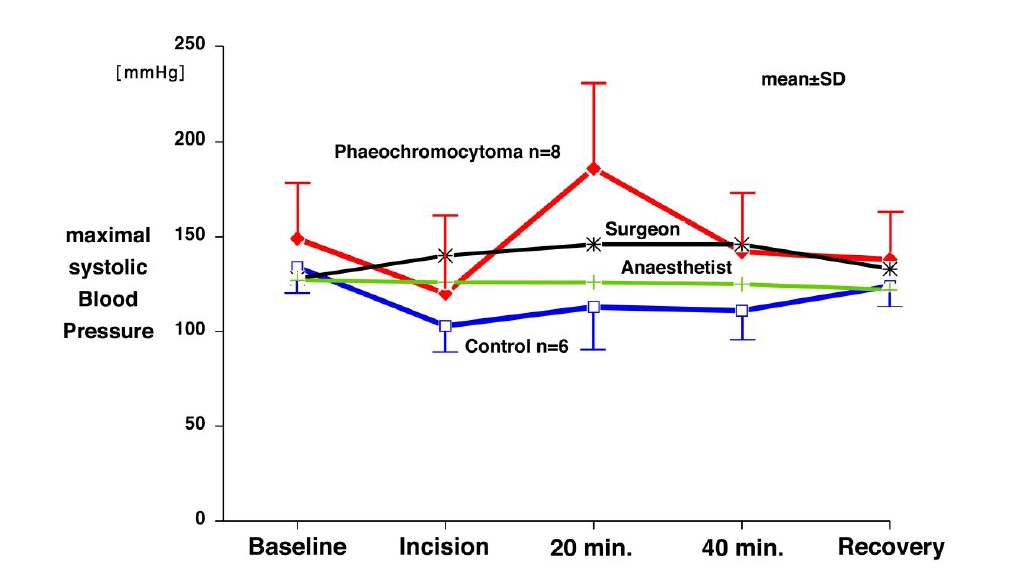
Figure 1: Maximum systolic blood pressure in patients with phaeochromocytoma, incidentaloma, a surgeon and an anesthetist at rest (Baseline), incision, after 20 minutes-, 40 minutes and in recovery room (mmHg; mean ± SD). red: phaeochromocytoma patients, black: surgeon, green: anesthetist, blue: incidentaloma patients
Heart rate
There were no significant differences in mean maximum heart rate within all study groups. However, the phaeochromocytoma patients had higher values overall and offered a nonsignificant heart rate increase to a maximum of 104 ± 29 bpm. On the contrary, in patients with an incidentaloma their maximum heart rate during anaesthesia was lower than their respective baseline heart rate.
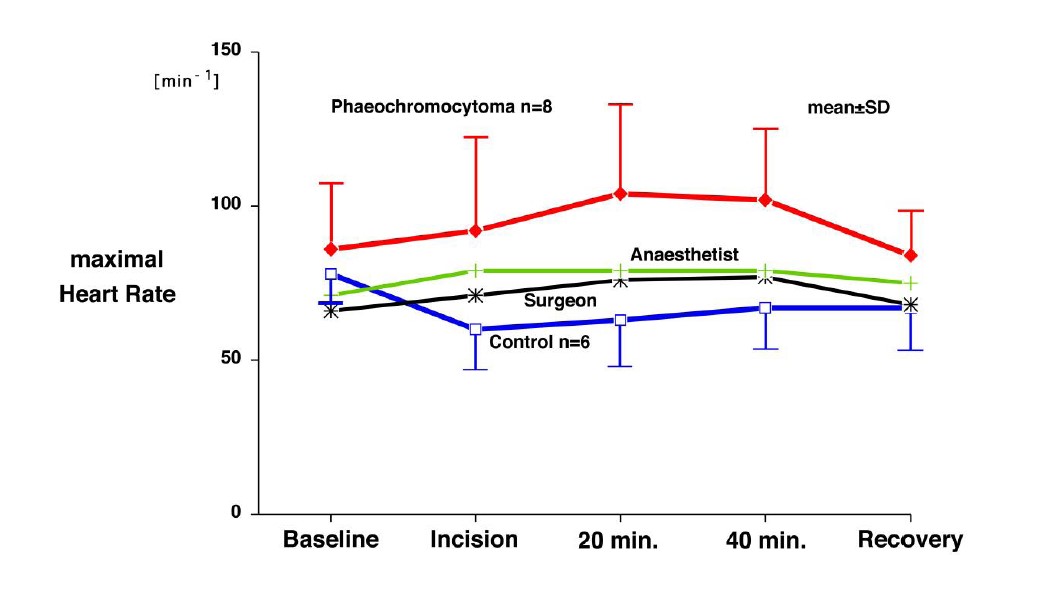
Figure 2: Maximal heard rate in patients with phaeochromocytoma, incidentaloma, a surgeon and an anesthetist at rest (Baseline), incision, after 20 minutes-, 40 minutes and in recovery room (mmHg; mean ± SD). red: pheochromocytoma patients, black: anesthetist, green: surgeon, blue: incidentaloma patients
Metanephrine
There was a significant increase in metanephrine concentration in phaeochromocytoma patients and the surgeon (p = 0.0116). However, the maximum metanephrine concentration was 25-fold higher in the phaeochromocytoma patients than in the surgeon, 40-fold higher than in the anesthetist, and 42-fold higher than in incidentaloma patients. After this excessive increase, metanephrine concentration dropped dramatically in the phaeochromocytoma patients after adrenalectomy. After adrenalectomy metanephrine concentration in the phaeochromocytoma patients were about 3-fold lower compared to the baseline metanephrine concentration but without hemodynamic instability. Because of the extreme range and the large interindividual variations of the maximal metanephrine concentration within the group of phaeochromocytoma patients (maximum: 2530 ± 3391 ng/l), the increases were set in percent to the respective baseline for comparison of the metanephrine concentrations (figure 3).These extreme fluctuations in maximum metanephrine concentration were not present in the control patients and the anesthetist (maximum: control-patients 60 ± 25 ng/l; anesthetist 64 ± 16) ng/l). The surgeon's metanephrine concentration also increased significantly, but several times less (25 fold), and was only just twice as high compared to baseline. Postoperatively, metanephrine concentration remained at slightly elevated levels on average (122% of baseline). Although the control patients showed an increase in metanephrine concentration, this was not significant. Postoperatively, they showed a slightly increased metanephrine concentration compared to baseline. (117 % of baseline). The anesthetist showed an almost linear course of the metanephrine concentration.
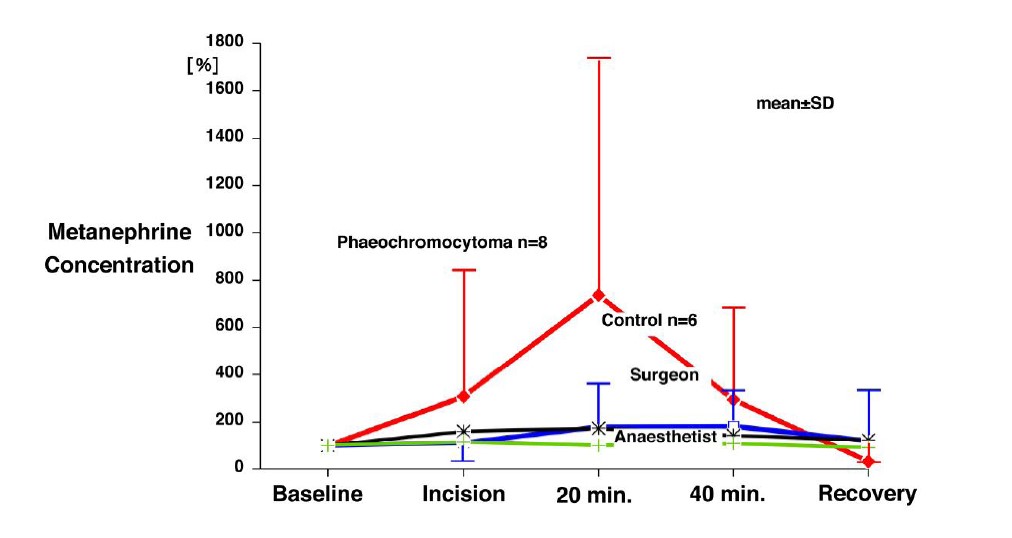
Figure 3: Metanephrin concentration in patients with phaeochromocytoma, incidentaloma, surgeon and anesthetist at rest (Baseline), incision, after 20 minutes-, 40 minutes and in recovery room (ng/l; mean ± SD). Changes in metanephrine plasma concentrations are expressed as a percentage of the respective baseline (100%). Red: phaeochromocytoma patients, green: anaesthetist, black: surgeon, blue: incidentaloma patients
Normetanephrine
There was a significant increase in normetanephrine concentration in the phaeochromocytoma patients (P = 0.0001) and the incidentaloma patients (p = 0.0285). However, the maximum normetanephrine concentration was 18-fold higher in the phaeochromocytoma patients than in the surgeon and 26-fold higher than in the anesthetist and incidentaloma patients. After this excessive increase (at the 20-minute time point), normetanephrine concentration in the phaeochromocytoma patients dropped dramatically after adrenalectomy and, on average, were more than 3-fold lower postoperatively than preoperatively. This drastic decrease in catecholamine concentration was not accompanied by haemodynamic instability.
The surgeon's normetanephrine concentration also showed a significant increase, as did the metanephrine concentration, but also appeared attenuated by a multiple (18-fold). In contrast to the surgeon's metanephrine concentration, the normetanephrine concentration remained at an average decreased level postoperatively (86% of baseline). In the anaesthetist, no significant increase in normetanephrine concentration could be detected. Although the range of normetanephrine concentration was smaller compared to metanephrine concentration within the group of phaeochromocytoma patients (NMN: 1735 ± 1210 ng/l vs. MN: 2530 ± 3391 ng/l), massive variations of maximal normetanephrine concentration were also presented. In order to show these extreme interindividual differences of the maximum normetanephrine concentration within the group of phaeochromocytoma patients more clearly, figures 4 shows the increase of the normetanephrine concentration in percent compared to the respective baseline.
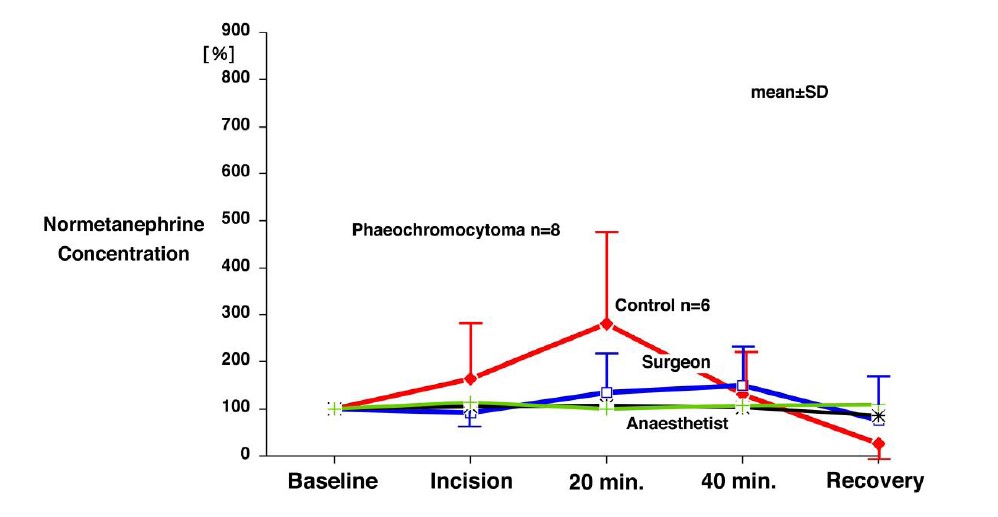
Figure 4: Normetanephrine concentration in patients with phaeochromocytoma, incidentaloma, surgeon and anesthetist at rest (Baseline), incision, after 20 minutes-, 40 minutes and in recovery room (ng/l; mean ± SD). Changes in normetanephrine plasma concentrations are expressed as a percentage of the respective baseline (100%). Red: phaeochromocytoma patients, green: anaesthetist, black: surgeon, blue: incidentaloma patients
Discussion
Despite the medical progress of the last years and decades, without surgical removal of the tumour phaeochromocytoma is still a potentially fatal disease. Therefore, surgery is still the therapy of choice for phaeochromocytoma or paraganglioma. Historically, surgery for catecholamine producing tumours has been burdened by a high rate of morbidity and mortality. Excessive catecholamine release, due to intraoperative tumour manipulation has been made responsible for this high rates.3 11-12 However, during the last three decades mortality has decreased significantly and it is unclear, how catecholamine release correlated with morbidity and mortality. A large international study on the outcome of phaeochromocytoma surgery suggests that hypotension, due to alpha-receptor blockade or catecholamine withdrawal also contributes to the outcome.10 The meaning of perioperative catecholamine concentrations and how these concentrations compare to physiological stress, is unclear.
Up to date, no study has compared catecholamine releases in phaeochromocytoma patients and catecholamine releases in control patients undergoing the same type of surgery and normal subjects exposed to physiological stress. Therefore, we evaluated plasma catecholamine concentrations in all three groups.
Moreover, previous studies had focused on the short-lived catecholamines epinephrine and norepinephrine themselves rather than their more stable plasma catecholamine metabolites normetanephrine and metanephrine, which are recommended to be measured by the current guideline. 8
Catecholamine concentrations during physiological vs. pathophysiological stress in physicians and phaeochromocytoma patients
Intraoperatively, there was a significant increase in normetanephrine and metanephrine levels in the phaeochromocytoma patients. The normetanephrine concentrations exceeded the values of the physicians by more than 18 - 26 times, the metanephrine concentrations even by 25 - 40 times. In addition, the group of phaeochromocytoma patients showed extreme interindividual differences with a maximum increase of the metanephrine concentration between 198-1465% and for normetanephrine between 110-1189% compared to the respective baselines (100%).
In this study, a significant increase in catecholamine metabolite concentration compared to the baseline was also demonstrated for the surgeon, despite the several times lower catecholamine release of the physicians. Whereas this was not the case for the anaesthetist. It is noteworthy, that a similar intraoperative dynamic of the catecholamine metabolite concentration of the surgeon increased in the middle of surgery. This suggests that the surgeon was exposed to significantly higher stress intraoperatively than the anaesthetist and thus substantiates the interindividual difference on stressors. The highest increase could be seen at the 20-minute time point, which represents the most critical part of surgery (tumour preparation and manipulation). Despite the significant increase in catecholamine metabolite concentration in the surgeon, there was only a maximum increase of less than 100% from baseline. These results demonstrate that physiologic stress does not lead to catecholamine concentrations some where close to the excessive catecholamine releases that occur in an autonomous catecholamine-producing tumour.
Catecholamine concentrations during perioperative stress in phaeochromocytoma and incidentaloma patients
Intraoperatively, there was also an increase in normetanephrine and metanephrine concentrations in the incidentaloma patients (control group), but only with significant changes in normetanephrine. The increase in catecholamines in the control group thus allows conclusions to be drawn about intraoperative stress caused by the surgical stimulus. However, this catecholamine increase did not result in arterial hypertension and tachycardia. Most likely, catecholamine concentration increased in control patients as a response to the vasodilation and circulatory suppression by anaesthetics. 13 Thus, the assumption that tumour manipulation of the adrenal gland alone leads to liberation of catecholamines in non-phaeochromocytoma patients has been refuted by this study. 3
Haemodynamics and catecholamine concentrations during physiological and pathophysiological stress
For phaeochromocytoma patients, it seems that the excessive catecholamine metabolite increase as well as the excessive catecholamine metabolite decrease after tumour extirpation were not reflected by the excessive haemodynamic responses. In particular, despite very low postoperative catecholamine concentrations, haemodynamic circulatory stabilization by vasopressor application was not necessary.
This study thereby supports the assumption that an altered physiological circulatory regulation can be assumed in patients with phaeochromocytoma. As a reaction of excessive catecholamine flooding, a desensitization or reduction of adrenoreceptors can be assumed. 11 14-15
However, in addition to the known research findings, this work also suggests that other unknown mechanisms of blood pressure regulation have to be discussed and this should initiate further research.
Changes in perioperative management
Over the last decade many aspects of the perioperative management have changed. These changes include improvements in surgery, anaesthesia, monitoring and intraoperative haemodynamic management. Moreover, major improvements in diagnosing catecholamine producing tumours and their exact localization has markedly contributed to improve the outcome in these patients.
Thus, the rate of complications perioperative mortality decreased from 20-45% in the second half of the last century, 4-5 over 3% in the last decade. 6-9 to finally, the largest and most recent study of over 1800 phaeochromocytoma and paraganglioma patients. This international study showed a mortality rate of 0,3-0,5 %. Interestingly, this study showed no advantage for the use of -receptor blockers in mortality, but an significantly lower morbidity rate.10 This again suggests that the use of -receptor blockade cannot be considered the sole criterion for enormously improved perioperative outcome.
Although excessive plasma catecholamine concentrations can be found in phaeochromocytoma patients far out of the range found in humans under physiological stress like in surgical stress (control patients) or in stressful situations (physicians during phaeochromocytoma surgery), the haemodynamic response is still controllable. Interestingly, after acute withdrawl of the catecholamines following surgery of the tumours, alternative mechanisms maintain physiological haemodynamic conditions.
Author’s Contribution
H. G.: Anaesthetist, who performed the anaesthesia, study design, data acquisition, data analysis and interpretation, writing of the first draft of the manuscript
L.S.: Data acquisition, data analysis and interpretation, writing of the manuscript
V.B.: Patient management, data acquisition
P. F. A.: Surgeon, who performed the surgery, patient recruitment, study design, data acquisition and interpretation
M. K. W.: Surgeon, who performed the surgery, patient recruitment, study design, data acquisition and interpretation
Article Details
The Medical Research Archives grants authors the right to publish and reproduce the unrevised contribution in whole or in part at any time and in any form for any scholarly non-commercial purpose with the condition that all publications of the contribution include a full citation to the journal as published by the Medical Research Archives.
References
2. Neumann HP Young WF, Eng C. Pheochromocytoma and paraganglioma. N Engl J Med. 2019; 381: 552-65
3. Neumann HP, Young WF, Krauss T, Bayley JP, Schiavi F, Opocher G, et al.. 65 years of the double helix: Genetics informs precision practice in the diagnosis and management of pheochromocytoma. Endocr Relat Cancer. 2018; 25: T201-T219
4. Thompson JE, Arrowod JG. Pheochromocytoma: surgical and anesthetic management. Anesthesiology. 1954; 15(6): 658–665
5. Ross EJ, Prichard BN, Kaufman L, Robertson AI, Harries BJ. Preoperative and operative management of patients with pheochromocytoma. Br Med J. 1967; 1(5534), 191–198
6. Toniato A, Boschin IM, Opocher G, Guolo A, Pelizzo M, Mantero F. Is the laparoscopic adrenalectomy for pheochromocytoma the best treatment? Surgery. 2007; 141(6): 723–727
7. Kercher KW, Novitsky YW, Park A, Matthews BD, Litwin DE, Heniford BT. Laparoscopic curative resection of pheochromocytomas. Ann Surg. 2005; 241(6): 919–926
8. Lenders JW, Duh QY, Eisenhofer G, Gimenez-Roqueplo AP, Grebe SK, Murad MH, et al.. Endocrine Society. Pheochromocytoma and paraganglioma: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2014; 99(6): 1915-1942
9. Plouin PF, Gimenez-Roqueplo AP. Pheochromocytomas and secreting paragangliomas. Orphanet J Rare Dis. 2006; 1: 49
10. Groeben, H., Walz, M. K., Nottebaum, B. J., Alesina, P. F., Greenwald, A., Schumann, R, et al.. International multicentre review of perioperative management and outcome for catecholamine-producing tumours. Br J Surg 2020; 107(2): 170-178
11. Zelinka T, Pacák K, Widimský J Jr. Characteristics of blood pressure in pheochromocytoma. Ann N Y Acad Sci. 2006; 1073: 86-93
12. Bravo EL, Tarazi RC, Gifford RW, Stewart BH. Circulating and urinary catecholamines in pheochromocytoma. Diagnostic and pathophysiologic implications. N Engl J Med. 1979; 301(13): 682-686
13. Dahaba AA, Prax N, Gaube W, Gries M, Rehak PH, Metzler H. Haemodynamic and catecholamine stress responses to the Laryngeal Tube-Suction Airway and the Proseal Laryngeal Mask Airway. Anaesthesia. 2006; 61(4): 330-334
14. Spiss CK, Maze M. [Adrenoreceptors]. Anaesthesist. 1985; 34(1): 1-10
15. Bravo E, Fouad-Tarazi F, Rossi G, Imamura M, Lin WW, Madkour MA, et al.. A reevaluation of the hemodynamics of pheochromocytoma. Hypertension. 1990; 15(2): 128-131